Renal Dosing Calculator
This tool helps determine appropriate dosing for metformin and SGLT2 inhibitors based on your kidney function (eGFR). Always consult your healthcare provider for medical advice.
When you’re managing type 2 diabetes and your kidneys aren’t working as well as they should, the medications you take need to change. It’s not just about lowering blood sugar anymore-it’s about protecting your kidneys, avoiding dangerous side effects, and making sure your drugs still work without harming you. Two of the most important diabetes drugs-metformin and SGLT2 inhibitors-require careful dosing adjustments based on kidney function. Get this wrong, and you risk lactic acidosis, acute kidney injury, or missing out on life-saving protection for your kidneys.
Why Kidney Function Matters More Than Ever
Your kidneys filter waste, regulate fluids, and help control blood pressure. When they’re damaged-common in people with long-standing diabetes-your body can’t clear drugs like metformin or SGLT2 inhibitors the same way. That means they build up, increasing the risk of side effects. But here’s the twist: these drugs aren’t just safe to use in kidney disease anymore. They’re now some of the best tools we have to slow kidney damage. The old rule-stop metformin if your eGFR drops below 60-doesn’t apply anymore. And SGLT2 inhibitors? They’re no longer just for people with healthy kidneys. New evidence shows they protect the kidneys even when function is already low. The big shift came from major trials like DAPA-CKD, EMPA-KIDNEY, and CREDENCE, which showed these drugs reduce the risk of kidney failure and heart death by 30-40% in people with chronic kidney disease (CKD). That’s not a small benefit. It’s a game-changer.Metformin: How Much Is Safe?
Metformin is still the first-line drug for type 2 diabetes, even with kidney issues. But you can’t take the same dose if your kidneys are struggling. The guidelines now use your estimated glomerular filtration rate (eGFR)-a blood test that measures how well your kidneys filter waste-to decide your dose.- eGFR ≥60 mL/min/1.73 m²: You can take the full dose-up to 2550 mg per day.
- eGFR 45-59 mL/min/1.73 m²: Cut it back to 2000 mg per day max.
- eGFR 30-44 mL/min/1.73 m²: Maximum is 1000 mg per day. Don’t go higher.
- eGFR <30 mL/min/1.73 m²: Stop metformin. It’s contraindicated.
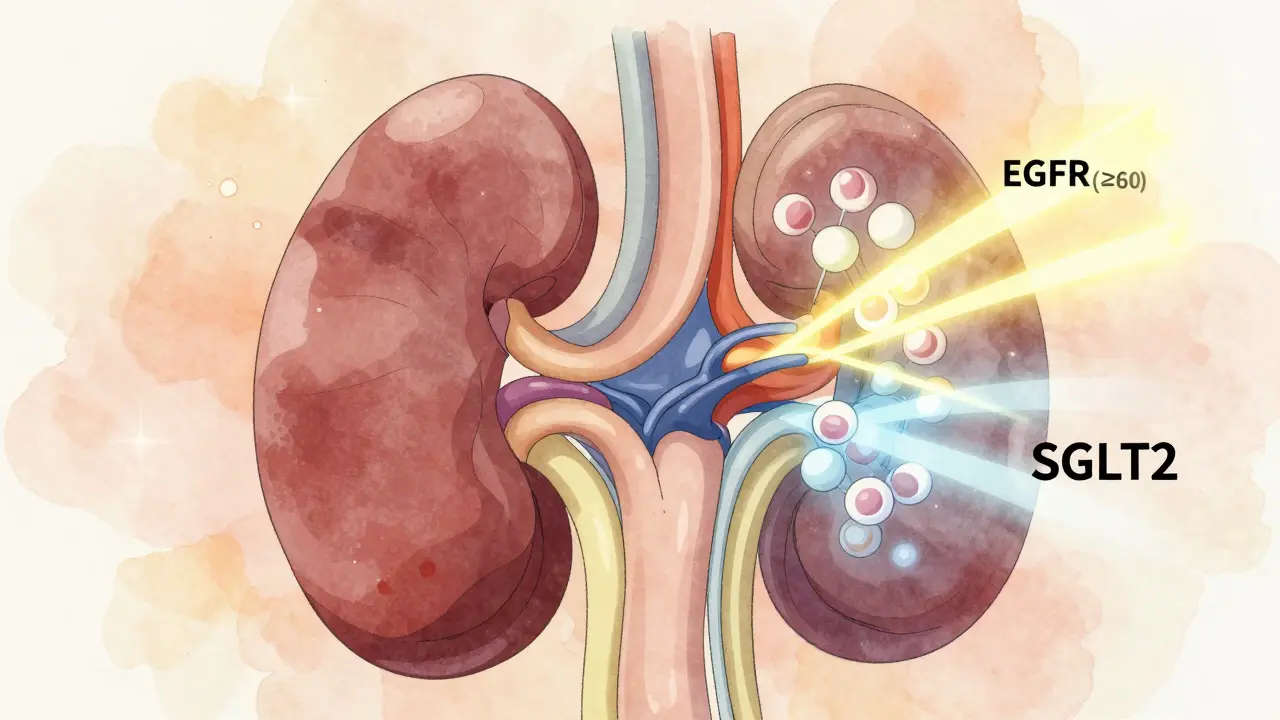
SGLT2 Inhibitors: The Kidney Protectors
SGLT2 inhibitors-like dapagliflozin, empagliflozin, and canagliflozin-are different. They don’t just lower blood sugar. They reduce protein in the urine, lower blood pressure in the kidneys, and slow the progression of kidney disease. That’s why guidelines now say: start them earlier, not later. The 2022 KDIGO guidelines made a bold move: they lowered the minimum eGFR threshold for starting an SGLT2 inhibitor from 30 to 20 mL/min/1.73 m². That means if your kidneys are working at 25% of normal, you can still benefit from these drugs. And once you start them, you usually keep them-even if your eGFR drops further, as long as you’re not having side effects or needing dialysis. Here’s how dosing breaks down by drug:| Drug | eGFR ≥60 | eGFR 45-59 | eGFR 30-44 | eGFR 20-29 | eGFR <20 |
|---|---|---|---|---|---|
| Canagliflozin | 100-300 mg | ≤100 mg | Contraindicated | Contraindicated | Contraindicated |
| Dapagliflozin | 5-10 mg | 5-10 mg | 5-10 mg | 5-10 mg | Contraindicated |
| Empagliflozin | 10-25 mg | 10-25 mg | ≤10 mg | ≤10 mg | Contraindicated |
The Narrow Window: eGFR 20-29
This is where things get tricky. If your eGFR is between 20 and 29 mL/min/1.73 m²:- You can still take an SGLT2 inhibitor (dapagliflozin or empagliflozin at full dose).
- You should stop metformin-it’s no longer safe.
What About That Initial eGFR Drop?
When you start an SGLT2 inhibitor, your eGFR often drops by 2-5 mL/min/1.73 m² in the first few weeks. That’s normal. It’s not kidney damage-it’s the drug working. SGLT2 inhibitors reduce pressure in the kidney’s filtering units, which temporarily lowers the eGFR reading. Think of it like a pressure relief valve. Don’t panic. Don’t stop the drug. Wait three months. In most cases, the eGFR stabilizes-and your proteinuria (protein in urine) drops. That’s the real sign of kidney protection. The UK Kidney Association says it clearly: “A decline in eGFR needs to be interpreted with caution and in the context of an expected drug effect.”Monitoring: How Often Should You Get Tested?
You can’t set it and forget it. Regular kidney checks are non-negotiable.- Metformin users:
- eGFR ≥60: every 6-12 months
- eGFR 45-59: every 3-6 months
- eGFR 30-44: every 3 months
- SGLT2 inhibitor users:
- Check eGFR before starting
- Check again at 4-12 weeks after starting
- Then every 3-6 months, or more often if eGFR is below 45
What Happens When You Need Dialysis?
For patients on hemodialysis or peritoneal dialysis, guidelines are less clear. But here’s what we know:- Metformin: Not recommended. The risk of buildup is too high. Some centers use 250 mg daily on peritoneal dialysis or 500 mg after hemodialysis-but only under strict supervision.
- SGLT2 inhibitors: Not effective. These drugs need working kidneys to work. Once you’re on dialysis, they’re stopped.
Insurance, Labels, and Real-World Confusion
Here’s the ugly truth: guidelines and drug labels don’t always match. The FDA still says canagliflozin is contraindicated if eGFR is below 45. But KDIGO and ADA say it’s safe down to 20. So what happens? A 2022 survey found that 43% of endocrinologists had insurance claims denied for SGLT2 inhibitors when prescribed to patients with eGFR between 20 and 29. That’s not because the drug doesn’t work. It’s because the payer’s system only sees the FDA label. Doctors are caught in the middle. Some follow the label to avoid liability. Others follow the evidence to protect their patients. The KDIGO guidelines say it plainly: “Clinicians should follow evidence-based clinical practice guidelines rather than regulatory labeling when they conflict.”What’s Next?
The field is moving fast. In February 2024, the FDA approved dapagliflozin for chronic kidney disease even in people without diabetes-based on the same trials that showed kidney protection. That’s huge. It means these drugs are becoming standard for kidney disease, not just diabetes. The ADA and KDIGO are already working on a 2025 update. Early drafts are looking at whether SGLT2 inhibitors can be used safely in patients with eGFR as low as 15-19 mL/min/1.73 m². That’s the next frontier. For now, the message is clear: don’t let kidney disease stop you from getting the best diabetes care. With the right dosing and monitoring, metformin and SGLT2 inhibitors can keep your blood sugar under control while protecting your kidneys for years to come.Can I take metformin if my eGFR is 35?
Yes, but only at a reduced dose of 1000 mg per day or less. eGFR between 30 and 44 mL/min/1.73 m² is the last safe range for metformin. You should monitor kidney function every 3 months and avoid the drug if you’re dehydrated, sick, or having surgery.
Should I stop my SGLT2 inhibitor if my eGFR drops from 30 to 25?
No. A drop of 5 mL/min/1.73 m² in the first few months is normal and expected with SGLT2 inhibitors. It doesn’t mean your kidneys are getting worse-it means the drug is working. Continue the medication unless you have symptoms of dehydration, low blood pressure, or your eGFR falls below 20.
Can I take both metformin and an SGLT2 inhibitor together?
Yes, and it’s often the best combination. For eGFR ≥45, both drugs can be used safely at full doses. For eGFR 30-44, you can still take both, but metformin must be capped at 1000 mg. For eGFR 20-29, you should stop metformin and keep the SGLT2 inhibitor. This combination reduces kidney failure risk by up to 40%.
Why do some doctors refuse to prescribe SGLT2 inhibitors below eGFR 45?
Many doctors follow the FDA-approved drug labels, not clinical guidelines. Canagliflozin’s label says it’s contraindicated below eGFR 45, even though KDIGO and ADA say it’s safe down to 20. Some doctors fear legal risk or insurance denials. Others haven’t kept up with the latest evidence. Always ask your doctor why they’re making a decision-especially if it goes against current guidelines.
Is it safe to use SGLT2 inhibitors if I have heart failure?
Yes-in fact, SGLT2 inhibitors are now recommended for people with heart failure, even without diabetes. Trials like DAPA-HF and EMPEROR-Reduced showed these drugs reduce hospitalizations and death from heart failure. They’re safe and effective in patients with eGFR ≥20, regardless of heart function.




13 Comments
Metformin dosing adjustments based on eGFR are well-documented and clinically sound. The 2022 KDIGO guidelines reflect a significant evolution in nephrology practice. Clinicians must prioritize evidence over outdated institutional protocols.
OMG this is SO important!! 🙌 I had no idea SGLT2 inhibitors could still work when eGFR drops to 20!! My dad’s on dapagliflozin and his kidneys are at 24-he’s been doing AMAZING. Please don’t stop these meds just because a label says so!! 💪🩺
The epistemological shift in renal pharmacology, as articulated herein, constitutes a paradigmatic rupture from the reductionist paradigms of prior therapeutic dogma. The ontological status of eGFR as a biomarker has been reconfigured by empirical evidence, rendering regulatory labeling an epiphenomenon rather than a normative authority. One is compelled to interrogate the moral economy of pharmaceutical governance in light of such clinical triumphs.
There’s something profoundly beautiful about how medicine is finally catching up with biology. SGLT2 inhibitors don’t just lower glucose-they recalibrate the kidney’s internal environment. That drop in eGFR? It’s not failure. It’s adaptation. Think of it like a dam releasing pressure to prevent a catastrophic breach. We’ve been misreading the signs for decades. This is why I love being a clinician today.
I’ve seen this play out in clinic-patients panic when their eGFR drops 5 points after starting an SGLT2i. But their proteinuria plummets. Their BP stabilizes. Their hospitalizations drop. The numbers lie if you don’t look at the whole picture. Why do we still treat lab values like gospel instead of clues?
So you're telling me the FDA is wrong and some fancy study is right? I'm sure the drug companies paid those researchers. Also why are we even giving meds to people with kidneys this bad? Maybe they should just die faster
Wait. So. If you’re on dialysis… you stop the SGLT2i… but if your eGFR is 25… you keep it? And metformin is bad at 35… but okay at 36? This is insane. Who decided this? What if I’m on vacation in Mexico and my lab results are delayed? I could die. I’m terrified now.
Another overcomplicated article. Just tell me what to do. Also, why are there 7 different dosing charts? This is why people don’t trust doctors.
These guidelines are a disgrace to American medicine. In the good old days, we didn’t give dangerous drugs to people with failing kidneys. Now we’re letting foreign studies dictate our practice. This is why our healthcare system is collapsing.
Man, this is the kind of stuff I wish my doc explained like this. I’ve got eGFR at 38 and was scared to take metformin. Now I know I can still take 1000mg. Also, my SGLT2i made my eGFR drop a bit at first-thought I was dying. Turns out it was just the drug doing its job. Thanks for clearing that up.
okay so i think this is all a lie because the cia controls the fda and the kidney studies are funded by big pharma and they want us to take these drugs so they can sell more insulin and also the moon landing was faked so maybe the eGFR test is fake too??
I can't believe we're still talking about this. I mean, really? We have a whole system built on numbers that change based on who you are, where you live, what time of day, and whether your lab uses the same calibration as the next one. And now we're supposed to trust a 2022 guideline? What about the 2018 one? The 2015 one? This is why people don't trust medicine anymore. It's all just shifting sand. And don't even get me started on insurance.
India has better kidney care than the US. We don’t need these fancy American guidelines. Our traditional medicine has been treating diabetes for centuries. Why are we listening to Western science that changes every year? This is cultural imperialism.
Write a comment