Hyponatremia Risk Calculator for SSRIs
Assess Your Hyponatremia Risk
Hyponatremia is a dangerous condition where sodium levels drop too low, especially when taking SSRIs. This calculator helps you understand your risk factors and make informed decisions with your doctor.
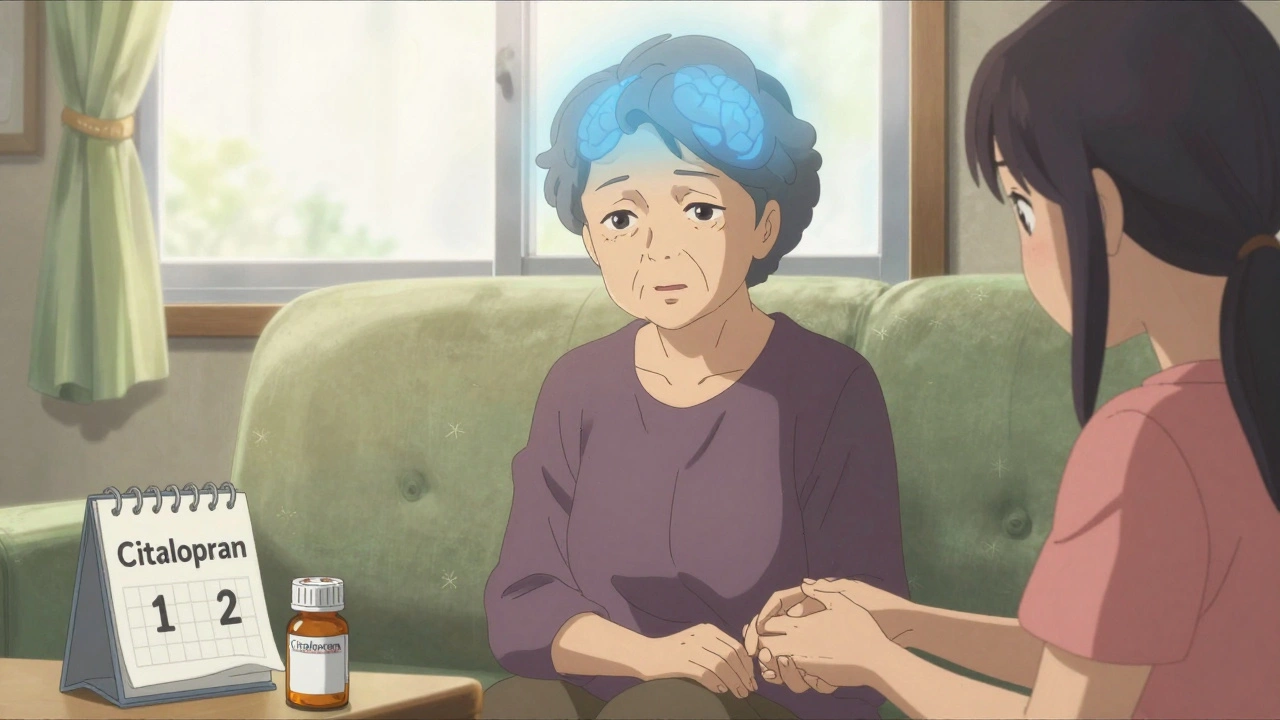
When you start an SSRI for depression, you expect better sleep, less anxiety, maybe even a little more energy. But what you don’t expect is to feel confused, dizzy, or strangely nauseous-especially if you’re over 65. These aren’t just signs of aging. They could be warning signs of something far more dangerous: hyponatremia-dangerously low sodium in your blood-triggered by the very medication meant to help you feel better.
What Exactly Is Hyponatremia?
Hyponatremia means your blood sodium level has dropped below 135 mmol/L. Sodium isn’t just table salt-it’s critical for nerve function, muscle control, and keeping fluid balanced in and out of your cells. When sodium dips too low, water floods into your brain cells, causing them to swell. That’s when confusion, headaches, nausea, and even seizures start showing up. In extreme cases, sodium levels can plunge to 118 mmol/L or lower. That’s not just abnormal-it’s life-threatening.This isn’t rare. A 2024 meta-analysis found that nearly 1 in 25 people taking SSRIs develop hyponatremia. For those over 65? The risk jumps to almost 1 in 6. And it doesn’t happen right away. Most cases show up between two and four weeks after starting the drug-or after a dose increase. That’s why many doctors and families miss it. They think the confusion is just dementia. The fatigue? Just getting older. The nausea? A stomach bug.
Why Do SSRIs Cause This?
It all comes down to serotonin. SSRIs boost serotonin in your brain to lift your mood. But serotonin doesn’t just stay in your brain. It also affects your hypothalamus-the part of your brain that controls how much antidiuretic hormone (ADH) your body releases. Too much serotonin = too much ADH. And too much ADH tells your kidneys to hold onto water instead of flushing it out.You end up with more water in your bloodstream. That water dilutes your sodium. Your sodium level drops. Your brain swells. And suddenly, you’re confused, stumbling, or even hospitalized.
Not all SSRIs are equal in this risk. Citalopram and sertraline carry the highest risk, with citalopram nearly 2.4 times more likely to cause hyponatremia than other antidepressants. Fluoxetine and paroxetine follow closely. Even if you’ve been on one of these for months, a small dose increase can push you over the edge.
Who’s Most at Risk?
You might think this is just a side effect that affects everyone equally. It doesn’t. The biggest risk factors are clear:- Age over 65-Your kidneys don’t clear fluid as well, and your body’s natural sodium balance weakens. Relative risk jumps 3.7 times.
- Women-Nearly two-thirds of reported cases are in women, likely due to lower body weight and hormonal differences.
- Low body weight-If you weigh less than 60 kg, your blood volume is smaller, so water retention hits harder.
- Already on diuretics-Especially thiazides like hydrochlorothiazide. Taking these with an SSRI increases hyponatremia risk by over 4 times.
- Kidney problems-If your eGFR is below 60, your body can’t regulate fluid properly.
- Multiple medications-The more drugs you take, the higher the chance of dangerous interactions.
One case from a Reddit caregiver in March 2024 described her 82-year-old mother: two weeks after starting citalopram, she became unrecognizable-confused, withdrawn, unable to dress herself. Sodium was 122 mmol/L. Hospitalized. Medication stopped. Took days to recover. She wasn’t ‘just getting forgetful.’ She had a medical emergency.
What Do the Experts Say?
The evidence is now overwhelming. The American Geriatrics Society’s 2023 Beers Criteria explicitly lists SSRIs as potentially inappropriate for older adults because of hyponatremia risk. The 2024 European Psychiatry meta-analysis concluded that mirtazapine should be the first choice for elderly patients needing antidepressants-not SSRIs.Mirtazapine? It’s not an SSRI. It doesn’t strongly affect serotonin in the same way. Its hyponatremia risk is less than half that of SSRIs. Studies show for every 1,000 older adults prescribed mirtazapine instead of an SSRI, you prevent 12 cases of hyponatremia. That’s not just safer-it’s life-saving.
Dr. Elena Martinez, lead author of the 2024 study, says bluntly: “Mirtazapine should be first-line for elderly patients.” Dr. Thomas Reynolds, a geriatric psychiatrist, recommends this: “Test sodium before starting any antidepressant. Test again at two weeks. That’s now standard care.” Yet, a 2023 survey found that 63% of primary care doctors didn’t even know the typical onset window was 2-4 weeks.
What About Other Antidepressants?
Not all antidepressants carry the same risk. Here’s how they stack up:| Antidepressant | Risk Compared to SSRIs | Notes |
|---|---|---|
| Citalopram | 2.37x higher | Strongest association; highest risk |
| Sertraline | 2.15x higher | Very common; high risk in elderly |
| Fluoxetine | 1.98x higher | Long half-life; risk persists |
| Paroxetine | 1.82x higher | Anticholinergic effects add to confusion |
| Venlafaxine (SNRI) | 1.72x higher | Still risky, but lower than SSRIs |
| Amitriptyline (TCA) | 1.94x higher | Older drug; anticholinergic side effects |
| Bupropion | 0.85x (lower) | Doesn’t affect serotonin; safest non-SSRI |
| Mirtazapine | 0.47x (lowest) | First choice for elderly; minimal hyponatremia risk |
If you’re over 65, have kidney issues, or are on a diuretic, mirtazapine or bupropion are far safer starting points. They still treat depression. They just don’t flood your body with extra water.
How to Spot It Early
The symptoms start small. You might think it’s nothing:- Mild headache
- Feeling unusually tired
- Nausea without a stomach bug
- Loss of appetite
- Feeling “off” or foggy
Then it escalates:
- Confusion
- Difficulty walking
- Slurred speech
- Seizures
- Coma
If you or someone you care for is on an SSRI and starts showing any of these, especially after two weeks, get a blood test. Don’t wait. Don’t assume it’s dementia. Sodium levels can drop fast. Recovery is quick-if caught early.

What Should You Do?
If you’re prescribed an SSRI:- Ask for a baseline sodium test before starting.
- Request a repeat test at two weeks.
- Ask if mirtazapine or bupropion could be an alternative, especially if you’re over 65.
- Don’t increase your dose without checking sodium again.
- If you feel confused or nauseous, tell your doctor immediately-don’t wait for your next appointment.
If you’re already on an SSRI and feel fine? Don’t stop. But know the signs. And ask your doctor if you’re on a high-risk medication. The 2024 guidelines say monitoring is non-negotiable for older adults.
And if you’re a caregiver? Pay attention. If your parent suddenly seems different-less alert, more withdrawn, forgetful in a new way-it’s not just aging. It could be low sodium. A simple blood test can save a life.
What Happens If It’s Caught?
Mild hyponatremia (sodium 125-134 mmol/L)? Stop the SSRI. Limit fluids to 800-1,000 mL a day. Sodium usually returns to normal in 2-4 days.Severe hyponatremia (below 125 mmol/L)? Hospitalization. IV hypertonic saline. Slow correction-no more than 6-8 mmol/L per day. Go too fast, and you risk osmotic demyelination syndrome, a rare but devastating brain injury.
Recovery is possible. But delay? That’s when things turn irreversible.
The Bigger Picture
SSRIs are still the most prescribed antidepressants in the U.S.-over 214 million prescriptions in 2023. But something’s changing. Between 2018 and 2023, SSRI starts in patients over 65 dropped by 22%. Mirtazapine prescriptions for that group rose by 35%. That’s not coincidence. That’s medicine learning.The FDA now requires all SSRI labels to include hyponatremia warnings. The European Medicines Agency is reviewing the safety profile. And the cost? In the U.S. alone, SSRI-induced hyponatremia costs $1.27 billion a year in hospital visits and emergency care.
But the real cost isn’t money. It’s the 38% of mild cases that go undetected in primary care. It’s the elderly person who falls because they’re confused. It’s the family who thinks their loved one is slipping into dementia-when it was just a medication side effect they never knew to watch for.
Can SSRIs cause confusion in elderly patients?
Yes. SSRIs can cause confusion in elderly patients through hyponatremia-low sodium levels caused by excess water retention. This typically happens 2-4 weeks after starting or increasing the dose. Symptoms like disorientation, memory lapses, or dizziness are often mistaken for dementia, but they’re a medical reaction to the drug. A simple blood test can confirm low sodium.
Which SSRI has the lowest risk of hyponatremia?
None of the SSRIs have low risk. All carry significant hyponatremia risk, especially in older adults. Citalopram and sertraline have the highest risk. If you’re over 65 or have kidney issues, mirtazapine or bupropion are safer alternatives. They treat depression without triggering water retention.
How long does it take for hyponatremia to develop after starting an SSRI?
Hyponatremia usually develops between 2 and 4 weeks after starting an SSRI or increasing the dose. It rarely happens immediately. That’s why it’s often missed. Doctors and families assume symptoms are from aging or another condition. Testing sodium at the two-week mark is critical.
Should I stop my SSRI if I feel confused?
Don’t stop abruptly without medical advice. But do get tested immediately. Confusion, nausea, or dizziness on an SSRI could be hyponatremia. Stopping the drug is often the first step in treatment, but it should be done under supervision. Your doctor may recommend fluid restriction and a blood test before deciding on next steps.
Is mirtazapine really safer than SSRIs for older adults?
Yes. Multiple studies confirm mirtazapine has less than half the risk of hyponatremia compared to SSRIs. It’s now recommended as first-line for elderly patients by the American Geriatrics Society and leading psychiatric researchers. It’s effective for depression, helps with sleep, and doesn’t trigger the same hormonal response that causes water retention.




15 Comments
My grandma started sertraline last year and got super confused. We thought it was dementia. Turned out her sodium was 121. They stopped the med, she bounced back in 3 days. Why isn't this common knowledge?
As a nurse who’s seen this 3x in the last year, I’m screaming into the void. Elderly patients get SSRIs like they’re candy. No baseline labs. No follow-up. Just ‘try this, come back in 6 weeks.’ By then, it’s too late. Test sodium at week 2. Please. I’m begging you.
And if you’re a caregiver? If Mom suddenly stops recognizing you or can’t button her shirt? Don’t wait. Go to urgent care. Ask for a basic metabolic panel. It’s a $30 test. Could save her life.
I’ve been on citalopram for 18 months and never had an issue-but my 78-year-old aunt? Two weeks after starting it, she was stumbling, muttering nonsense, forgetting her own birthday. We thought she was fading. Turns out her sodium was lower than a desert well. They admitted her. They stopped the med. She’s back to knitting and complaining about the weather. It’s terrifying how fast this happens. And how invisible it is.
Doctors act like SSRIs are harmless. They’re not. They’re like a silent tide. You don’t feel it rising until you’re already drowning.
It’s not just SSRIs. It’s the entire system. We treat aging like a disease to be medicated, not a phase of life to be understood. We throw pills at confusion, fatigue, sadness-instead of asking: What’s missing? Connection? Movement? Sleep? Nutrition?
Mirtazapine is safer? Great. But why not start with therapy, community, sunlight, walking? Why is pharmacology the first, last, and only answer? We’ve outsourced care to chemicals and ignored the human stuff that actually heals.
I appreciate the data here, and the urgency. But I worry this post might scare people away from needed treatment. Depression in the elderly is underdiagnosed and deadly. The goal isn’t to demonize SSRIs-it’s to use them wisely. Testing sodium, choosing alternatives like mirtazapine, monitoring closely-these are responsible practices, not red flags.
Let’s not swing from ‘pill every problem’ to ‘never prescribe anything.’ Let’s just do it better. With eyes open.
As a medical professional from India, I must commend the clarity of this post. In our hospitals, elderly patients are often prescribed SSRIs without adequate screening for electrolyte imbalances. The cultural tendency to attribute cognitive changes to ‘old age’ is deeply entrenched. This article should be mandatory reading for all primary care physicians, especially in resource-limited settings where diagnostic tools are scarce.
I have personally witnessed a case where a patient’s confusion resolved within 72 hours of discontinuing sertraline and initiating fluid restriction. The tragedy lies not in the medication, but in the lack of awareness. Education must precede prescription.
Let me be perfectly clear: if you are over 65 and your doctor prescribes an SSRI without ordering a baseline sodium panel and a follow-up at 14 days, you are being malpracticed. This is not speculation. This is not opinion. This is standard of care, as defined by the American Geriatrics Society, the EMA, and multiple peer-reviewed meta-analyses.
Any physician who fails to do this is either negligent or dangerously ignorant. And if you are a family member? Demand the test. Write it on the chart. If they refuse, get a second opinion. Lives are not expendable for institutional inertia.
Oh great. Now we’re blaming SSRIs for everything. Next thing you know, they’ll say sunlight causes skin cancer or water causes drowning. People are getting confused because they’re old, not because of a pill. My uncle’s been on fluoxetine for 8 years and he’s sharper than half the people in this thread. Stop pathologizing aging.
Also, mirtazapine makes you gain 30 pounds and sleep 14 hours a day. Sounds like a worse deal. Maybe just let Grandma nap and stop medicating her into oblivion.
As a Black woman whose mother was misdiagnosed with dementia for 11 months while on sertraline, I’m so tired of this being ignored. We were told she was ‘just getting forgetful.’ Turns out her sodium was 119. They thought it was Alzheimer’s. It was a drug side effect.
And guess what? Her doctor didn’t even know SSRIs caused this. He’s white, 70, and practiced since 1985. This isn’t just about meds-it’s about who gets listened to. Elderly women, especially women of color, get dismissed as ‘just old.’ We need systemic change, not just lab tests.
My mom took citalopram and started walking into walls. We thought she was drunk. She wasn’t. Sodium was 120. We rushed her to the ER. They said ‘thank you for catching this.’ Why didn’t the pharmacy warn us? Why didn’t the doctor? I’m so mad I could scream.
PLEASE if you’re on an SSRI and feel weird after 2 weeks-GET BLOODBLOODBLOOD. Don’t wait. Don’t hope it goes away. This isn’t a side effect. It’s a medical emergency.
Let’s be honest here-this isn’t about medicine, it’s about capitalism. Pharma companies spent billions marketing SSRIs as ‘safe, non-addictive, miracle cures’-and now they’re quietly burying the data on hyponatremia because it’s inconvenient. The FDA’s warning label? Barely legible. The EMA’s review? Still pending. Meanwhile, prescriptions hit 214 million last year. This isn’t negligence. It’s profit-driven negligence.
And don’t get me started on how mirtazapine is cheaper, less monitored, and less marketed. It’s not that it’s better-it’s that it doesn’t make enough money. We’re not talking about science here. We’re talking about who gets to profit from your grandmother’s confusion.
Wait… so SSRIs cause water retention? And that’s why people get confused? Hmm. Interesting. But have you considered… what if this is all part of a larger government agenda to control the elderly? I mean, think about it-why would they push these drugs so hard? Maybe it’s to make seniors dependent on hospitals, so they can track them through their bloodwork? Or maybe… it’s the water fluoridation? The sodium levels are a distraction from the real issue: the deep state is using antidepressants to lower our collective consciousness.
Also, my cousin’s neighbor’s dog got sick after the new water filter was installed. Coincidence? I think not.
This post is dangerously irresponsible. You’re telling people to stop SSRIs based on a few case studies and a meta-analysis? What about the millions who benefit? What about the fact that depression kills more elderly people than hyponatremia? You’re playing doctor with fear, not facts.
And mirtazapine? It’s sedating. It’s weight-gaining. It’s not a ‘safe alternative’-it’s a trade-off. You want to avoid hyponatremia? Then don’t take antidepressants at all. That’s the real solution. Stop medicating sadness. Let people suffer. It builds character.
From a clinical psychology perspective, the pathophysiological mechanism described here is compelling-serotonin’s effect on ADH release leading to SIADH (syndrome of inappropriate antidiuretic hormone secretion) is a well-documented phenomenon in geriatric psychopharmacology.
However, the emotional valence of this post risks triggering therapeutic nihilism among patients who are otherwise benefiting from SSRIs. A risk-benefit analysis is essential. For some, the risk of hyponatremia is low, and the relief from suicidal ideation is profound.
What’s needed is not blanket avoidance, but individualized, longitudinal monitoring protocols integrated into primary care workflows. The data is clear. The framework exists. Implementation is the barrier.
So let me get this straight-you’re saying that after 30 years of prescribing SSRIs, doctors are just now figuring out they might cause brain swelling? And we’re supposed to believe this is a revelation? This isn’t medicine. This is a collective, decades-long failure of basic science education. I’m not mad. I’m just… disappointed. We could’ve prevented this. We didn’t. And now we’re writing blog posts about it like it’s new. Pathetic.
Write a comment