Every year, tens of thousands of seniors end up in the emergency room-not from falls, heart attacks, or infections-but because of a pill they were told to take. It’s not rare. It’s not an accident. It’s a predictable result of outdated prescribing habits and a lack of medication reviews. If you or a loved one is over 65 and taking five or more medications, you’re not alone. But you are at risk.
Why Seniors Are More Vulnerable to Medication Risks
As we age, our bodies change. The liver slows down. The kidneys filter less efficiently. Fat increases, muscle mass decreases. These changes mean drugs stick around longer, build up in the system, and hit harder. A dose that was fine at 50 can become dangerous at 75.Take zolpidem (Ambien), a common sleep aid. In younger people, it clears the body in 6-8 hours. In seniors, it can linger for over 11 hours. That means next-day drowsiness, confusion, and a much higher chance of falling. Studies show seniors on zolpidem have an 82% greater risk of falling than those on safer alternatives like trazodone. And it’s not just falls. Some seniors report sleepwalking, hallucinations, or waking up disoriented-sometimes with no memory of what happened.
Then there’s glyburide (Diabeta), a diabetes pill. It’s cheap. It’s been around for decades. But it’s also one of the most dangerous choices for older adults. While newer options like glipizide clear the body quickly, glyburide sticks around too long. That leads to low blood sugar-sometimes so severe it lands people in the hospital. Data from CMS shows glyburide causes 4.2 emergency visits per 100 patients each year. Glipizide? Less than half that.
The Beers Criteria: The Gold Standard for Safe Prescribing
If you’ve never heard of the Beers Criteria, you’re not alone. But every doctor who treats seniors should know it. First created in 1991 by Dr. Mark Beers, it’s now updated every two years by the American Geriatrics Society. The 2023 version lists 30 classes of medications and 14 individual drugs that should generally be avoided in older adults.These aren’t random lists. They’re based on real-world outcomes: hospitalizations, falls, confusion, kidney damage, even death. The criteria don’t say “never use.” They say, “Use only if absolutely necessary-and only after trying safer options.”
Here are the top offenders flagged in the 2023 update:
- First-generation antihistamines like diphenhydramine (Benadryl) and chlorpheniramine. These have a high anticholinergic burden, meaning they block a brain chemical critical for memory and focus. Long-term use increases dementia risk by 54%.
- Benzodiazepines like diazepam (Valium) and lorazepam (Ativan). Used for anxiety or sleep, they double the risk of falls and car crashes in seniors over 75.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen. These can cause stomach bleeds, kidney failure, and heart problems-even at low doses.
- Alpha-blockers like doxazosin and terazosin. Prescribed for prostate issues or high blood pressure, they cause dizziness and fainting in nearly 25% of seniors.
- Long-acting sulfonylureas like glyburide and chlorpropamide. These are the most dangerous diabetes pills for older adults.
- Meperidine (Demerol). An opioid that builds up toxic metabolites in the kidneys, triggering seizures in seniors.
- Nitrofurantoin (Macrobid). A common UTI drug that can cause fatal lung damage in people with reduced kidney function.
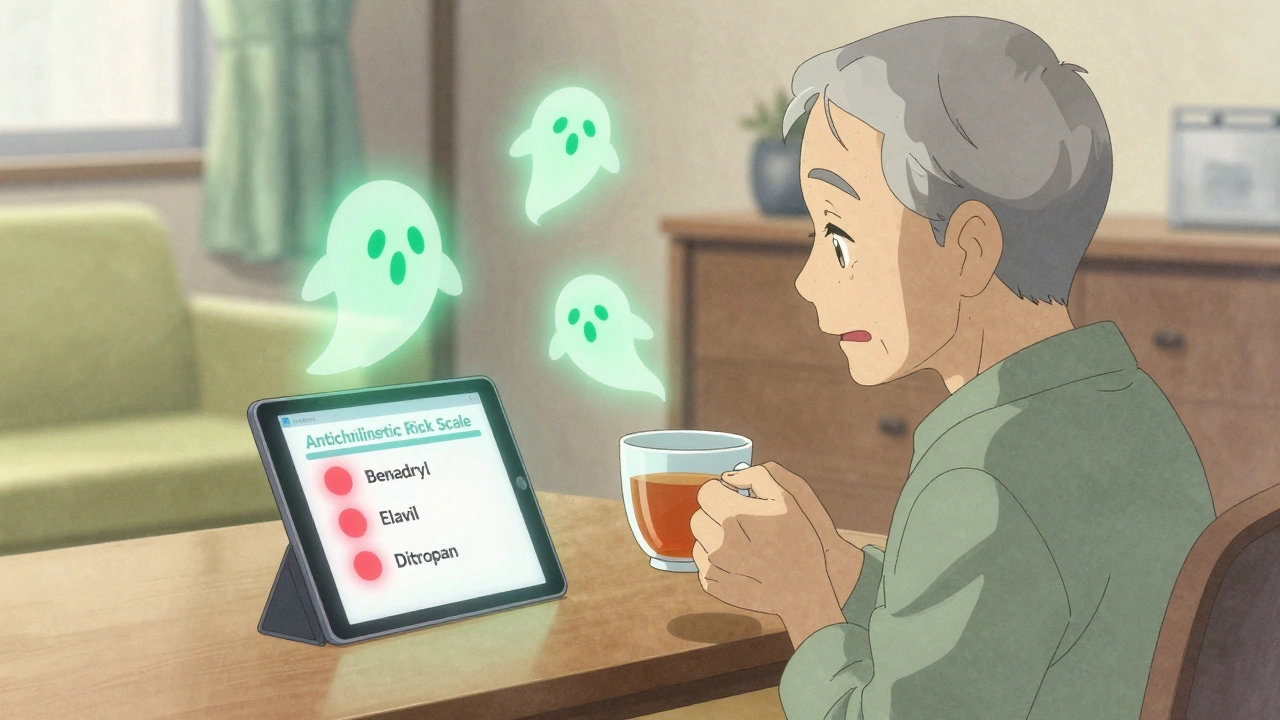
Anticholinergic Burden: The Silent Killer
One of the most overlooked dangers is anticholinergic burden. This isn’t about one drug. It’s about the total effect of all drugs a person takes that block acetylcholine-a key brain messenger.Many common medications have this effect, even if they’re not meant for the brain:
- Diphenhydramine (Benadryl)
- Trimethoprim-sulfamethoxazole (Bactrim)
- Amitriptyline (Elavil)
- Oxybutynin (Ditropan)
- Chlorpromazine (Thorazine)
When you add them up, the damage piles up. A score of 3 or higher on the Anticholinergic Risk Scale means high risk. A score of 5? That’s a red flag. One study found seniors with a cumulative score of 3+ had a 2.3 times higher risk of dementia over seven years.
And here’s the kicker: most seniors don’t realize they’re taking multiple anticholinergic drugs. One person might be on Benadryl for allergies, amitriptyline for nerve pain, and oxybutynin for bladder leaks. That’s three hits to the brain-all at once.
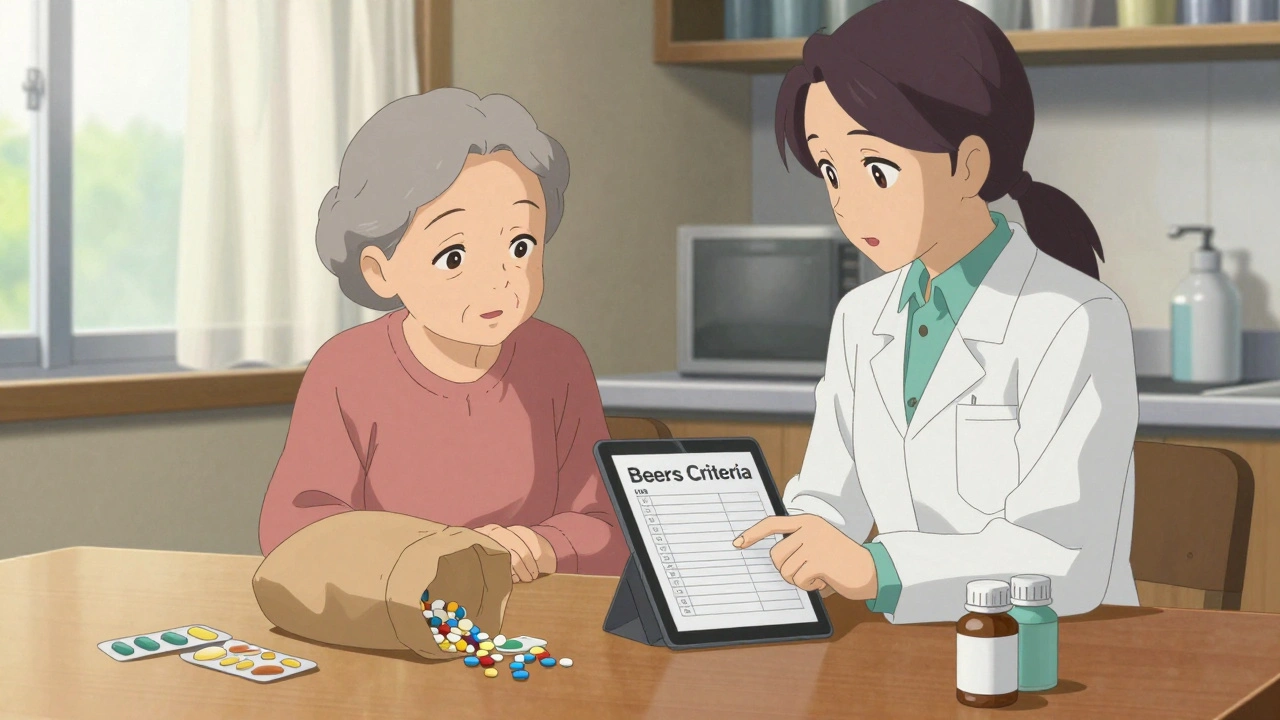
What to Do: How to Review Medications Safely
You don’t need to stop everything overnight. But you do need to ask questions.Start with a brown bag review. Take all your medications-pills, patches, liquids, even over-the-counter drugs-and bring them to your doctor or pharmacist. Don’t just say, “I’m taking my meds.” Show them. They’ll spot duplicates, interactions, and outdated prescriptions.
Ask these four questions:
- Why am I taking this? If the reason is vague-“It’s just what we’ve always done”-that’s a red flag.
- Is there a safer alternative? For sleep, try sleep hygiene or trazodone instead of zolpidem. For pain, acetaminophen (Tylenol) is often better than NSAIDs. For UTIs, nitrofurantoin can be swapped for fosfomycin if kidney function is low.
- Can I stop or reduce this? Many medications are prescribed for short-term use but kept for years. Think: muscle relaxants, sedatives, or even statins in very elderly patients with limited life expectancy.
- What happens if I don’t take this? Sometimes, the risk of the drug outweighs the benefit. That’s okay.
Pharmacists are your best allies. Studies show pharmacist-led medication reviews reduce high-risk drug use by over 34% in six months. They know the Beers Criteria inside out. Ask if your pharmacy offers a Medication Therapy Management (MTM) service-it’s free for Medicare Part D beneficiaries.
Real Stories, Real Changes
One 82-year-old woman in Ohio was on five medications: diphenhydramine for sleep, glyburide for diabetes, ibuprofen for arthritis, doxazosin for blood pressure, and oxybutynin for bladder leaks. She was falling once a week. Her memory was fading. Her doctor didn’t know she was taking Benadryl every night.After a brown bag review, her team switched her to melatonin, glipizide, acetaminophen, chlorthalidone, and a pelvic floor exercise program. Within six weeks, her falls stopped. Her confusion lifted. She started reading again.
Another man in Florida had been on amitriptyline for 15 years for nerve pain. He was constipated, dizzy, and forgetful. His pharmacist flagged the anticholinergic burden. They switched him to duloxetine. Within a month, his digestion improved. His energy came back. He didn’t need a cane anymore.
These aren’t miracles. They’re outcomes of a simple review.

What’s Changing in 2025
The system is catching up. Medicare Advantage plans now use the Beers Criteria to decide which drugs they cover. In 2024, CMS started tying 5% of bonus payments to how well plans reduce high-risk prescriptions. Electronic health records now pop up warnings when doctors try to prescribe glyburide or diphenhydramine to someone over 65.Still, awareness is low. A 2022 Kaiser Family Foundation survey found that 58% of seniors using high-risk medications didn’t know there were safer options. Only 32% had ever discussed the risks with their doctor.
That needs to change.
Medication safety isn’t about cutting pills. It’s about choosing better ones. It’s about asking, “Is this still helping me-or is it just keeping me company?”
What are the most dangerous medications for seniors?
The most dangerous medications for seniors include first-generation antihistamines like diphenhydramine (Benadryl), benzodiazepines like diazepam (Valium), long-acting sulfonylureas like glyburide, NSAIDs like ibuprofen, alpha-blockers like doxazosin, and nitrofurantoin in those with kidney issues. These drugs are flagged in the 2023 AGS Beers Criteria due to high risks of falls, confusion, low blood sugar, kidney damage, and even death.
How do I know if my meds are high-risk?
Check the Beers Criteria list, which is freely available online from the American Geriatrics Society. Look for drugs like diphenhydramine, glyburide, or benzodiazepines. Also, count your anticholinergic medications-if you’re taking three or more with anticholinergic effects, your risk is high. Ask your pharmacist to run a medication review using the Anticholinergic Risk Scale.
Can I stop these medications on my own?
No. Stopping some medications suddenly-especially benzodiazepines, antidepressants, or steroids-can cause serious withdrawal symptoms, seizures, or rebound conditions. Always work with your doctor or pharmacist. Tapering safely often takes 4-6 weeks and may include non-drug alternatives like cognitive behavioral therapy for insomnia or physical therapy for pain.
Are over-the-counter drugs safe for seniors?
Many are not. Diphenhydramine (Benadryl), sleep aids with antihistamines, and NSAIDs like ibuprofen are common OTC culprits. Even “natural” supplements like valerian root or melatonin can interact with prescription drugs. Always check with your pharmacist before starting any OTC product-even if it’s labeled “safe for seniors.”
How often should seniors have their medications reviewed?
At least once a year, but every 3-6 months is better if you’re on five or more medications, have recently been hospitalized, or have new symptoms like dizziness, confusion, or falls. Medicare Part D offers free Medication Therapy Management (MTM) services for eligible beneficiaries-take advantage of it.
What’s the best alternative to glyburide for seniors with diabetes?
Glipizide is the preferred alternative. It’s a second-generation sulfonylurea with a much lower risk of prolonged low blood sugar. Other safer options include metformin (if kidney function allows), SGLT2 inhibitors like empagliflozin, or GLP-1 receptor agonists like semaglutide. These not only lower blood sugar more safely but also protect the heart and kidneys.
Do all doctors know about the Beers Criteria?
Not all. While most primary care physicians and geriatricians use it, specialists often don’t. A 2023 survey found only 68% of cardiologists and 54% of neurologists regularly check the Beers list when prescribing. Don’t assume your doctor knows. Bring the list yourself. Ask: “Is this on the Beers Criteria? Is there a safer option?”
Next Steps: What to Do Today
1. Collect all medications-prescription, OTC, vitamins, supplements. Put them in a bag.2. Call your pharmacist and ask for a free medication review. Mention the Beers Criteria.
3. Schedule a visit with your doctor. Bring the bag. Ask the four key questions.
4. Write down your goals. Do you want to sleep better? Stop falling? Think more clearly? Let those guide the changes.
5. Follow up in 30 days. Did the new plan help? Any side effects? Adjustments may be needed.
Medications aren’t harmless. They’re powerful tools. But like any tool, they can hurt if used the wrong way. For seniors, the stakes are higher. A simple review today could mean months of safety, independence, and peace of mind tomorrow.



8 Comments
Whoa, this is insane-I just found out my grandpa’s been on Benadryl every night for 10 years!!! And he’s been falling like a sack of potatoes!!! I’m taking his meds to the pharmacist tomorrow-no more “just a little help sleeping”!!!
The Beers Criteria has been around since 1991 and yet primary care physicians still prescribe glyburide like it’s aspirin. This is not negligence-it’s institutional laziness. The data is clear, the guidelines are published, and the consequences are fatal. Yet nothing changes. The system is broken.
OMG this is SO important!!! I just had my 78-year-old mom switch from Ambien to trazodone and she’s been sleeping like a baby without the zombie mode!!! Also dropped the ibuprofen for Tylenol-no more dizzy spells!!! You guys NEED to do a brown bag review!!! It’s FREE!!! And your grandma will thank you!!! 🙌💊
Actually, you’re all missing the real issue. It’s not the meds-it’s the damn doctors who don’t listen. My uncle was on doxazosin for 8 years and no one ever asked why. He got dizzy, fell, broke his hip-and the doctor just upped his blood pressure med. Like, what?!? You think the system’s gonna fix itself? It won’t. You gotta fight for your own health. Every. Single. Time.
As an Australian, I’m genuinely impressed by how detailed this is. We have similar guidelines here-the STOPP/START criteria-but they’re not nearly as widely promoted. The anticholinergic burden point is critical. My mother-in-law was on three anticholinergics-Benadryl, oxybutynin, and amitriptyline-and her cognitive decline was terrifying. Switching her out took six months, but she’s back to gardening and crossword puzzles. Patience and persistence win.
This isn’t just about medication safety-it’s about dignity. Every pill we take is a choice. A choice between comfort and consequence. For too long, we’ve treated aging as a disease to be managed with more drugs, not a life to be lived with clarity. The fact that a 75-year-old woman can stop Benadryl, regain her memory, and start reading again? That’s not a medical miracle. That’s justice. That’s what happens when we finally listen to the body instead of the prescription pad. We owe our elders more than convenience. We owe them awareness.
Wait… so you’re telling me Big Pharma is secretly pushing these dangerous drugs on seniors?? I knew it!! My aunt’s doctor always pushes the cheapest meds-but what if they’re just testing them on old people?? Like, what if they’re using us as guinea pigs?? And why does Medicare still cover glyburide?? Something’s not right… I’m calling the FDA. 👁️🗨️💊
Thank you for this comprehensive and meticulously referenced exposition. The integration of clinical guidelines, epidemiological data, and patient-centered narratives elevates this from a cautionary article to a public health imperative. I would further recommend that all primary care practices implement automated Beers Criteria alerts within their electronic health record systems, and that Medicare Advantage plans be mandated to report quarterly metrics on high-risk medication reduction. The data is unequivocal; the moral obligation is clear.
Write a comment