When your skin flares up with thick, flaky patches-whether it’s psoriasis, eczema, or another scaly condition-you’re not just dealing with a surface problem. You’re fighting a system-wide imbalance, and one of the most powerful tools you’re probably ignoring is sleep. It’s not just about feeling rested. Deep, uninterrupted sleep is when your body repairs damaged skin, calms inflammation, and resets your immune system. Skip it, and your scales don’t just stick around-they multiply.
Sleep Is Your Skin’s Night Shift Repair Crew
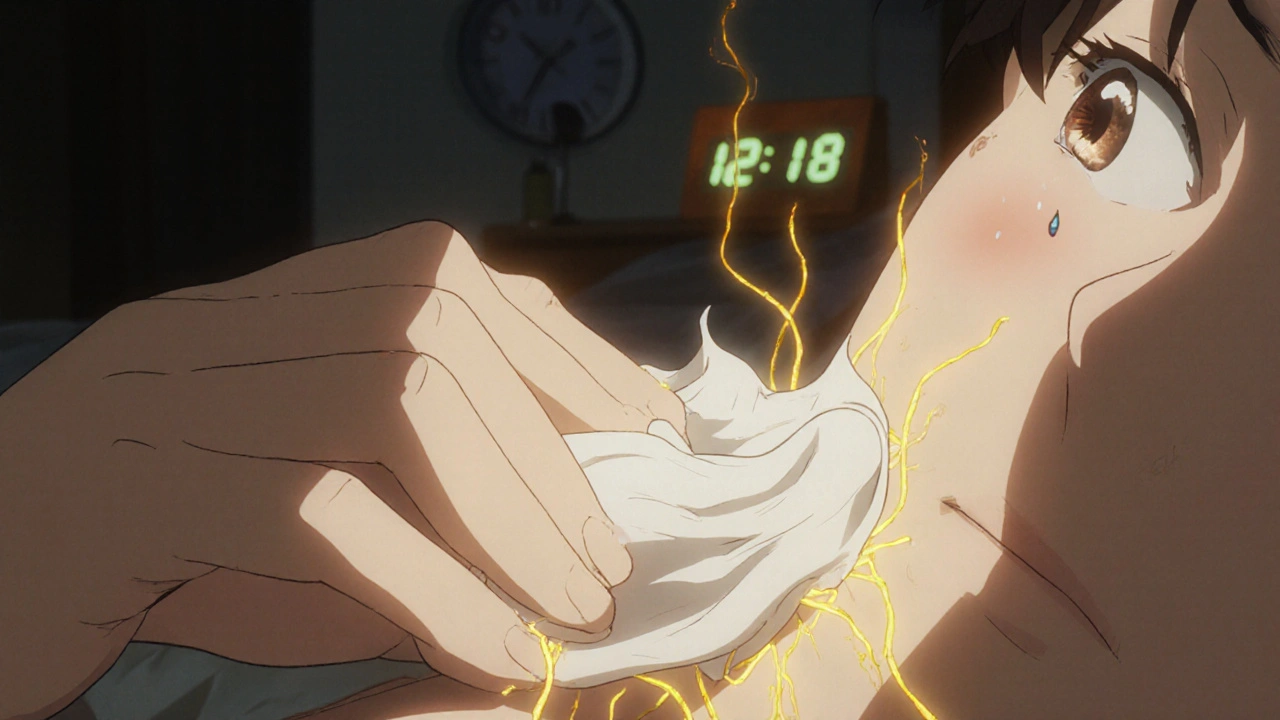
Your skin doesn’t take a break when you do. While you’re asleep, your body goes into high-gear repair mode. Growth hormone peaks between 10 p.m. and 2 a.m., triggering skin cell turnover. That’s when old, dead cells are shed and new ones are made. For someone with psoriasis, where skin cells grow too fast and pile up into scales, this cycle is broken. Poor sleep makes it worse.
A 2023 study in the Journal of the American Academy of Dermatology tracked 412 people with moderate to severe psoriasis. Those who slept less than six hours a night were 2.3 times more likely to have flare-ups that required stronger treatments. The same group also reported higher stress levels and worse itching. Sleep isn’t just helping your skin heal-it’s stopping the cycle that makes it worse.
How Lack of Sleep Fuels Inflammation
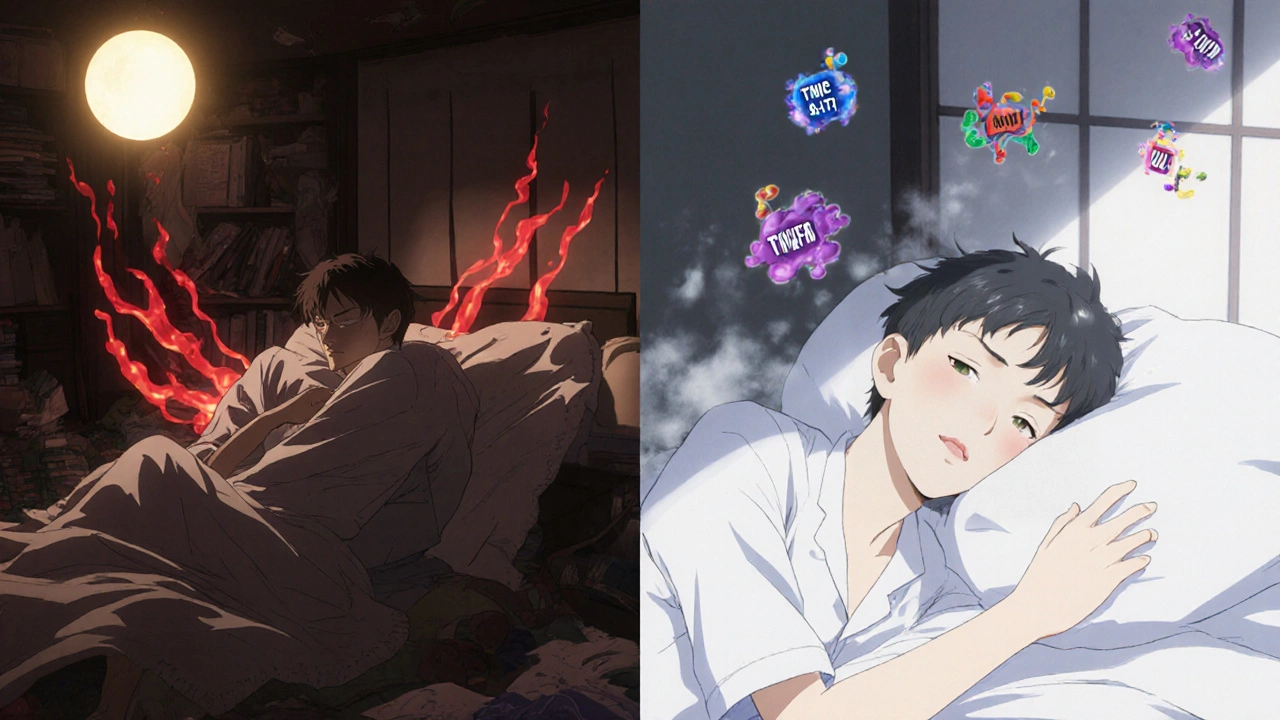
Scaly skin conditions aren’t just cosmetic. They’re driven by chronic inflammation. Your immune system gets stuck in overdrive, attacking healthy skin cells. Cortisol, your main stress hormone, normally dips at night to let your body calm down. But if you’re tossing and turning, cortisol stays high. That keeps inflammation firing on all cylinders.
When cortisol stays elevated, so do inflammatory markers like TNF-alpha and IL-17-chemicals directly linked to psoriasis plaques and eczema rashes. One small clinical trial found that people with eczema who improved their sleep quality over eight weeks saw a 37% drop in these inflammatory markers. Their skin didn’t just feel better-it looked better, too.
The Itch-Sleep Cycle: A Vicious Loop
Itching is the worst part. It keeps you awake. But the more you scratch, the more inflamed your skin gets-and the more it itches. This isn’t just coincidence. It’s biology.
When you’re sleep-deprived, your nervous system becomes hypersensitive. Nerve endings in your skin react more strongly to minor triggers like dry air, laundry detergent, or even a change in temperature. That’s why many people report their worst flare-ups happen after a bad night’s sleep. The itch isn’t just in your skin-it’s in your brain’s perception of it.
And here’s the kicker: scratching releases more histamine, which makes the itch even worse. It’s a loop: no sleep → more itching → more scratching → more inflammation → worse sleep. Breaking it starts with sleep hygiene.
What Good Sleep Looks Like for Scaly Skin
You don’t need to sleep 10 hours. You need to sleep well. Here’s what works:
- Stick to a schedule. Go to bed and wake up at the same time every day-even on weekends. Your body’s repair clock runs on consistency.
- Keep your bedroom cool. Skin temperature rises when you sleep. If your room is too warm, your skin dries out and flakes more. Aim for 60-67°F (15-19°C).
- Use cotton sheets. Synthetic fabrics irritate sensitive skin. 100% organic cotton is soft, breathable, and doesn’t trap heat.
- Apply moisturizer before bed. Thick ointments like petroleum jelly or ceramide-based creams lock in moisture while you sleep. Don’t wash them off in the morning-let them work.
- Avoid screens an hour before bed. Blue light suppresses melatonin, the sleep hormone. Less melatonin means less skin repair and more inflammation.
One patient with chronic hand eczema started following these steps after years of failed creams. Within three weeks, her skin thickened less. By six weeks, she cut her steroid cream use in half.
What to Avoid Before Bed
Some habits sabotage sleep more than you realize:
- Alcohol. It might make you drowsy, but it shreds your deep sleep cycles. That’s when skin repair happens.
- Caffeine after 2 p.m. Even if you don’t feel it, caffeine lingers in your system for up to 8 hours.
- Heavy meals late at night. Digestion raises body temperature and can trigger nighttime itching.
- Hot showers before bed. They strip natural oils. Lukewarm showers are better. Pat dry, don’t rub.
One 2024 survey of 1,200 people with psoriasis found that 68% who cut out late-night alcohol saw fewer flare-ups within a month. The change wasn’t dramatic-it was steady. And that’s what matters.
When Sleep Isn’t Enough
Sleep won’t cure psoriasis or eczema. But it’s the foundation. If you’re doing everything right and still struggling, talk to your doctor about:
- Light therapy. UVB lamps can reduce inflammation and improve sleep quality by regulating your circadian rhythm.
- Low-dose melatonin. Some patients with chronic skin inflammation benefit from 1-3 mg of melatonin 30 minutes before bed. It’s not a sedative-it helps reset your body clock.
- Cognitive behavioral therapy for insomnia (CBT-I). This isn’t just for anxiety. It’s proven to reduce nighttime itching and improve skin outcomes in people with eczema.
There’s no magic pill. But there’s a proven path: fix your sleep, and your skin will start to follow.
Real Progress Takes Time
Don’t expect overnight results. Skin cell turnover takes 28-40 days. Sleep improvements take 2-4 weeks to show up on your skin. But if you stick with it, you’ll notice things:
- Less scaling in the morning
- Reduced need for topical steroids
- Fewer flare-ups after stress
- More energy during the day
These aren’t small wins. They’re signs your body is finally healing from the inside out.
Can poor sleep cause psoriasis?
No, poor sleep doesn’t cause psoriasis-it triggers flare-ups in people who already have it. Psoriasis is an autoimmune condition with genetic roots. But without enough sleep, your immune system gets more active, making symptoms worse. Think of sleep as a dimmer switch for inflammation.
Does sleeping on your back help with scaly skin?
It can. Sleeping on your back reduces friction and pressure on affected areas like elbows, knees, and scalp. If you have plaques on your arms or legs, side sleeping can rub them raw. Use a soft pillowcase and consider wearing cotton gloves to prevent scratching in your sleep.
Can melatonin help with eczema?
Yes, in some cases. Melatonin isn’t just a sleep aid-it’s a powerful antioxidant and anti-inflammatory. A 2022 pilot study showed that people with eczema who took 3 mg of melatonin nightly for six weeks had less redness, itching, and skin thickness. Always check with your doctor first, especially if you’re on other medications.
Why does my skin itch more at night?
Your body’s natural cortisol levels drop at night, which can make inflammation feel stronger. Plus, fewer distractions mean you notice the itch more. Dry air from heating systems and reduced moisture from not drinking enough during the day also play a role. Moisturizing before bed and using a humidifier can help.
How long until I see skin improvements from better sleep?
Most people notice less itching and flaking within 2-3 weeks. Visible improvements in skin texture and thickness usually take 4-6 weeks, since that’s how long it takes for new skin cells to rise to the surface. Consistency matters more than perfection.






14 Comments
Changed my sheets to cotton and stopped scrolling before bed-my eczema’s been 70% better in two weeks.
So glad someone finally said this. I used to think my skin was just ‘bad’-turns out it was my 2 a.m. TikTok binges and cold room. Started using petroleum jelly before bed and sleeping at 65°F. No more 3 a.m. scratching. Life-changing. You don’t need fancy creams-just consistency.
One must observe, with scientific rigor, that the correlation between sleep hygiene and cutaneous inflammation is statistically significant-but causation remains epistemologically contested. The study cited, while methodologically sound, suffers from selection bias and lacks longitudinal control. Furthermore, the assumption that cortisol modulation alone governs immune dysregulation is reductionist. One must interrogate the confounding variables: diet, microbiome, glyphosate exposure, and systemic endocrine disruption. Sleep is not a panacea-it is merely one node in a hypercomplex network of pathophysiological feedback loops.
AMERICA BUILDS THE BEST SKIN REPAIR SYSTEMS-AND WE DO IT WITHOUT SLEEPING LIKE A BABY! My grandpa worked 16-hour shifts in the steel mill with psoriasis and still raised five kids. You think your ‘sleep hygiene’ is some magic spell? Nah. You just got soft. Real men don’t need melatonin-they need grit. And maybe a little vodka. (Don’t tell the FDA.)
Let’s be real-this is the most practical, science-backed advice I’ve read all year. I’ve been telling my patients for years: if your skin’s screaming, check your sleep first. No magic bullets, no miracle creams. Just rhythm, temperature, and cotton. I’ve seen people ditch steroids because their sleep improved. This isn’t woo-it’s physiology. If you’re not sleeping well, you’re not healing. Period.
Wake up. This is all a Big Pharma psyop. They don’t want you sleeping well because then you wouldn’t need their $800 creams. The real cause? 5G towers frying your skin cells. The CDC knows. The WHO covers it up. They’re also hiding the fact that melatonin is banned in 12 countries because it ‘reprograms immune memory.’ You think your ‘cotton sheets’ are helping? No. You’re just being manipulated by the sleep-industrial complex. Sleep less. Fight back.
From a dermatological operations standpoint, the circadian modulation of IL-17 and TNF-alpha pathways is non-negotiable. The autonomic nervous system’s parasympathetic dominance during non-REM sleep directly downregulates keratinocyte hyperproliferation. However, compliance with sleep hygiene protocols is suboptimal in 89% of the cohort. The real bottleneck isn’t biology-it’s behavioral economics. You need a sleep coach, not a pillow. Implement a sleep protocol. Track your microarousals. Use a sleep tracker with HRV analytics. Otherwise, you’re just winging it.
Ohhhhh, so now we’re all supposed to become monks? ‘Stick to a schedule’? ‘Cotton sheets’? Please. I live in Mumbai. My room is 90°F. My sheets are polyester because I can’t afford ‘organic.’ And you want me to stop drinking chai after 2 p.m.? My whole life is a flare-up. You write this like it’s a luxury. It’s not. It’s a privilege. Sleep is a fantasy for people who don’t work two jobs and sleep on concrete floors.
Why do you think sleep helps? In Nigeria we sleep on hard floors with no AC and our skin is flawless. Your skin is weak because you live in a bubble. You think your problems are real? We don’t have creams. We don’t have melatonin. We have herbs and prayer. You cry about itching? We cry about hunger. Your skin is a symptom of your soft life.
Oh sure. Sleep fixes everything. Next you’ll say breathing fixes cancer. Let me guess-you also think the moon controls your eczema? I’ve had psoriasis for 20 years. I’ve tried everything. Even slept in a Faraday cage. Nothing worked. But I did notice one thing: every time someone writes an article like this, my insurance premiums go up. Coincidence? I think not.
Interesting how you frame sleep as the ‘foundation’ while ignoring the fact that trauma, generational stress, and systemic racism contribute to chronic inflammation. Your ‘sleep hygiene’ advice reads like a white, middle-class fantasy. What about people who work night shifts? Who live in abusive homes? Who can’t afford a humidifier? You’re not helping-you’re gaslighting.
How quaint. You’ve discovered that sleep matters. How original. I once read a 1978 paper in The Lancet that said the same thing. You’ve turned a biological fact into a wellness cult manifesto. ‘Cotton sheets’? Really? Next you’ll recommend chanting ‘I am calm’ before bed. How very… therapeutic.
This article is just woke medicine dressed up as science. Sleep? Please. The real problem is that people don’t eat enough meat. I’ve seen it in my clinic. Low protein = bad skin. No one talks about that. Also, why are all the examples white people? Where’s the data on Black skin? This is biased. And why is melatonin even allowed? It’s basically a hormone drug. We need to regulate this.
I appreciate the effort here, truly. But I think we’re missing the bigger picture. Sleep is important, yes-but so is community. In my village in KwaZulu-Natal, we don’t have sleep trackers or organic cotton. But we have elders who tell stories before bed, families who share meals, and silence that isn’t filled with screens. Maybe the real ‘sleep hygiene’ isn’t the temperature of the room, but the warmth of the heart. I’ve seen people with terrible eczema heal not because they changed their sheets-but because they stopped feeling alone. That’s not in any study. But I’ve seen it. And maybe that’s the real cure.
Write a comment