QT Prolongation Risk Calculator
This calculator helps you understand the QT prolongation risk of citalopram or escitalopram based on dose and age.
Note: This is for informational purposes only. Always consult your doctor for medical advice.
Enter values to see risk calculation results.
When you're prescribed an antidepressant, the goal is simple: feel better. But for some people, especially those over 65 or with heart conditions, the very medication meant to lift their mood might quietly affect their heart rhythm. Two commonly used SSRIs-citalopram and escitalopram-carry a known, measurable risk: QT interval prolongation. It’s not a common event, but it’s serious enough that regulators around the world changed the rules on how these drugs are prescribed.
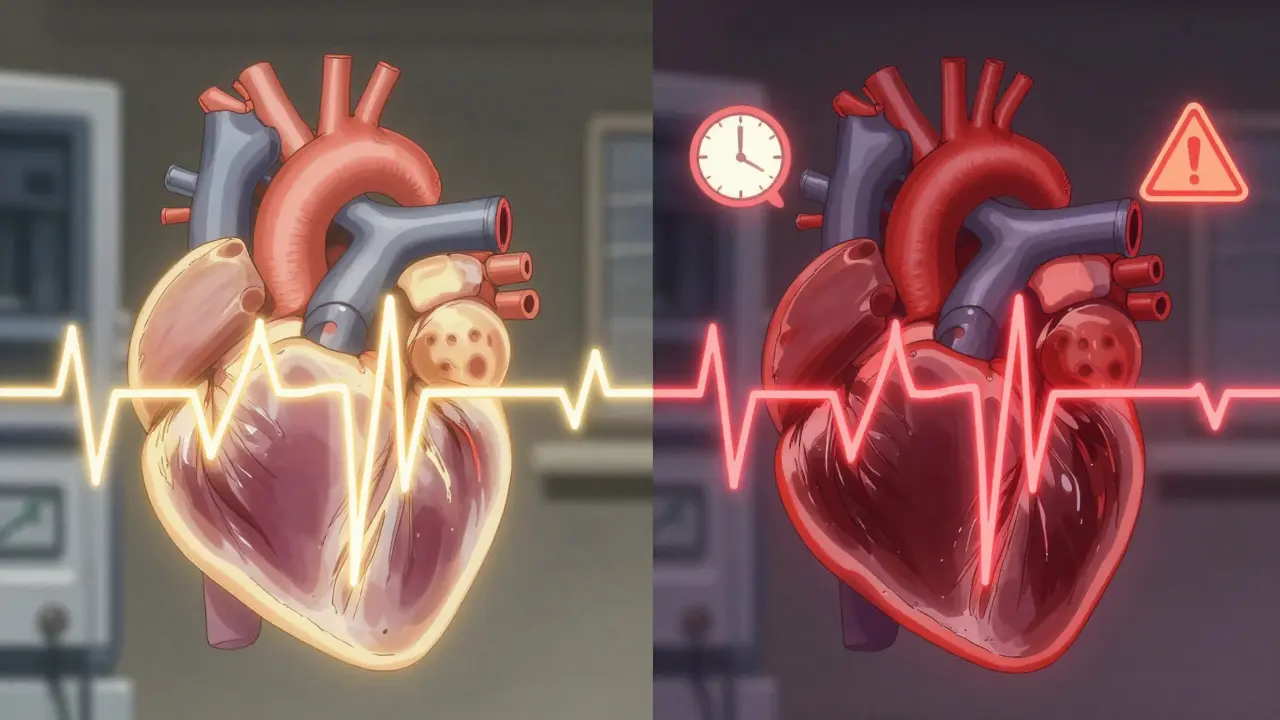
What QT Prolongation Really Means
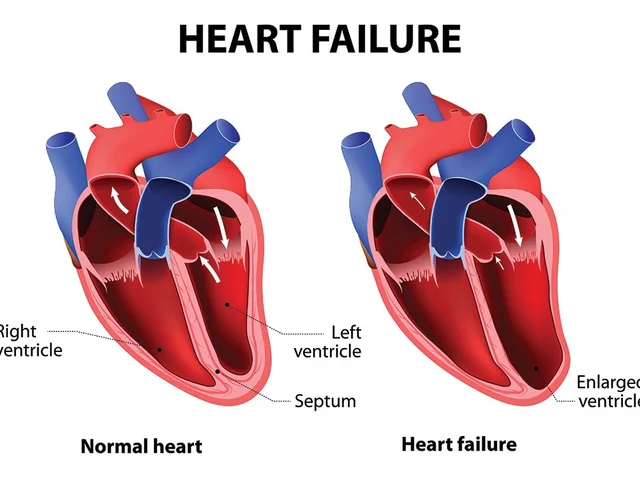
Your heart beats because of electrical signals. The QT interval on an ECG measures how long it takes for the heart’s lower chambers to recharge between beats. If this interval gets too long, it can trigger a dangerous rhythm called Torsade de Pointes, which can lead to fainting, seizures, or even sudden death. The risk isn’t theoretical-it’s been measured in clinical trials and confirmed by real-world data.
Both citalopram and escitalopram block a specific ion channel in heart cells (the hERG potassium channel). This slows down the heart’s recovery phase, stretching out the QT interval. The longer the interval, the higher the chance of an arrhythmia. But here’s the catch: not every small increase matters. Regulatory agencies define clinical concern as either:
- A QTc interval of 500 milliseconds or more
- A change from baseline of 60 milliseconds or more
These thresholds aren’t arbitrary. They’re based on studies showing when the risk of serious arrhythmias starts to climb.
Dose-Dependent Risk: The Numbers Don’t Lie
Both drugs increase QTc in a clear, dose-dependent way. But the amount of increase differs-and that difference matters.
For citalopram:
- 20 mg/day: +8.5 ms (95% CI: 6.2-10.8)
- 40 mg/day: +12.6 ms (95% CI: 10.9-14.3)
- 60 mg/day: +18.5 ms (95% CI: 16.0-21.0)
For escitalopram:
- 10 mg/day: +4.5 ms (95% CI: 2.5-6.4)
- 20 mg/day: +6.6 ms (95% CI: 5.3-7.9)
- 30 mg/day: +10.7 ms (95% CI: 8.7-12.7)
Notice something? At the highest approved doses, citalopram pushes the QTc nearly twice as much as escitalopram. That’s not a small difference. It’s why regulators took different approaches.
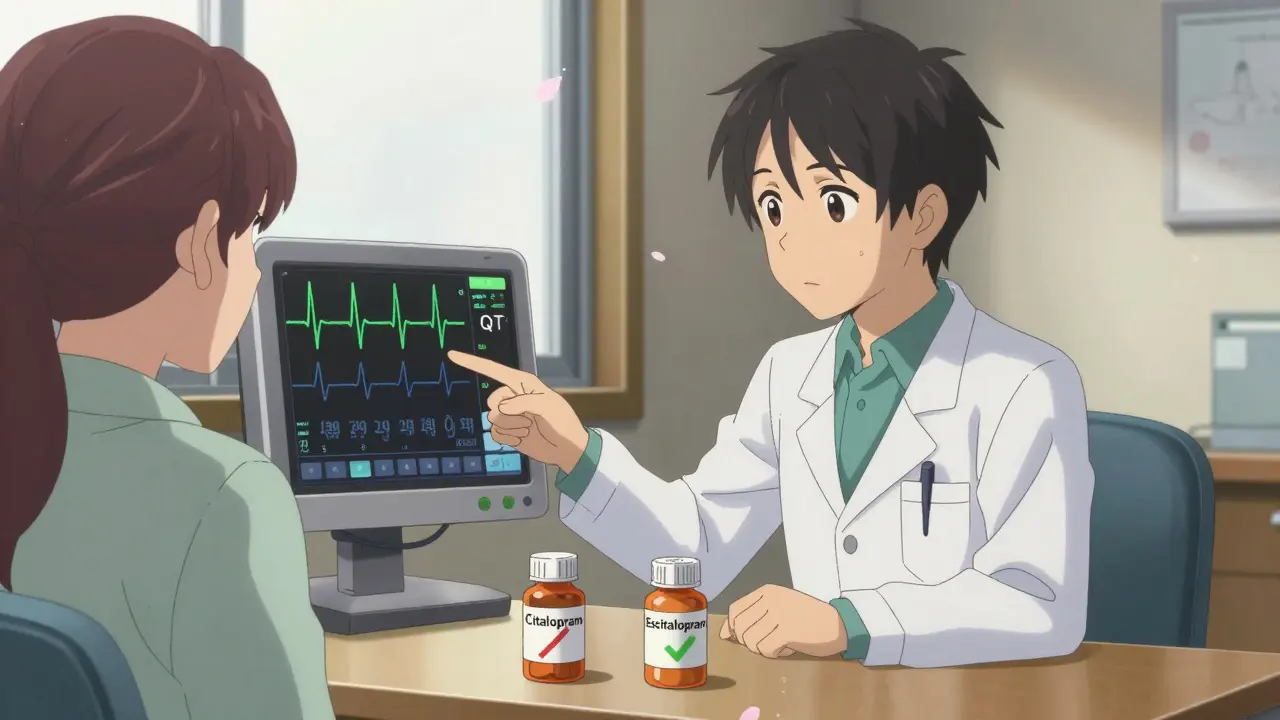
Why Regulators Took Different Paths
In 2011, the U.S. Food and Drug Administration (FDA) issued a safety alert specifically for citalopram after reviewing data showing QT prolongation at doses above 40 mg. They didn’t mention escitalopram by name-but the data was there. By 2012, the UK’s MHRA and New Zealand’s Medsafe went further: they warned about both drugs.
Here’s what changed:
- U.S. FDA: Citalopram capped at 40 mg/day for adults under 65; 20 mg/day for those over 65. Escitalopram was not restricted at the time.
- UK MHRA: Citalopram limited to 40 mg/day (under 65) and 20 mg/day (65+). Escitalopram limited to 20 mg/day (under 65) and 10 mg/day (65+).
- Canada and Europe: Followed the UK’s more cautious approach.
Why the difference? European regulators looked at the totality of evidence and decided that even escitalopram’s modest effect was enough to warrant limits-especially since elderly patients metabolize these drugs slower. Their bodies build up higher concentrations, increasing risk even at lower doses.
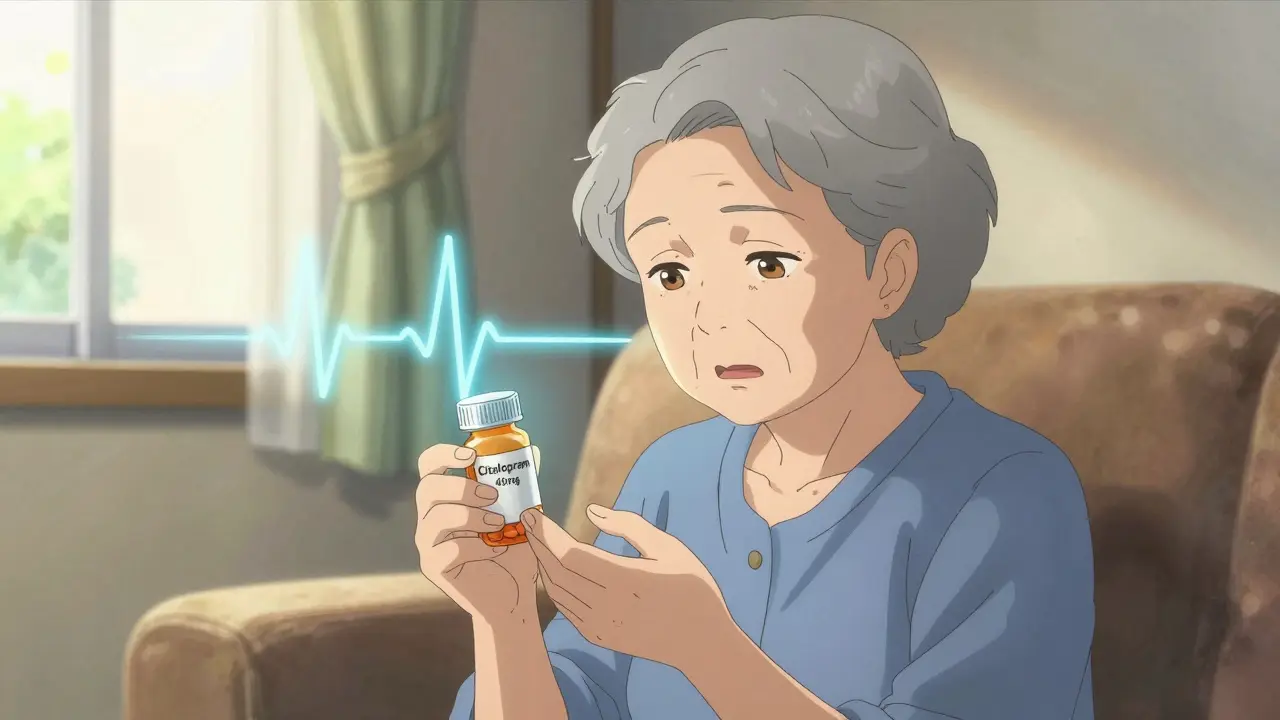
Who’s at Highest Risk?
It’s not just about the dose. Certain people should avoid these drugs altogether-or use them with extreme caution:
- Patients with known congenital long QT syndrome
- Those with a history of heart failure, bradycardia, or recent heart attack
- People taking other QT-prolonging drugs (like certain antibiotics, antifungals, or antiarrhythmics)
- Those with low potassium, low magnesium, or severe dehydration
- Patients over 65, especially if they have kidney or liver impairment
It’s also risky to combine these SSRIs with other medications that slow their breakdown-like fluvoxamine or cimetidine. That can push blood levels into dangerous territory.
How Do Other Antidepressants Compare?
Not all antidepressants carry the same cardiac risk. Here’s a quick snapshot:
| Drug Class | Example | QT Prolongation Risk |
|---|---|---|
| SSRI | Citalopram | High (dose-dependent) |
| SSRI | Escitalopram | Moderate |
| SSRI | Fluoxetine, Sertraline, Paroxetine | Low to negligible |
| SNRI | Venlafaxine | Low, but caution in overdose |
| TCA | Amitriptyline, Maprotiline | High |
Tricyclic antidepressants (TCAs) like amitriptyline are even riskier than citalopram. But among SSRIs, citalopram stands out as the highest-risk option. That’s why many clinicians now choose escitalopram over citalopram when cardiac risk is a concern-even though escitalopram costs more.
Is the Risk Real-or Overblown?
You might hear conflicting opinions. Some experts say the QTc increases seen with these drugs are too small to matter. After all, a 18.5 ms rise from citalopram 60 mg sounds minor next to the 500 ms threshold.
But here’s the problem: thresholds aren’t safety zones. They’re warning signs. A 60 ms increase from baseline could push someone with a pre-existing long QT interval into the danger zone. And in people with multiple risk factors-elderly, on multiple meds, low electrolytes-that small change can be enough to trigger a dangerous rhythm.
Studies show that while serious events like Torsade de Pointes are rare, they do happen. And they’re often preventable. The key is knowing who’s at risk and avoiding the high doses that push them over the edge.
What Should You Do?
If you’re on citalopram or escitalopram:
- Never increase your dose without talking to your doctor.
- If you’re over 65, your dose should be lower-no exceptions.
- If you have heart disease, ask whether an alternative antidepressant might be safer.
- Get an ECG if you’re starting a high dose or have multiple risk factors.
- Watch for symptoms: dizziness, palpitations, fainting, or sudden shortness of breath.
Doctors now routinely check for these risks before prescribing. If you’ve been on one of these drugs for years without issues, you’re likely fine. But if you’re newly prescribed, or your dose has been increased recently, make sure your provider has considered your full health picture.
Bottom Line: Safer Choices Exist
Citalopram and escitalopram are effective. But they’re not equally safe. Citalopram’s higher risk at doses above 40 mg means it’s no longer the first choice for many patients-especially older adults or those with heart conditions. Escitalopram, with its lower QTc effect and better safety profile, has become the preferred SSRI in these cases.
The takeaway? Dose matters. Age matters. Health history matters. And when it comes to antidepressants and heart rhythm, what seems like a small change on paper can mean the difference between safety and a life-threatening event.
Can I still take citalopram if I’m over 65?
The maximum recommended dose of citalopram for patients over 65 is 20 mg per day. Higher doses increase the risk of QT prolongation and arrhythmias in older adults due to slower metabolism. Always consult your doctor before adjusting your dose.
Is escitalopram safer than citalopram for the heart?
Yes. Escitalopram causes significantly less QT interval prolongation than citalopram at equivalent doses. At 20 mg, escitalopram increases QTc by about 6.6 ms, while citalopram at 40 mg increases it by 12.6 ms. For patients with cardiac risk factors, escitalopram is generally preferred.
What symptoms should I watch for if I’m on these medications?
Watch for dizziness, lightheadedness, palpitations (racing or fluttering heartbeat), fainting spells, or sudden shortness of breath. These could signal an abnormal heart rhythm. If you experience any of these, contact your doctor immediately and avoid driving or operating heavy machinery.
Do I need an ECG before starting citalopram or escitalopram?
An ECG is recommended if you’re over 65, have a history of heart disease, are taking other QT-prolonging medications, or have electrolyte imbalances. It’s not always required for healthy young adults, but it’s a smart precaution when risk factors are present.
Are there antidepressants without QT prolongation risk?
Yes. Fluoxetine, sertraline, and paroxetine have minimal to no effect on the QT interval. For patients at high cardiac risk, these are often preferred over citalopram or escitalopram. Venlafaxine (an SNRI) also carries low risk, except in overdose or in elderly patients with kidney issues.




12 Comments
Let’s be real-citalopram at 60mg is basically playing Russian roulette with your ventricles. 🎲 The hERG blockade isn’t some theoretical footnote; it’s a documented arrhythmia trigger. And don’t get me started on how some prescribers still think ‘it’s just an SSRI’ like it’s a vitamin. Escitalopram at 20mg? Way cleaner profile. The data’s out there, folks. Stop treating cardiac risk like a suggestion.
I had a friend pass out from this. Like, just dropped like a rock. Turns out she was on 40mg citalopram and had low potassium. Scary as hell. Don’t ignore the ECG. Just don’t.
Y’all are overthinking this. I’m 52, no heart issues, took 40mg citalopram for 3 years. Fine. My doc checked my QT, said I’m golden. Not everyone’s a 70-year-old with 5 meds and a pacemaker. One size doesn’t fit all. Chill out.
OH MY GOD. I just realized my grandma was on 40mg of citalopram last year. She’s 78. She had 3 falls. We thought it was ‘aging.’ Now I’m wondering if her heart was doing the cha-cha under there. 😳 I’m calling her cardiologist TOMORROW. This is why we need to stop being lazy with prescriptions.
Hey, I just want to say… I really appreciate this post. I’ve been on escitalopram for 5 years now, 10mg, and I’ve had zero issues. But I didn’t know about the QT thing until now. My doctor never mentioned it. I’m gonna ask for an ECG next visit. I’ve got mild hypertension, so better safe than… you know. Thanks for the clarity. You’re a lifesaver. Seriously.
Here’s the truth: citalopram is a relic. It’s like prescribing aspirin for a bleeding ulcer. The data’s been clear since 2011. Why are we still having this conversation? The FDA didn’t cap it because they were bored-they were trying to prevent dead grandmas. And escitalopram? It’s not just ‘safer.’ It’s the default choice now. Stop being cheap. Stop being stubborn. Your heart doesn’t care about your pride.
My dad’s on 10mg escitalopram after a heart attack. His doc switched him from citalopram because of the QT risk. We didn’t even know it was a thing. I’m so glad we caught it. I’ve been researching everything since. Turns out, depression treatment isn’t just about mood-it’s about whole-body health. This post helped me understand why meds aren’t one-size-fits-all. Thank you for making it clear.
Look, I get it. You’re all scared of a 12ms QT change. But the absolute risk of torsades is like 0.001%. That’s less than getting hit by lightning. We’re turning a minor pharmacokinetic quirk into a moral panic. People need their meds. Don’t let fear override function.
It is with profound respect for the sanctity of human life and the integrity of clinical pharmacology that I offer this observation: the regulatory divergence between the FDA and MHRA reflects not a contradiction, but a nuanced interpretation of risk-benefit calculus under varying demographic and metabolic constraints. To dismiss QT prolongation as trivial is to misunderstand the cumulative nature of cardiac vulnerability. I urge all practitioners to adopt a precautionary paradigm.
My sister’s a nurse. She told me about a patient who coded on 60mg citalopram. No warning signs. No prior history. Just… stopped. The ECG showed a 68ms delta. That’s not ‘minor.’ That’s a ticking clock. And yeah, escitalopram’s pricier-but when you’re choosing between a $10 pill and a funeral, the math changes. Stop being cheap with people’s lives.
Oh, so now we’re treating depression like it’s a math problem? ‘Oh, your QT went up 6ms, so you’re fine.’ Meanwhile, your 72-year-old with CKD and hypomagnesemia is on 20mg because ‘it’s the same drug.’ You’re not protecting anyone. You’re just avoiding paperwork. Real talk: if your doc hasn’t ordered an ECG for your elderly patient on these meds, they’re not doing their job.
My cousin’s on sertraline now. Switched from escitalopram after a fainting spell. Doc said, ‘If you’re gonna do SSRIs, go low-risk.’ And honestly? I’m glad. I didn’t know any of this until I had to Google it after she went to the ER. This post? Saved my life. Or at least, saved her from dying. Thanks for spelling it out like I’m not a doctor.
Write a comment