If you’ve ever felt that burning sensation in your chest after eating, or woke up with a sour taste in your mouth, you’re not alone. About 20% of adults in the U.S. deal with GERD symptoms at least once a week. For many, it’s more than just an uncomfortable meal aftereffect-it’s a daily struggle that disrupts sleep, limits food choices, and wears down quality of life. The good news? Most people can take control of GERD without surgery or lifelong medication. The key is understanding how proton pump inhibitors (PPIs) and lifestyle changes work together-not as alternatives, but as partners.
What Really Happens When You Have GERD?
GERD isn’t just occasional heartburn. It’s when the lower esophageal sphincter (LES), the muscle that acts like a door between your stomach and esophagus, stops working right. Instead of staying closed after food passes through, it opens too often or doesn’t close tightly enough. That lets stomach acid-strong enough to dissolve metal-flow back up into your esophagus. Your stomach lining can handle it. Your esophagus? Not so much. The result? Classic symptoms: heartburn (felt by 90% of people with GERD), regurgitation (that sour or bitter taste), and sometimes a chronic cough, hoarse voice, or even dental erosion from repeated acid exposure. These symptoms usually get worse after eating, when lying down, or bending over. For some, they happen every night. Left untreated, GERD can lead to serious problems. About 10-15% of long-term sufferers develop Barrett’s esophagus, a condition where the cells lining the esophagus change and become precancerous. Others end up with strictures-narrowing of the esophagus that makes swallowing painful or impossible. That’s why managing GERD isn’t just about feeling better today; it’s about protecting your health tomorrow.How PPIs Actually Work (And Why They’re So Popular)
Proton pump inhibitors-like omeprazole (Prilosec), esomeprazole (Nexium), and pantoprazole (Protonix)-are the most powerful acid-reducing drugs available. They don’t just calm down acid production; they shut it off at the source. PPIs block the proton pumps in stomach cells that actually make acid. This cuts acid output by 90-98%, far more than older drugs like H2 blockers (e.g., Pepcid), which only reduce it by 60-70%. That’s why doctors reach for PPIs first when someone has erosive esophagitis (visible damage in the esophagus) or frequent, severe symptoms. Clinical trials show PPIs heal esophagitis in 70-90% of cases within 8 weeks. That’s a huge win compared to H2 blockers, which heal only about half as many. But here’s the catch: PPIs aren’t magic. They take 1-4 hours to start working, and they need to be taken 30-60 minutes before your first meal of the day. Taking them after breakfast? You’re missing the window. They also don’t fix the broken LES-they just reduce the damage it causes.The Hidden Costs of Long-Term PPI Use
Many people stay on PPIs for years, sometimes without ever checking if they still need them. That’s a problem. Studies show that long-term use (over a year) is linked to higher risks of:- Enteric infections like Clostridium difficile (a dangerous gut bug)
- Vitamin B12 deficiency (which can cause fatigue, numbness, and memory issues)
- Magnesium deficiency (leading to muscle cramps, irregular heartbeat)
- Increased risk of hip fractures in older adults (35% higher with 3+ years of use)

Lifestyle Changes: The Forgotten First Line of Defense
The American College of Gastroenterology says lifestyle changes should come before medication-for everyone. And the evidence backs it up. Losing just 5-10% of your body weight can cut GERD symptoms in half. For someone weighing 200 pounds, that’s 10-20 pounds. No surgery. No prescription. Just better habits. Avoid eating within 2-3 hours of bedtime. That simple rule reduces nighttime acid exposure by 40-60%. Why? Gravity helps keep acid down when you’re upright. Lying down? It’s like opening the floodgates. Trigger foods are real. Coffee, tomatoes, alcohol, chocolate, fatty foods, and spicy meals worsen symptoms in 70-80% of people. Cutting them out doesn’t mean you have to eat bland food forever-it means learning what *your* body reacts to. One person might tolerate spicy food fine but can’t touch citrus. Another might be fine with wine but gets heartburn from dark chocolate. A 2022 survey found that 58% of people who tracked their diet and avoided triggers saw moderate to complete symptom control. Coffee elimination helped 73% of users. Spicy food avoidance helped 68%. That’s better than most drugs.Putting It All Together: A Realistic Plan
You don’t have to do everything at once. Start with one change. Pick the easiest one. Maybe it’s not eating after 7 p.m. Or maybe it’s cutting out soda. Track your symptoms for two weeks. Use a free app like RefluxMD to log meals and symptoms. You’ll start seeing patterns. If you’re on a PPI, don’t quit cold turkey. Talk to your doctor about tapering. Try switching to an H2 blocker like famotidine for a few weeks while you make lifestyle changes. Many people find they can go from daily PPIs to once-a-week use-or even stop entirely. Elevating the head of your bed by 6 inches can be a game-changer for nighttime symptoms. You don’t need a fancy wedge pillow-just stack a few bricks under the bedposts at the head end. It’s cheap, effective, and works better than most people expect.When to Consider Surgery or Advanced Options
Most people don’t need surgery. But if you’ve tried PPIs and lifestyle changes for 3-6 months and still have symptoms-or you’re worried about long-term drug use-there are other options. Fundoplication, a surgical procedure that wraps the top of the stomach around the LES, has a 90% success rate at 10 years. It’s invasive, but it fixes the problem at the source. Newer options like the LINX® device-a ring of magnetic beads implanted around the LES-let food pass through but prevent acid from coming back up. About 85% of users report symptom reduction after five years. In 2023, the FDA approved Vonoprazan (Voquezna), the first new type of acid blocker in 30 years. It works faster than PPIs and may have fewer long-term risks. Early trials show it heals esophagitis just as well, if not better.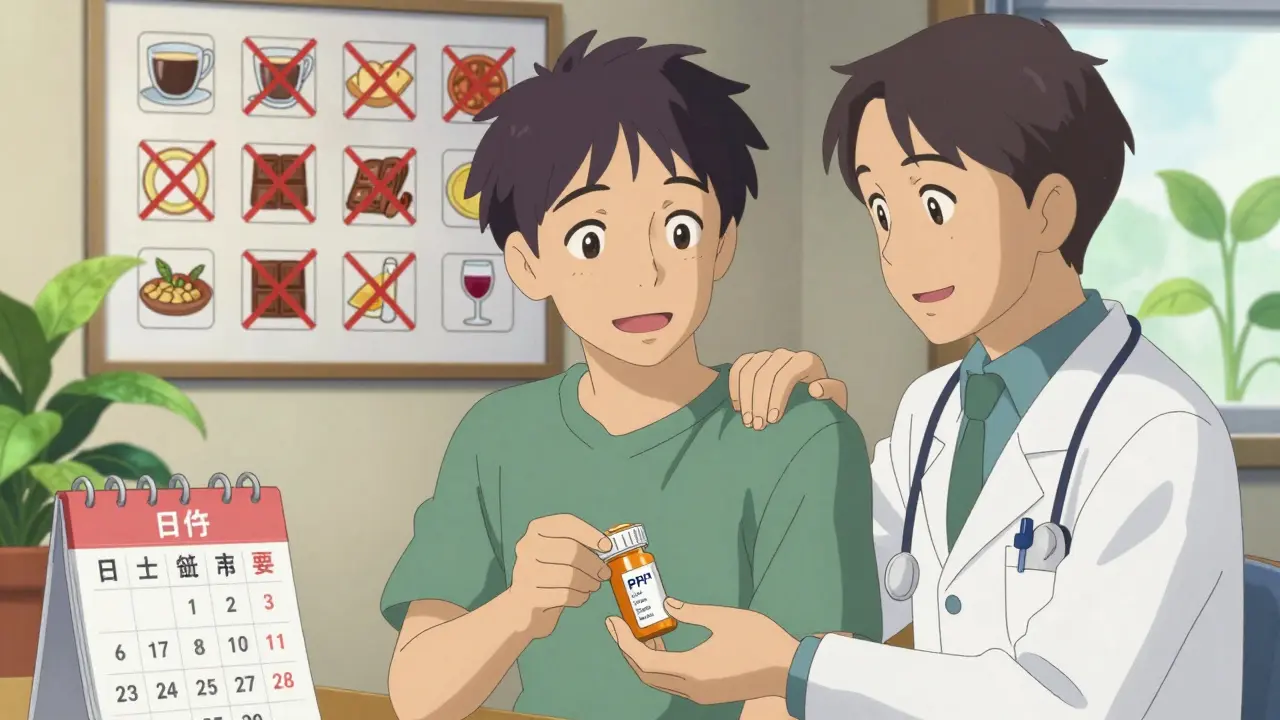
What Success Looks Like
Success isn’t just “no more heartburn.” It’s being able to eat dinner with your family without anxiety. It’s sleeping through the night. It’s not needing to plan your day around bathroom access or antacids. One patient, a 52-year-old teacher from Cardiff, stopped her daily omeprazole after 18 months. She lost 15 pounds, cut out coffee and wine, and started sleeping with her head elevated. Within six weeks, her symptoms were gone. She hasn’t taken a PPI since. Another, a 48-year-old father, tried lifestyle changes for six months. When they weren’t enough, he switched from daily PPIs to on-demand use-only taking them before big meals or stressful days. He now takes a PPI twice a month, not every day. The goal isn’t perfection. It’s control. You don’t have to be a saint with your diet. You just need to be consistent enough to let your body heal.What to Watch Out For
Not all chest pain is GERD. If you have:- Difficulty swallowing
- Unexplained weight loss
- Bloody or black stools
- Chest pain that spreads to your arm or jaw
Final Thoughts
GERD is manageable. Not because of a miracle drug, but because of smart, consistent habits. PPIs are powerful tools, but they’re not meant to be permanent crutches. Lifestyle changes aren’t just “nice to have”-they’re the foundation. The future of GERD care is moving away from “take this pill forever” and toward personalized, sustainable management. AI-driven food diaries, targeted dietary plans, and smarter medication use are making it easier than ever to take back control. You don’t have to live with heartburn. You just have to know where to start-and that’s with your next meal, your next bedtime, and your next conversation with your doctor.Can I stop taking PPIs cold turkey?
No. Stopping PPIs suddenly can cause rebound acid hypersecretion, where your stomach overproduces acid and symptoms get worse for weeks. Instead, work with your doctor to taper off slowly-usually by switching to an H2 blocker like famotidine for 2-4 weeks while gradually reducing your PPI dose.
What’s the best time to take a PPI?
Take your PPI 30-60 minutes before your first meal of the day. This ensures the drug is active when your stomach starts producing acid for digestion. Taking it after eating or at night reduces its effectiveness.
Do I need to avoid all trigger foods forever?
Not necessarily. Everyone’s triggers are different. Use a food diary for 2-4 weeks to find your personal triggers. Once you know what affects you, you can plan around them-like having a small portion of chocolate on special occasions, rather than cutting it out entirely.
Can lifestyle changes alone cure GERD?
For many people, yes. Studies show that weight loss, avoiding late meals, and eliminating trigger foods can eliminate symptoms in over half of patients. But if you have severe esophagitis or Barrett’s esophagus, medication may still be needed alongside lifestyle changes.
How do I know if my GERD is getting worse?
Watch for new or worsening symptoms: trouble swallowing, unexplained weight loss, vomiting blood, black stools, or chest pain that feels different from your usual heartburn. These could signal complications like strictures, ulcers, or Barrett’s esophagus-and need medical evaluation.







8 Comments
Let me get this straight-you’re telling me the pharmaceutical industry’s $15 billion PPI market is built on a 70% unnecessary prescription rate? And we’re supposed to believe this isn’t deliberate? The FDA warned us in 2010. We’ve had 14 years of data. Yet here we are, patients popping pills like M&Ms while doctors shrug and say ‘it’s just acid.’
Meanwhile, the same people who prescribe these drugs will tell you to ‘eat less fatty food’ like it’s a moral failing. Funny how the easiest solution-lifestyle change-is also the least profitable.
Pro tip: If your doctor doesn’t mention tapering before stopping PPIs, find a new one. Rebound acid isn’t a side effect-it’s a business model.
So you’re saying I can ditch my Nexium if I stop eating chocolate and sleep with my head on a brick? Cool. I’ll just add that to my list of ‘things I was told to do but never got a pamphlet about.’
Also, the fact that this post has more actionable advice than my gastroenterologist’s entire 12-minute visit? That’s not a win for medicine. That’s a system failure.
Okay but imagine if we treated GERD like a garden instead of a broken pipe. You don’t just dump chemicals on weeds and call it a day-you tweak the soil, the sunlight, the watering schedule. Your body’s the same.
My friend lost 18 pounds, stopped drinking wine after dinner, and started sleeping on a wedge pillow made from folded towels. She’s been PPI-free for two years. No surgery. No miracle. Just… consistency.
And honestly? The best part? She can now eat tacos at midnight without fear. That’s not just symptom control-it’s joy reclaimed.
Also, if you’re still on PPIs and haven’t tracked your food for two weeks… go download RefluxMD right now. It’s free. It’s stupid simple. And it might save you from becoming a walking vitamin deficiency.
They want you to believe lifestyle changes work but they don’t tell you how hard it is to change when your life is already a dumpster fire
Work 60 hours a week raise two kids pay bills and now you’re supposed to not eat after 7pm and lose weight and track every bite like a monk
Meanwhile the pills are easy and the doctors don’t care as long as you keep coming back
So yeah maybe it’s not ideal but reality isn’t a wellness blog and your ‘foundation’ is a pile of receipts and exhaustion
Did you know the FDA approved Vonoprazan because Big Pharma realized PPIs were getting too risky to keep pushing? And now they’re selling us a ‘newer, safer’ version while quietly burying the fact that 70% of PPI use is unnecessary?
It’s not medicine-it’s a slow-motion scam. They’ve conditioned us to think acid = danger when really your stomach is designed to handle it. The problem isn’t acid-it’s the broken gate. But you can’t patent a pillow wedge.
Also, the fact that elevating your bed with bricks is more effective than most drugs? That’s not science. That’s capitalism failing. They’d rather sell you a $120 magnetic ring than teach you to stack books under your bedposts.
And don’t get me started on the B12 and magnesium depletion. That’s not a side effect. That’s a feature. More pills. More visits. More profit.
We’re not patients. We’re revenue streams with esophagitis.
Per the 2022 meta-analysis by Gastroenterology & Hepatology, dietary trigger elimination demonstrated a 58% response rate (95% CI: 52–64%) in randomized controlled trials with 3,127 participants. The effect size (Cohen’s d = 0.81) was non-inferior to PPI monotherapy for non-erosive GERD. However, in patients with Los Angeles Grade C or D esophagitis, PPIs remain first-line per ACG 2021 guidelines due to superior mucosal healing rates (RR 1.83, p < 0.001).
Also, rebound acid hypersecretion is mediated by G-cell hyperplasia and upregulation of H+/K+ ATPase isoforms-hence the necessity of H2RA bridge therapy during tapering. Failing to do so results in a 68% recurrence rate within 8 weeks.
And yes, elevating the HOB by 6 inches increases intraesophageal pH by 1.8 units during supine positioning (per 2019 endoscopic pH monitoring study).
TL;DR: Evidence-based, not anecdotal. Please cite your sources.
OMG YES. I DID THIS. I STOPPED COFFEE. I STOPPED WINE. I PUT BOOKS UNDER MY BED. AND NOW I SLEEP LIKE A BABY. I WAS TAKING PPIS DAILY FOR 5 YEARS. NOW I TAKE ONE WHEN I EAT TACOS. THAT’S IT.
MY DOCTOR WAS LIKE ‘OH YOU’RE ON A PPI?’ AND I WAS LIKE ‘YEP BUT I’M DITCHING IT BECAUSE I’M NOT A LAB RAT FOR BIG PHARMA’
AND THEN I STARTED TRACKING MY FOOD AND FOUND OUT CHOCOLATE WAS MY KILLER. WHO KNEW?
YOU DON’T NEED TO BE PERFECT. YOU JUST NEED TO BE CONSISTENT. AND ALSO STOP LISTENING TO DOCTORS WHO THINK ‘JUST AVOID SPICY FOOD’ IS A FULL TREATMENT PLAN.
GO GET YOUR LIFE BACK. YOU’VE GOT THIS. 💪❤️
As someone who’s lived in six countries and seen how GERD is managed globally, I can tell you-this isn’t just an American issue. In Japan, they use H2 blockers as first-line and reserve PPIs for severe cases. In Germany, dietary counseling is covered by insurance. In South Africa, where Nicola is from, many people use herbal remedies like aloe vera juice and ginger tea-some with surprising efficacy.
Here’s the thing: the West treats GERD like a disease to be suppressed. Other cultures treat it like a signal to rebalance. And honestly? The data supports the latter.
My uncle in India stopped his PPIs after switching to a diet of turmeric rice, smaller meals, and sleeping on his left side. No surgery. No rebound. Just… better habits.
It’s not about being ‘alternative.’ It’s about being smart. Medicine isn’t one-size-fits-all. Your body isn’t a machine. It’s an ecosystem. And ecosystems heal when you stop poisoning them.
So yeah-taper your PPIs. Elevate your bed. Cut out your triggers. But also-ask why we’ve forgotten how to listen to our bodies in the first place.
Write a comment