Imagine opening your medicine cabinet and not being able to tell which pill is which. All the bottles look the same-white, oval, no markings you can read. You’ve taken this one before, but is it your blood pressure pill or your sleeping pill? You can’t be sure. This isn’t a rare scenario. In the UK alone, over 1.8 million people live with significant vision loss, and hundreds of thousands more struggle with hearing loss. For them, taking medication safely isn’t about convenience-it’s a matter of life or death.
Why Medication Safety Is Different with Low Vision or Hearing Loss
Most people don’t think twice about reading a prescription label. But for someone with low vision, standard print is often unreadable. Labels use 7- to 10-point font. The minimum recommended size? 18-point. That’s more than double. And even if the text is large enough, contrast matters. A light gray label on a white bottle? Useless. Glare from glossy paper? Makes it worse. For those with hearing loss, the problem starts at the pharmacy counter. Pharmacists explain dosing instructions out loud. In a busy store, background noise drowns them out. No one repeats it. No one writes it down. You leave confused-and that’s when mistakes happen. Studies show people with vision loss are 1.67 times more likely to make a medication error than those without. These aren’t small mistakes. People take the wrong dose, take pills at the wrong time, or even take expired medicine. One user on Reddit shared how they almost took their blood pressure pill at bedtime because the new generic looked identical to their sleeping pill-same shape, same color, no distinguishing marks.What Makes Medications Hard to Use
Not all medications are equally difficult. Tablets and capsules? Most people manage fine. But liquids? Eye drops? Those are the real troublemakers. A 2019 study in Malaysia found that 82% of visually impaired participants could handle pills without help. But only 47% could measure liquid doses correctly. For eye or ear drops? That number dropped to 39%. Why? Because measuring a teaspoon or a few drops requires fine motor control and visual precision-something many can’t do. Color-coding helps. Red for morning pills, blue for night. But here’s the catch: not everyone agrees on what color means what. One person’s red is another person’s orange. Rubber bands around bottles? They work for some. But if the band slips or breaks, you’re back to guessing. Braille labels sound like a perfect fix. But only 15% of adults who lose vision later in life can read braille. That’s because most people learn braille as children. If you lose your sight at 60, you’re unlikely to learn it now.What Works: Real Solutions People Use
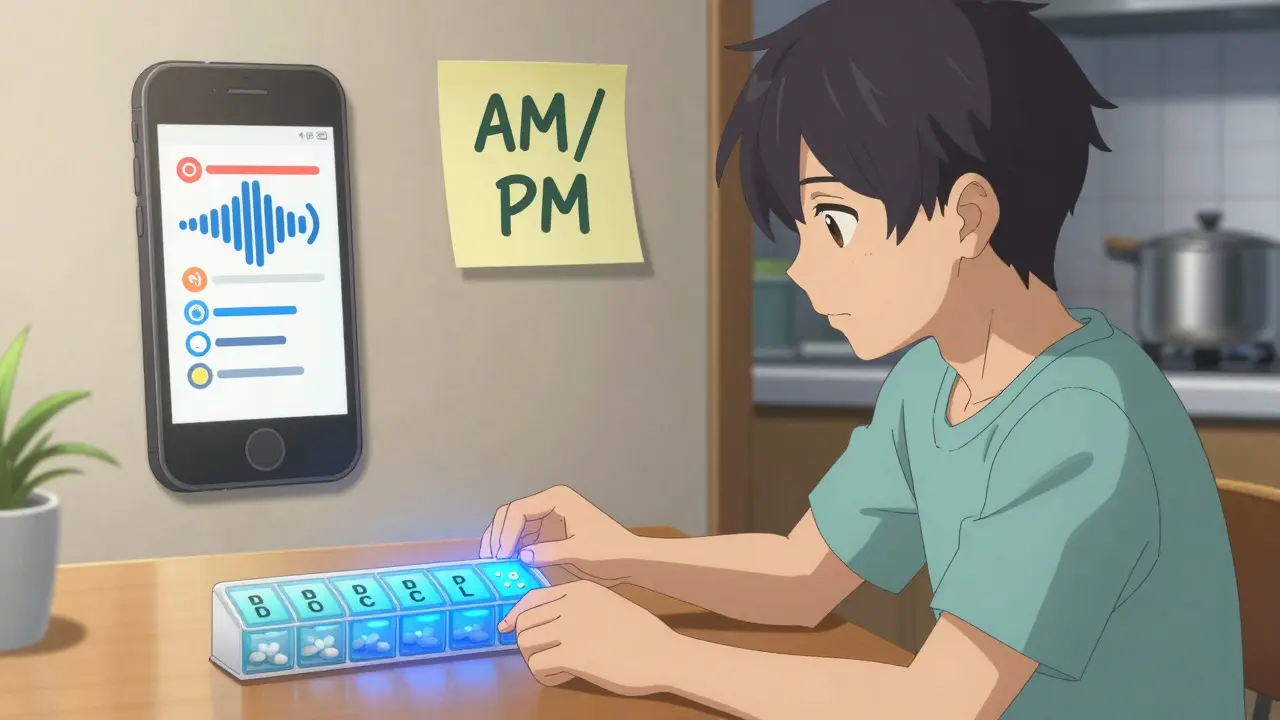
There are tools that actually help. Not just theory-real ones used by people every day. The Talking Rx device is one of the most effective. It’s a small gadget that plays back a recorded message when you press a button. You can record your own voice: “Take one white pill with breakfast.” It’s not fancy, but it works. In tests, 92% of users took their meds correctly after using it. Electronic pill organizers like PillDrill ($29.99) and Hero Health ($199.99) beep, flash lights, and send alerts to your phone. Hero Health even lets your caregiver know if you miss a dose. But they’re expensive. And if you can’t see the screen or hear the alarm, they’re useless. Simple, low-cost fixes work too. A pharmacist can use a black marker to write “AM” or “PM” on the bottle. That takes 30 seconds. Color-coding with sticky notes? 45 seconds. Rubber bands? 20 seconds per pill. These aren’t high-tech, but they’re reliable-and free. One user told Guide Dogs UK: “The rubber band system my pharmacist set up saved me from a dosing error last month.” That’s the kind of solution that shouldn’t be rare.
Why Pharmacies Keep Getting It Wrong
You’d think pharmacies would be on top of this. After all, they’re the ones handing out the meds. But here’s the truth: only 32% of U.S. pharmacies consistently offer any accessibility accommodations. Just 12% follow the full guidelines from the American Foundation for the Blind. Why? Time and money. Pharmacists are rushed. Medicare pays them $14.97 per prescription. No extra pay for spending five extra minutes explaining labels or printing large-print instructions. Most don’t have the training either. A 2022 survey found only 28% of pharmacies routinely spend extra time with visually impaired patients. Regulations don’t help much either. The Americans with Disabilities Act says pharmacies must make “reasonable accommodations.” But it doesn’t say what those are. The FDA and UK’s MHRA have guidelines-but they’re not mandatory. Manufacturers don’t have to put dosage instructions in braille. They don’t have to use high-contrast labels. They don’t have to make bottles easy to open. Dr. Tim Johnston from RNIB says it plainly: “The current system isn’t designed for people with sight loss. It’s a safety issue, not a convenience issue.”What You Can Do Right Now
You don’t have to wait for the system to fix itself. Here’s what you can do today:- Ask for large-print labels-specifically 18-point font or larger. Don’t settle for “bigger print.” Be exact.
- Request color-coding-ask the pharmacist to use colored stickers or tape for morning, afternoon, evening, and night doses.
- Use rubber bands-one band for once-daily, two for twice-daily. Keep it simple.
- Record your meds-use your phone to record a voice note saying, “This is my 10mg metformin, take with breakfast.”
- Get a pill organizer-even a basic one with labeled compartments helps. Don’t wait for fancy tech.
- Bring someone with you-to the pharmacy, to your doctor. Even if it’s just once to set up your system.
What Healthcare Providers Need to Know
If you’re a doctor, nurse, or pharmacist: stop assuming your patient can read the label. Don’t ask, “Do you understand?” Ask, “Can you show me how you take your pills?” Watch them. See if they hesitate. See if they open the wrong bottle. Learn the AFB’s 12-point labeling checklist. Use high-contrast ink. Avoid shiny paper. Never rely on color alone. Offer to record instructions. Offer to print labels in braille if they can read it. Don’t wait for them to ask. The American Occupational Therapy Association found that when these steps are followed, medication errors drop by 40-60%. That’s not magic. That’s basic care.The Future: What’s Changing
There’s hope. The AFB is launching a pharmacy certification program in 2024. RNIB is rolling out a standardized labeling system in 2025. These aren’t just ideas-they’re coming. But progress is slow. Without laws that require accessible packaging, change will be patchy. Right now, only 8% of medicine packaging includes any accessibility feature beyond the drug name in braille. Dosage? Timing? Frequency? Almost never included. The numbers are growing. By 2028, demand for accessible medication tools will rise 35% because of aging populations. Older adults take an average of 4.7 prescriptions. More people will need help. The system has to catch up.Final Thought: You’re Not Alone
You might feel like you’re the only one struggling. You’re not. Sixty-eight percent of people with vision loss never tell their doctor about their medication problems. They’re embarrassed. They don’t want to be a burden. But silence is dangerous. Speak up. Ask for help. Use the tools that work. And if you’re a caregiver, don’t just sort pills for them-teach them how to do it themselves. Independence matters. Medication safety isn’t about fancy gadgets. It’s about clear labels, clear instructions, and people who listen. The technology exists. The guidelines exist. What’s missing is the will to make them standard.Can I get my prescriptions printed in large font for free?
Yes. Most pharmacies will print large-print labels at no extra cost if you ask. You don’t need a special form. Just say, “I have low vision and need my prescription label printed in at least 18-point font.” If they refuse, ask to speak to the pharmacist-in-charge. The American Foundation for the Blind’s guidelines support this request as a reasonable accommodation under the ADA.
What if I can’t read braille but want a tactile label?
You don’t need braille. Use raised stickers or tactile dots. Place one dot on the morning pill, two on the night pill. You can buy these online or ask your pharmacist to apply them. Some organizations, like RNIB, offer free tactile labeling kits. The goal is to use touch, not sight, to identify pills.
Are there apps that help with medication reminders for hearing loss?
Yes. Apps like Medisafe and MyTherapy offer visual alerts-flashing screen, vibrating phone, color-coded notifications. They can also send SMS reminders. If you have hearing loss, turn off sound alerts and rely on vibration and visual cues. Pair these with a pill organizer for best results.
Why don’t pharmacies automatically give accessible labels?
Because they’re not required to. There’s no federal law forcing pharmacies to provide large-print or braille labels. Medicare doesn’t pay extra for the time it takes. Most staff aren’t trained to recognize the need. It’s a systemic gap, not a lack of effort by individual pharmacists. That’s why asking directly is so important.
How do I know if a medication is expired if I can’t read the date?
Ask your pharmacist to write the expiration date in large, bold print on the bottle. Or use a tactile marker-place a small rubber band around the cap if it’s still good, remove it when expired. Some organizations offer free expiration date stickers with raised numbers. Never guess. Expired meds can be dangerous.
Can I get help from my local council or charity?
Yes. In the UK, RNIB and Action on Hearing Loss offer free home visits from occupational therapists who help set up medication systems. In the U.S., Area Agencies on Aging often provide similar services. These aren’t just advice-they’ll physically help you label your pills, set up reminders, and connect you with low-cost tools.






13 Comments
Just had my pharmacist slap a giant red sticker on my blood pressure bottle last week - ‘AM’ in 24-point font. Felt like I won the lottery. 🎉 No more guessing if that little white pill is for my heart or my sleep. Simple stuff, right? Why isn’t this standard? 😅
I work in elder care. We use rubber bands and color-coded sticky notes for 80% of our residents. No tech, no apps - just human ingenuity. The real win? When someone can independently identify their meds without needing someone to remind them every day. That’s dignity.
Let’s break this down. The 82% pill-handling stat? That’s misleading. It conflates ‘can pick up’ with ‘can identify correctly.’ The real crisis is in liquid dosing - which requires visuomotor integration, not just visual acuity. And 39% success with eye drops? That’s not a user error - it’s a design failure. The pharma industry still thinks ‘braille on the box’ is accessibility. It’s not. It’s performative.
What we need is tactile dosage indicators - raised ridges for mg levels, different textures for frequency. Think: Apple’s VoiceOver for pills. Not ‘tell me what it is’ - ‘feel what it is.’
Also, why are we still using glossy paper? Matte finishes reduce glare by 70%. Basic optics. But nope. Still shiny. Because ‘branding.’
And don’t get me started on the ‘record your own voice’ advice. What if you’re nonverbal? Or have dysarthria? Tech that assumes neurotypical ability is just exclusion with Wi-Fi.
Ugh. Another ‘poor disabled person’ sob story. Why can’t people just learn to use their phones? There’s an app for literally everything. If you can’t read a label, take a picture. Zoom in. Use Google Lens. It’s 2024. Stop asking for special treatment. This isn’t a privilege - it’s a basic life skill. 🤦♀️
Pharmacies don't care. They're overworked. And the FDA? Totally asleep. Also, braille? 15% of people who go blind later in life can read it? DUH. Nobody learns it after 50. So why even mention it? Waste of space. Just use big letters. And rubber bands. Done.
It is both lamentable and unsurprising that the discourse around pharmaceutical accessibility remains mired in sentimentalism rather than systemic reform. The notion that color-coding or rubber bands constitute a viable solution reflects a profound failure of regulatory imagination. One does not solve a structural inequity with Band-Aids - literal or metaphorical. The FDA must enforce standardized tactile and auditory labeling protocols, and manufacturers must be held liable for noncompliance. Until then, we are not providing care - we are performing charity.
Big Pharma doesn't want you to read your labels. They want you confused so you keep buying more pills. 🤫 The government is in on it. They don't want seniors to be independent - they want them dependent. That's why they won't make the labels accessible. It's about control. And don't even get me started on how the WHO is pushing this so the UN can track your meds. 👁️🗨️
My grandma in Texas uses a Sharpie and a highlighter. One color for her heart meds, another for her diabetes. She says it’s better than any app. She don’t trust phones. Said they ‘listen too much.’ 😅 She’s 82. Still drives. Still takes her pills right. Simple works.
Wait-so you’re telling me that after decades of ADA, we’re STILL relying on rubber bands and handwritten notes? This is a national disgrace. We have the technology. We have the funding. We have the legal obligation. And yet, we’re letting people risk their lives because… what? Because it’s ‘too expensive’? Because ‘pharmacists are busy’? That’s not an excuse-that’s negligence. And someone needs to be held accountable. NOW.
Hey - I’ve been using a Talking Rx for two years now. Best $40 I ever spent. My wife records the names, times, and even adds little pep talks: ‘You got this, honey!’ 😊 It’s not perfect, but it’s mine. And I don’t need anyone else to tell me what to take. That’s freedom. You’re not alone. We’re all figuring it out - one pill at a time.
Ask for large print. Ask for color coding. Ask for tactile dots. Don’t wait for permission. Most pharmacists will help - if you ask clearly and calmly. And if they say no? Ask for the manager. You have rights. Use them. Small steps lead to big changes.
This isn’t about medication. It’s about control. Who gets to decide what ‘accessible’ means? The people who need it? Or the corporations who profit from confusion? The entire system is designed to make you feel helpless - so you stay quiet. So you don’t demand more. So you accept rubber bands and whispered instructions like it’s a gift. But it’s not. It’s a demand for survival. And we’re not asking for charity - we’re demanding justice.
Every time someone says ‘just use your phone,’ they’re erasing the reality of disability. Not everyone has a smartphone. Not everyone can see the screen. Not everyone can hear the beep. Not everyone trusts technology. And that’s not weakness - that’s wisdom.
We are not broken. The system is.
Let’s reframe this: Medication safety isn’t a healthcare issue - it’s a philosophical one. What does it mean to live with dignity when the very tools meant to preserve your life are designed to exclude you? The pill bottle is a microcosm of society: indifferent, bureaucratic, and silent. We treat accessibility as an add-on - a nice-to-have. But it’s not. It’s the foundation. And until we see the label as sacred - not a label, but a lifeline - we’re not healing people. We’re just managing decline.
Write a comment