When you’re scheduled for surgery, your body is about to go through a controlled crisis. Doctors will put you under, cut into you, and manipulate your organs-all while using a cocktail of powerful drugs. If you’ve had a bad reaction to a medication before, not telling your medical team could be the difference between a smooth recovery and a life-threatening emergency. This isn’t just about being careful. It’s about survival.
Why Drug Reactions Matter More Than You Think
Every year, around 4.5% of surgical complications are linked to medication errors, according to a 2022 NIH study. Of those, allergic reactions account for 1.1% of anesthesia-related deaths. That might sound small, but consider this: anaphylaxis during surgery happens in 1 out of every 10,000 to 20,000 cases. And most of those cases are preventable. The problem isn’t that doctors don’t know how to respond. It’s that patients often don’t know how to explain what happened to them. Many people say, “I’m allergic to penicillin,” when they really had nausea or a rash. Others forget the name of the drug entirely. A 2022 study in Anesthesia & Analgesia found that 32% of patients couldn’t recall the exact medication that caused their reaction. True drug allergies trigger your immune system. Symptoms like hives, swelling, trouble breathing, or a drop in blood pressure are red flags. But side effects-like dizziness, upset stomach, or fatigue-are not allergies. Confusing the two can lead to unnecessary delays, missed treatments, or even wrong drug choices during surgery.What You Need to Remember Before Your Pre-Op Visit
Start thinking about your drug history at least a week before your surgery. Don’t wait until the day before. You need to be specific. Here’s what to gather:- The drug name-not just “that antibiotic” or “the pain pill.” Use the generic name if you can (like ibuprofen instead of “Advil”).
- What happened-rash? Swollen throat? Vomiting? Fainting? Write it down.
- When it happened-minutes after taking it? Hours later? Days?
- How it was treated-did you get epinephrine? Antihistamines? Were you hospitalized?
- Any other meds you take-prescription, over-the-counter, vitamins, herbs, or supplements. Even fish oil or St. John’s wort can interfere.
Many patients don’t realize that herbal supplements like ginkgo biloba or garlic can thin your blood. Others forget that even a single dose of aspirin years ago could matter if you’re having heart surgery. Your anesthesiologist needs the full picture.
How to Talk to Your Care Team
Don’t assume the nurse or doctor will ask the right questions. Be proactive. Say this:“I had a bad reaction to [drug name] in the past. Here’s what happened…”Use clear, calm language. Avoid phrases like “I think I’m allergic” or “It was probably nothing.” Say “I had a confirmed reaction” or “I was diagnosed with an allergy.” If you’re nervous, bring a written list. Or better yet-use a drug allergy card. These are small plastic cards you can get from allergists or pharmacies. They list your reactions, the drugs to avoid, and emergency contact info. Eighty-seven percent of allergists recommend them, according to a 2021 study. Your anesthesiologist will ask you about:
- Latex allergies (gloves, tubing)
- Reactions to muscle relaxants like rocuronium or succinylcholine
- History of malignant hyperthermia (a rare but deadly reaction to certain anesthetics)
- Previous reactions during surgery
They’ll also check if you’ve taken any medications that need to be stopped ahead of time. For example:
- NSAIDs (like ibuprofen) should be stopped 7 days before surgery
- Ticagrelor (Brilinta) needs 3-5 days to clear your system
- Prasugrel (Effient) requires 7 days
- MAO inhibitors (like phenelzine) must be stopped 2 weeks ahead to avoid dangerous interactions
These aren’t suggestions. They’re safety rules backed by guidelines from the American Society of Health-System Pharmacists (ASHP) and the American Society of Anesthesiologists (ASA).
What Happens if You Forget or Don’t Tell Them?
A 2021 incident reported to the Anesthesia Patient Safety Foundation involved a patient with a known vancomycin allergy. The team didn’t know because the allergy wasn’t documented in their records. During surgery, the drug was given. The patient went into anaphylactic shock. It took emergency drugs, intubation, and hours of stabilization to save them. Another case, shared on Reddit by a patient with a 10-year-old rocuronium reaction, showed what should happen. The pre-op nurse spent 20 minutes writing down every detail: what the patient ate that day, their stress levels, even the brand name of the drug. That attention to detail prevented a repeat. The difference? Documentation. If your allergy isn’t written down in your chart, it doesn’t exist to the team.How Hospitals Are Trying to Fix This
Most hospitals now use electronic health records (EHR) with mandatory allergy fields. Systems like Epic and Cerner require you to enter:- Drug name
- Reaction type
- Date of reaction
- Severity
Pharmacists now screen all surgery schedules 24 hours ahead of time. If they see a red flag, they alert the anesthesiologist. In hospitals that do this, drug-related complications drop by 37%, according to a 2021 Froedtert Hospital study.
But not every hospital is equal. Academic centers are nearly 100% compliant. Community hospitals? Only 74% have full protocols. And in emergencies, 37% of institutions still don’t have complete allergy records.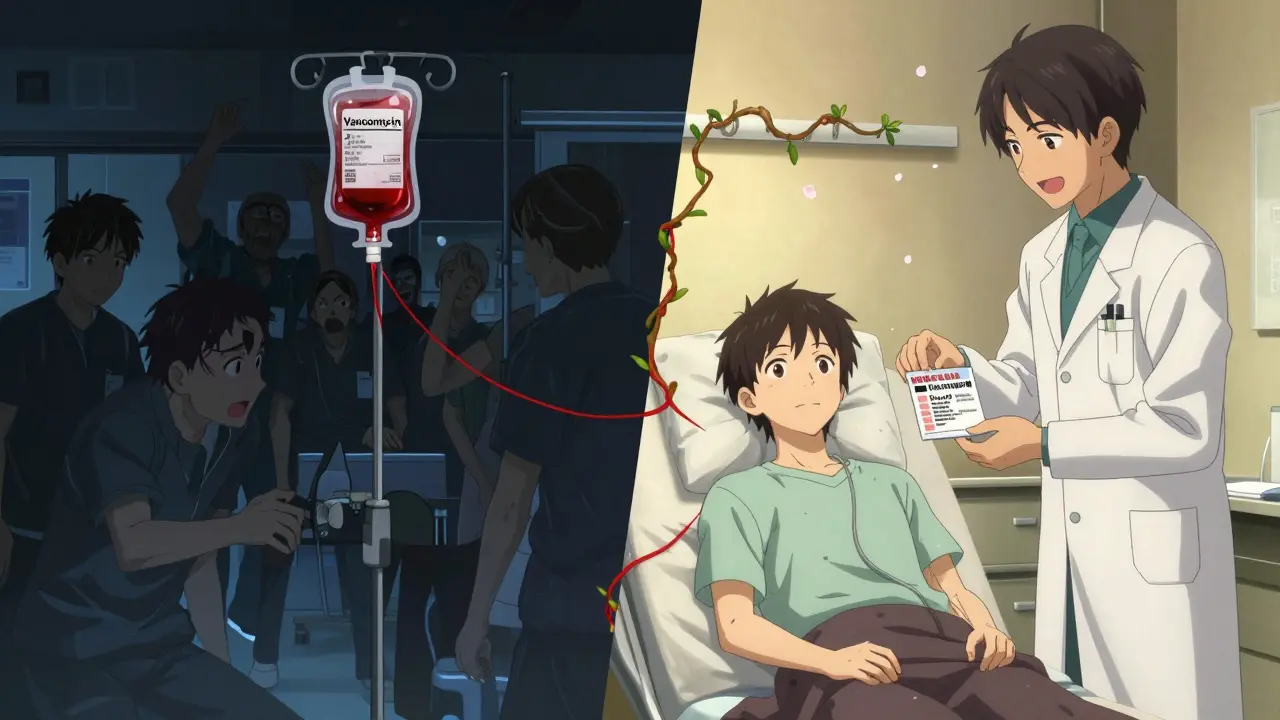
What You Can Do Right Now
1. Write it down-on paper or your phone. List every drug, reaction, and date. 2. Call your pharmacy-they have your full prescription history. 3. Ask your allergist-if you’ve had a serious reaction, get a formal allergy evaluation. They can test you and give you a card. 4. Bring your list to every appointment-don’t rely on memory or old records. 5. Confirm it’s in your chart-ask the nurse before surgery: “Is my allergy listed in the system?”If you’ve ever had a reaction-even if it was years ago-treat it like a live wire. Don’t downplay it. Don’t assume they’ll find it. Say it. Write it. Show it.
What If You’re Not Sure What Happened?
Some people have vague memories. Maybe you got sick after a surgery, but you don’t know why. That’s okay. Say: “I had a bad reaction after surgery, but I don’t remember the drug. I’d like to be tested.” Many hospitals now offer pre-surgery allergy testing. If you’ve had a reaction and haven’t been evaluated, ask for a referral to an allergist. The Spanish Journal of Anesthesia and Critical Care recommends getting tested within 4-6 weeks after the reaction.Even if you can’t pinpoint the drug, your team can still avoid high-risk categories. For example, if you had a reaction to one muscle relaxant, they’ll avoid the whole class.
Final Thought: This Is Your Safety, Not Their Job
Doctors and nurses want to keep you safe. But they can’t read your mind. If you’ve had a drug reaction, you’re not just a patient-you’re a source of critical information. Your job isn’t to be polite. It’s to be clear. To be specific. To be stubborn. The system works best when you’re part of it. Don’t wait for them to ask. Don’t hope they’ll find it. Tell them. Before surgery. Every time.What if I only had a mild reaction years ago? Do I still need to tell them?
Yes. Even mild reactions can become more severe with repeat exposure. A rash or nausea once could turn into anaphylaxis the next time. Medical teams treat all past reactions as potential risks, no matter how minor they seemed at the time.
Can I just say I’m allergic to everything to be safe?
No. Overreporting allergies makes it harder for doctors to choose safe medications. If you say you’re allergic to everything, they may avoid effective drugs and use riskier alternatives. Be accurate. List only what you know for sure. If you’re unsure, say so-don’t guess.
Do I need to tell them about supplements and herbal remedies?
Yes. Supplements like ginkgo, garlic, ginger, and fish oil can interfere with blood clotting. St. John’s wort can affect anesthesia metabolism. Even if you think it’s “natural,” it can have serious effects during surgery. List everything.
What if I’m allergic to latex? Is that important?
Very important. Latex is in gloves, IV tubing, catheters, and tourniquets. If you’re allergic, your team needs to use latex-free equipment. This isn’t optional-it’s standard protocol. Tell them even if you think it’s unrelated to surgery.
I got a reaction during a previous surgery. Should I get tested?
Yes. A formal allergist evaluation can identify the exact drug that caused the reaction and confirm whether it’s a true allergy or a side effect. Most hospitals recommend this within 4 to 6 weeks after the event. It gives you a clear, documented answer for future procedures.