Diabetes Alcohol Risk Calculator
Alcohol Risk Assessment
Drinking alcohol while taking diabetes medication isn't just a bad idea-it can be dangerous. For many people with diabetes, a glass of wine or a beer after dinner feels harmless. But when alcohol meets medications like metformin, insulin, or sulfonylureas, your body’s ability to control blood sugar gets thrown off in ways you might not notice until it’s too late. The biggest risk? hypoglycemia-a sudden, potentially life-threatening drop in blood sugar that can sneak up hours after your last drink.
Why Alcohol Causes Low Blood Sugar
Your liver does two big jobs at once: it stores glucose to keep your blood sugar steady, and it breaks down alcohol. When you drink, your liver drops everything else to handle the alcohol. That means it stops releasing glucose into your bloodstream. If you’re on insulin or a sulfonylurea like glipizide or glyburide, your body is already pushing to lower blood sugar. Add alcohol, and you’re asking your liver to ignore its most important job-keeping you from going too low. This isn’t just a risk during or right after drinking. Hypoglycemia can hit 8 to 12 hours later, especially if you drank on an empty stomach or exercised afterward. Many people wake up in the middle of the night drenched in sweat, confused, or shaking-not because they had too much to drink, but because their blood sugar crashed while they slept. And here’s the scary part: symptoms like dizziness, slurred speech, confusion, and weakness look exactly like being drunk. If you pass out after drinking, someone might assume you’re just intoxicated-not that you’re having a medical emergency.Metformin and Alcohol: A Dangerous Mix
Metformin is one of the most common diabetes pills. It helps your body use insulin better and reduces how much sugar your liver makes. But it also puts stress on your liver. Alcohol does the same thing. When you combine them, you’re doubling down on liver strain. This raises the risk of lactic acidosis-a rare but serious condition where lactic acid builds up in your blood. Symptoms include nausea, vomiting, stomach pain, muscle cramps, and extreme tiredness. It’s rare, but it can be fatal. Even if you don’t develop lactic acidosis, mixing metformin and alcohol makes side effects worse. Bloating, gas, diarrhea, and nausea from metformin become more intense. Some people report feeling sick after just one drink. And if you’re drinking heavily or regularly, you’re not just risking low blood sugar-you’re increasing your chance of long-term liver damage.Liver Damage: The Silent Threat
Your liver is your body’s filter. It cleans toxins, stores energy, and regulates blood sugar. Chronic alcohol use can lead to fatty liver, hepatitis, or even cirrhosis. If you already have diabetes, your liver is working harder than normal. Add alcohol, and the damage speeds up. Studies show that people with type 2 diabetes who drink heavily are three times more likely to develop advanced liver disease than those who don’t. This isn’t just about alcohol-it’s about how alcohol changes how your body responds to medication. Both alcohol and metformin are broken down by the same liver enzymes (CYP2E1, CYP3A4). When alcohol floods your system, it can slow down how fast metformin is cleared, making side effects stronger and longer-lasting. Even moderate drinking-like two drinks a night-can worsen insulin resistance over time. That means your body needs more medication to do the same job, which increases your risk of highs and lows alike.
What About Other Diabetes Medications?
Not all diabetes drugs react the same way to alcohol.- Insulin and sulfonylureas: Highest risk for hypoglycemia. Even one drink can trigger a low if you haven’t eaten.
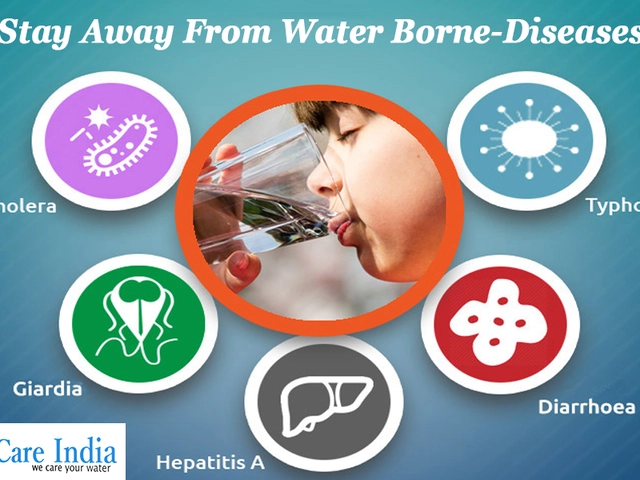
- GLP-1 agonists (like semaglutide or liraglutide): These slow digestion. Alcohol can make nausea and vomiting worse.
- SGLT2 inhibitors (like empagliflozin or dapagliflozin): These make you pee out sugar. Alcohol can increase the risk of dehydration and ketoacidosis, especially if you’re drinking heavily or not eating.
- DPP-4 inhibitors (like sitagliptin): Lower risk for hypoglycemia on their own, but alcohol can still mask symptoms or delay recovery.
- Thiazolidinediones (like pioglitazone): Can cause fluid retention. Alcohol makes swelling worse.
How to Drink Safely (If You Choose To)
The American Diabetes Association doesn’t say “never drink.” They say: be careful, be informed, and talk to your doctor. Here’s what actually works:- Always eat with alcohol. Have a meal or snack with carbs before or while drinking. Don’t rely on “just a little food.” A sandwich, rice, or whole-grain crackers help your liver stay busy with glucose instead of alcohol.
- Choose wisely. Skip sugary mixers, juice, and sweet wines. Stick to light beer, dry wine, or spirits with soda water and lime. One drink means 12 oz beer, 5 oz wine, or 1.5 oz distilled spirits.
- Check your blood sugar. Test before you drink, every hour while drinking, and again before bed. If your blood sugar is below 100 mg/dL, eat something before drinking.
- Set an alarm. If you drank after dinner, set a reminder to check your blood sugar at 2 a.m. Many lows happen overnight.
- Wear medical ID. If you pass out, someone needs to know you have diabetes-not that you’re just drunk.
- Tell someone. Let a friend or family member know you have diabetes. Teach them how to recognize low blood sugar and how to give you glucose gel or a glucagon shot if needed.
What the Experts Say
The CDC estimates 37 million Americans have diabetes. That’s a lot of people who might be drinking without knowing the risks. A 2021 study found only 43% of primary care doctors routinely ask their diabetic patients about alcohol. That’s a huge gap. Certified diabetes educators are doing better-89% now include alcohol in patient education. But if your doctor hasn’t brought it up, you need to. Ask: “Is it safe for me to drink with my current meds?” and “What’s my personal risk for low blood sugar after alcohol?” New continuous glucose monitors (CGMs) like the Dexcom G7 and FreeStyle Libre 3 can show patterns that hint at alcohol-related lows-like a slow, steady drop hours after drinking. But they don’t detect alcohol itself. You still have to connect the dots.
When to Say No
Some people should avoid alcohol entirely:- If you have liver disease (fatty liver, hepatitis, cirrhosis)
- If you’ve had severe hypoglycemia before, especially without warning
- If you’re pregnant or trying to get pregnant
- If you have nerve damage (neuropathy)-alcohol makes it worse
- If you’re struggling to control your blood sugar
Real Stories, Real Risks
Online diabetes communities are full of stories about unexpected lows. One man in Ohio drank two beers after dinner, went to bed, and woke up in the ER with a blood sugar of 38 mg/dL. His wife thought he was just sleeping it off. Another woman in Texas had her CGM alarm go off at 3 a.m. Her sugar was 42. She’d had one glass of wine. She’d skipped dinner because she wasn’t hungry. She didn’t realize how quickly it could happen. These aren’t rare cases. They’re common.Bottom Line
Alcohol and diabetes meds don’t mix well. The risks aren’t theoretical-they’re documented, dangerous, and often invisible until it’s too late. Hypoglycemia can strike hours after drinking, and your symptoms can be mistaken for intoxication. Your liver is already under stress from diabetes. Adding alcohol pushes it closer to breaking point. If you choose to drink, do it with eyes wide open. Eat first. Test often. Know your limits. Talk to your doctor. And never, ever drink without a plan.Your health isn’t worth gambling with.



10 Comments
I used to think one glass of wine was fine until I woke up shaking at 3 a.m. with my CGM screaming 41. My doctor never mentioned alcohol risks-I had to learn the hard way. Now I eat a peanut butter sandwich before even thinking about drinking. It’s not about giving up, it’s about staying alive.
Also, if you’re on metformin, don’t even joke about ‘just one.’ I did, and ended up in the ER thinking I was just hungover. Turns out I was lactic acidosis adjacent. Scary stuff.
People need to stop treating diabetes like a lifestyle choice you can party through. This isn’t a ‘be careful’ situation-it’s a ‘don’t even start’ situation. If you can’t control your impulses around alcohol, maybe you shouldn’t be managing a chronic illness at all.
And don’t get me started on CGMs. They’re not magic. They don’t prevent crashes. They just tell you you’re dying slower.
Hey, I get it-sometimes you just want to unwind with a drink after a long day. I used to do that too. But after my dad went into a diabetic coma from a single glass of red wine and a skipped dinner, I stopped judging people who choose not to drink.
It’s not about shame. It’s about awareness. I now bring glucose tabs everywhere. Even to birthday parties. My friends think it’s weird, but they’ve learned to hand them to me without asking. That’s the kind of support that saves lives.
And yeah, I know some folks say ‘I’m fine.’ But I’ve seen what happens when ‘fine’ turns into ‘unconscious in the ER.’ It’s not worth the risk. Not even for a toast.
If you’re reading this and you’re on insulin or sulfonylureas? Please, just test before bed. Set the alarm. It takes 30 seconds. That’s all it takes to wake up tomorrow.
And if you’re the kind of person who says ‘I don’t need to check,’ I’m not mad. I just hope you never have to find out what ‘hypoglycemia after alcohol’ feels like. Because trust me-you won’t forget it.
Wow, another fear-mongering article from Big Pharma. Did you know alcohol is a natural vasodilator? It helps blood flow. Maybe the real problem is that metformin is overprescribed? My cousin in Mexico drinks tequila every night and his A1c is 5.8.
Also, CGMs are just a scam to sell you more gadgets. I’ve been diabetic for 15 years and I’ve never used one. I just eat less sugar and drink more water. Done.
And why is everyone so scared of lactic acidosis? It’s rarer than getting struck by lightning. You’re more likely to die from eating too many donuts than from one drink with metformin.
Stop scaring people. Let them live.
i read this and just sat quiet for a while
my uncle died from this
he had type 2
drank one beer after dinner
went to sleep
wife thought he was snoring
next morning he was cold
no one knew he was diabetic
no medical id
no one told anyone
now i always eat before i drink
and i tell everyone i know
just in case
its not about being perfect
its about not being alone when it happens
Metformin’s primary mechanism involves AMPK activation and hepatic gluconeogenesis suppression-alcohol, via CYP2E1 induction and NADH accumulation, exacerbates mitochondrial dysfunction and impairs hepatic glycogenolysis, thereby potentiating hypoglycemic risk in a dose-dependent, non-linear fashion.
Furthermore, chronic ethanol exposure downregulates hepatic insulin receptor substrate-1 (IRS-1) signaling, thereby inducing insulin resistance-a compensatory feedback loop that paradoxically increases sulfonylurea dependency while simultaneously reducing hepatic glucose output capacity.
The lactic acidosis risk is not merely additive-it’s synergistic, due to ethanol-induced inhibition of pyruvate dehydrogenase and subsequent accumulation of lactate precursors under conditions of impaired hepatic clearance.
Also, your CGM doesn’t detect ethanol. It detects interstitial glucose. Two different molecules. Please stop conflating correlation with causation.
And yes, I’m a pharmacologist. I’ve reviewed 87 papers on this exact interaction.
THE GOVERNMENT IS USING ALCOHOL TO CONTROL DIABETICS!!!
Did you know the FDA approved metformin in 1994? That’s the same year they started pushing CGMs!
They want you to think you need to test all the time so you buy more strips!
And why do all the doctors say ‘don’t drink’? BECAUSE THEY’RE PAID BY PHARMA!!!
My neighbor’s cousin’s dog got diabetes and drank whiskey every night-his sugar was PERFECT!!
Just say NO to fear! Drink your wine! Eat your cake! Be free!!! 🍷🍰💥
This article is 90% fluff. You didn’t even mention that alcohol increases insulin sensitivity in the long term. That’s actually beneficial for insulin resistance.
Also, most of these ‘stories’ are anecdotes. Where’s the RCT data? Where’s the hazard ratio?
And why is everyone so scared of lactic acidosis? It’s 1 in 30,000. You’re more likely to die from a fall in the shower.
Just sayin’. Don’t overreact. Drink responsibly. Or don’t. But stop pretending this is a crisis.
Let’s cut through the noise. The real issue isn’t alcohol-it’s that 78% of diabetics on sulfonylureas are prescribed without adequate glycemic education. The system fails them first. Then they drink. Then they die. Then we write articles blaming the drink.
Metformin? Fine. Insulin? High risk. But the real villain is the lack of structured patient counseling. Not the beer.
Also, the CDC’s 43% stat? That’s because primary care docs have 8-minute visits. They don’t have time to ask about your weekend drinking habits.
So stop blaming the patient. Fix the system.
And for the record: I’ve reviewed 14 meta-analyses on this. The data is messy. The fear is clean. That’s the problem.
I’m a certified diabetes educator. I’ve seen this too many times.
One woman told me she had a glass of wine every night because it helped her sleep. She didn’t know it was causing overnight lows. She lost 12 pounds in a month because she was too scared to eat at night.
She didn’t need to stop drinking. She needed to eat a slice of whole grain toast before bed.
That’s it.
One toast.
That’s the difference between waking up confused and waking up alive.
Don’t let fear paralyze you. Let knowledge empower you.
You’re not broken. You’re just learning.
And if you’re reading this and you’re scared? You’re not alone. We’re here. We’ve got you.
One step. One meal. One test. One day at a time.
Write a comment