Every year, thousands of patients in the U.S. get the wrong medication-not because the pharmacist made a mistake with the pill, but because they gave it to the wrong person. This isn’t rare. It’s systemic. And the fix? Simple, but often ignored: use two patient identifiers before handing out any prescription.
Why Two Identifiers? It’s Not Just a Rule-It’s a Lifesaver
The Joint Commission, the group that accredits U.S. hospitals and pharmacies, made this rule official back in 2003. NPSG.01.01.01 says: Never rely on just one thing to confirm who a patient is. That means no more just asking, “Are you John Smith?” and assuming the answer is yes. You need two pieces of information that are unique to that person-like their full name and date of birth. Or name and medical record number. Or name and phone number. Room numbers? No. Diagnosis codes? No. Even “the guy in bed 3” isn’t enough. Those can change. Those can be wrong. And when they are, someone could get a drug they’re allergic to, a double dose, or a medication that clashes with something they’re already taking. A 2020 study in JMIR Medical Informatics found that up to 10% of serious drug interaction alerts get missed because systems can’t link a patient’s full history. That’s about 6,000 people a year getting dangerous combinations because their records were split across systems-or worse, because a pharmacist didn’t check the right name.What Counts as a Valid Identifier?
Not everything you think is unique actually is. Here’s what The Joint Commission says works:- Full legal name (first and last)
- Date of birth
- Assigned medical record number
- Telephone number
- Other unique personal identifiers (like a national ID if used locally)
- Room number
- Location (e.g., “the woman in aisle 2”)
- Diagnosis
- Prescription number
- Insurance ID
Manual Checks Alone Aren’t Enough
You might think, “I just ask the patient twice-name and DOB. That’s fine.” But human memory is messy. People forget their birth year. They give nicknames. They say “I’m John Smith” when they’re actually Jonathan Smith from the next town. And in a busy pharmacy, especially during lunch rush or flu season, staff get tired. They start skipping steps. A 2023 survey by the American Society of Health-System Pharmacists (ASHP) found that 63% of pharmacists admitted to occasionally cutting corners on verification because of time pressure. In community pharmacies, 42% said verification often happens verbally-with no written record. That’s a problem. If there’s no documentation, there’s no accountability. And if there’s no accountability, mistakes slip through. One real case from Imprivata in 2023 involved a patient transferred from another hospital. He was unconscious. The receiving hospital couldn’t find his record because he was registered under his middle name, not his first. They created a new file. Days later, they discovered he had a documented penicillin allergy-right in his old record. If the pharmacy had checked two identifiers properly, they’d have found it.Technology Makes It Faster and Safer
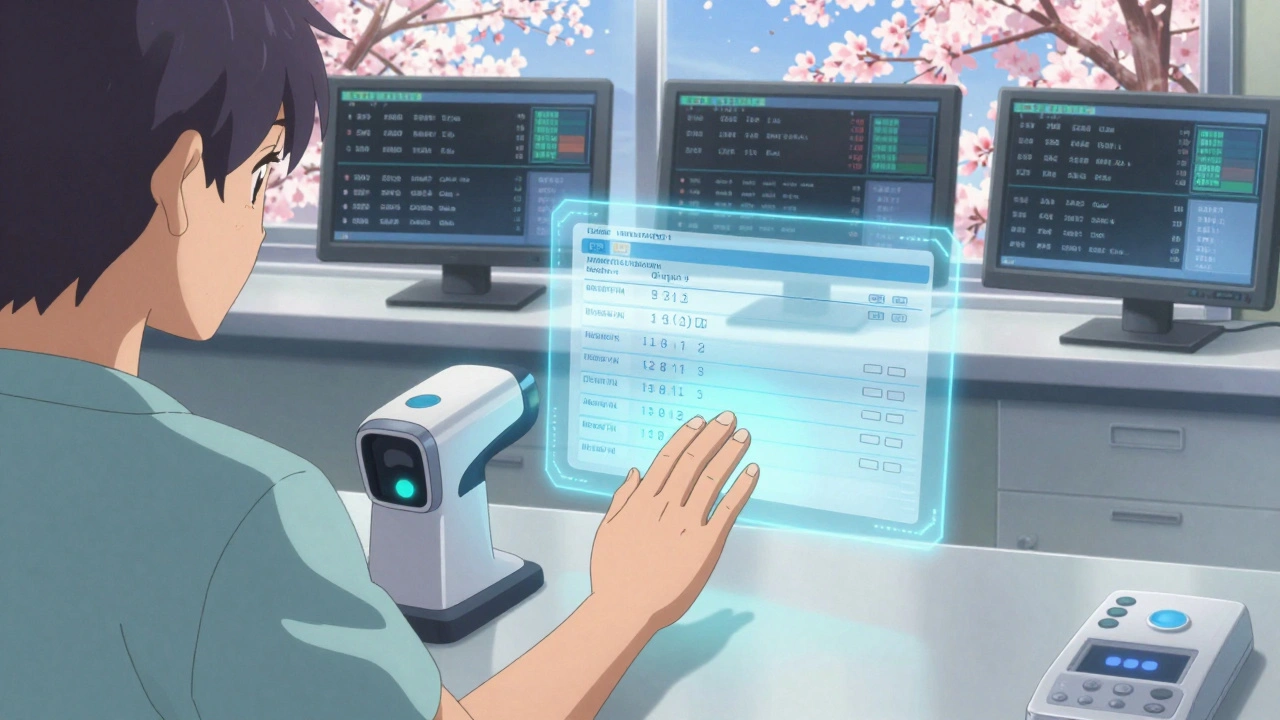
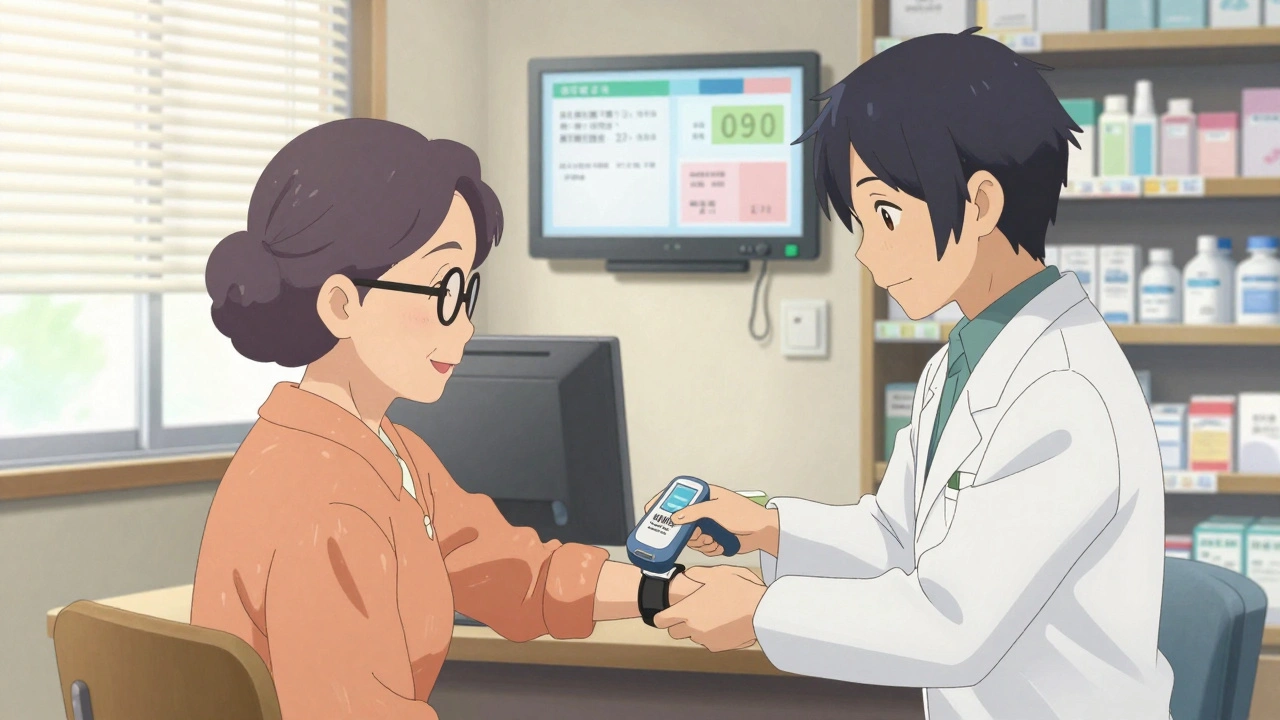
The best way to fix this isn’t by yelling at staff to be more careful. It’s by making it impossible to skip the check. Barcode scanning is the gold standard. When a pharmacist pulls a prescription, they scan the patient’s wristband (with name and MRN encoded) and the medication’s barcode. The system cross-checks: Is this the right drug? Is it for this patient? Is the dose correct? If anything’s off, it stops. A 2012 study in the Journal of Patient Safety showed that hospitals using barcode systems saw a 75% drop in medication errors reaching patients. That’s not a small win. That’s life-or-death. Even better? Biometric systems. Companies like Imprivata PatientSecure use palm-vein scanning. No one shares your vein pattern. No one can fake it. A 2024 Altera Health survey found these systems match patients to records 94% of the time. Compare that to hospitals without good systems-only 17% accuracy. And here’s the kicker: biometric verification takes under 10 seconds. Faster than asking two questions. And it doesn’t rely on the patient being awake, coherent, or honest.
What About Double Checking by Two People?
You’ve probably heard: “Have two pharmacists check the prescription.” Sounds safe, right? Turns out, it doesn’t work as well as you think. A 2020 review in BMJ Quality & Safety looked at 18 studies on double-checking. Result? No solid proof it reduces errors. Why? Because if both people are looking at the same screen, reading the same name, and trusting the same system-they’re likely to miss the same mistake. Independent double-checking only works if the second person doesn’t just nod along. And most times, they don’t. Technology doesn’t replace human judgment. But it removes the chance for human error to creep in at the verification stage.Why Do Pharmacies Still Get It Wrong?
There are three big reasons:- Duplicate records: A patient visits five different clinics. Each one creates a new file. Now there are three “John Smiths” in the system. One has allergies. One has diabetes. One has a history of substance use. If the pharmacy pulls the wrong one, disaster follows.
- Legacy systems: Many pharmacies still use old software that doesn’t talk to each other. No Enterprise Master Patient Index (EMPI) means no central record. No EMPI = 8-12% of patient records are duplicated or mismatched. That’s not a glitch. That’s the norm in underfunded systems.
- Staff burnout: Community pharmacists are stretched thin. One study showed pharmacists spend 40% of their day on administrative tasks. When you’re rushing, skipping a step feels harmless. Until it’s not.
How to Implement This Right
If you’re in charge of a pharmacy, here’s how to do it without chaos:- Start with policy. Write down exactly which two identifiers you’ll use-and which ones are banned. Make it clear. Post it.
- Train everyone. Not just pharmacists. Techs, cashiers, even the person who hands out pickup bags. Everyone touches the process.
- Pilot it. Try it in one section for a month. Track near-misses. See where it breaks.
- Go tech-heavy. If you can’t afford biometrics, start with barcode scanners. They’re affordable, proven, and easy to integrate.
- Document everything. The Joint Commission found that 37% of non-compliant pharmacies didn’t even record the verification. That’s not safety. That’s negligence.
What Happens If You Don’t?
The Joint Commission doesn’t just say “please.” They enforce it. In 2023, non-compliance with two-identifier rules was the third most common violation in hospital surveys. That’s not a footnote. That’s a red flag. Lose accreditation? You lose Medicare and Medicaid payments. That’s not just money. That’s survival. And the cost of a single error? A patient dies. Or goes blind. Or loses a limb from a wrong drug. The financial cost? Up to $40 million a year per large hospital system just to fix duplicate records and clean up errors.The Future Is Unique Identifiers
The Office of the National Coordinator for Health IT is running a pilot in early 2025 to test a national, voluntary patient identifier system. Think of it like a Social Security number for health records-unique, secure, and linked across all providers. Right now, we’re stuck with patchwork systems. But the data is clear: without a single, reliable identifier, we’re just guessing who’s who. And guessing with medications? That’s not risk management. That’s gambling. The American Medical Informatics Association says a national system could catch up to 9.7% more dangerous drug interactions. That’s thousands of people spared harm every year.Bottom Line: This Isn’t Optional
Using two patient identifiers isn’t bureaucracy. It’s basic science. You wouldn’t give insulin to someone without checking their blood sugar. You wouldn’t give an antibiotic without knowing the infection. So why give a pill without knowing the person? The tools are here. The data proves it works. The cost of doing nothing is too high. If you’re a pharmacist: scan the wristband. Say the name. Confirm the birthdate. Write it down. If you’re a patient: Don’t be shy. Ask, “Are you sure this is for me?” Because in a pharmacy, the difference between safety and disaster isn’t a fancy algorithm. It’s two questions. And the courage to ask them.What are the two patient identifiers required in a pharmacy?
The two patient identifiers must be unique to the individual and directly tied to their identity. Acceptable identifiers include the patient’s full name and date of birth, full name and medical record number, or full name and telephone number. Room numbers, diagnoses, insurance IDs, or prescription numbers are not valid because they don’t uniquely identify the person.
Why is using only one identifier dangerous in a pharmacy?
Using only one identifier, like a last name, can lead to misidentification-especially if multiple patients share similar names or demographics. This can result in giving the wrong medication, incorrect dosage, or a drug that interacts dangerously with another the patient is already taking. Studies show up to 10% of serious drug interaction alerts go undetected due to poor identification, putting thousands at risk annually.
Can a pharmacist just ask the patient their name and assume it’s correct?
No. Patients may give nicknames, forget their birth year, or even accidentally confirm the wrong identity due to confusion, stress, or cognitive impairment. Relying solely on verbal confirmation without a second, objective identifier (like a medical record number or date of birth) increases the risk of error. Documentation of both identifiers is required for compliance and safety.
Do barcode scanning systems really reduce medication errors?
Yes. Studies show barcode scanning systems reduce medication errors reaching patients by up to 75%. These systems match the patient’s wristband barcode with the medication’s barcode and the electronic prescription. If anything doesn’t align-wrong patient, wrong drug, wrong dose-the system alerts the pharmacist before dispensing, preventing errors before they happen.
What happens if a pharmacy doesn’t follow the two-identifier rule?
Non-compliance with The Joint Commission’s two-identifier requirement is one of the top three most common violations in hospital and pharmacy surveys. This can lead to loss of accreditation, which affects Medicare and Medicaid reimbursement. Beyond financial penalties, failure to comply puts patients at risk of serious harm or death due to medication errors, which can result in legal liability and reputational damage.
Are there any new technologies improving patient identification in pharmacies?
Yes. Biometric systems like palm-vein scanning (e.g., Imprivata PatientSecure) offer 94% accuracy in matching patients to records, far exceeding manual methods. Enterprise Master Patient Index (EMPI) systems help eliminate duplicate records by linking all patient data across departments. In 2025, pilot programs are testing a national unique patient identifier to improve interoperability and reduce errors caused by fragmented records.
Why is documentation of the two identifiers important?
Documentation proves that verification occurred. Without it, there’s no way to audit compliance or investigate errors. The Joint Commission found that 37% of non-compliant pharmacies failed to document the identifiers used. This isn’t just paperwork-it’s legal and safety protection for both the patient and the pharmacy.



9 Comments
So let me get this straight: we’re still letting pharmacists guess who’s who in 2025? 🤦♀️. I got my blood pressure med last week and they asked if I was ‘Sarah’-I said ‘Lauren.’ They said, ‘Oh, right, sorry.’ No second check. No barcode. No shame. Just… luck.
Safety is not a suggestion. It is a sacred duty. Every human life is a miracle, and we must honor it with every step we take. When we fail to verify identity, we do not just risk error-we risk the soul of care itself. Let us choose compassion over convenience.
This whole post is just a glorified compliance checklist. Nobody cares about your Joint Commission rules. The real problem is lazy staff and broken IT systems. Stop pretending paperwork fixes human failure. You need to fire people who skip steps, not install more scanners.
OMG I CAN’T BELIEVE WE’RE STILL TALKING ABOUT THIS!! Like duh, scan the wristband!! My cousin got the wrong antibiotic because they just asked his name and he said ‘yeah’-he was half-asleep!! We need to BAN verbal checks!! #pharmacyfail #america
The notion that technology can replace human judgment is dangerously naive. Biometrics may be accurate, but they do not confer wisdom. A system that prevents error without understanding context is not safety-it is automation masquerading as care.
YESSSS this is so important!! 🙌 I work in a clinic and we just got barcode scanners last month-GAME CHANGER. My grandma almost got a double dose of warfarin last week because the system flagged it. She’s alive today because tech didn’t let us mess up. Keep pushing this!! 💪❤️
Wait, you mean you actually have to ask for DOB and name? I thought you just looked at the picture on the insurance card. That’s what I’ve always done. And I’ve never messed up. Why is everyone making this so complicated?
Australia’s been using unique patient identifiers since 2015. No duplicates. No confusion. No ‘I think that’s John Smith’ nonsense. We still have human errors, yes-but not because of bad identification. The tech works. The culture supports it. The result? Fewer deaths. Simple.
Let’s remember: this isn’t about rules. It’s about people. That elderly woman who forgot her birthday? The teenager who’s nervous and says ‘yes’ to everything? The immigrant who doesn’t speak English well? They’re not failing the system. The system is failing them. We need tech that meets people where they are-not just scans and checklists. A barcode won’t help someone who’s scared. But a pharmacist who takes a breath and asks again? That saves lives.
Write a comment