Steroid Withdrawal Risk Calculator & Tapering Guide
Risk Assessment
This tool helps you determine if you're at risk of adrenal insufficiency after stopping corticosteroids and provides a personalized tapering schedule if needed.
Stopping corticosteroids like prednisone or dexamethasone suddenly can trigger a medical emergency you might never see coming. If you’ve been on these drugs for weeks or even months, your body stops making its own cortisol. When you cut the medication off too fast, your adrenal glands can’t snap back in time - and that’s when things turn dangerous.
Why Your Body Can’t Handle a Sudden Stop
Corticosteroids mimic cortisol, the hormone your adrenal glands make to handle stress, regulate blood pressure, and keep your metabolism running. When you take them for more than a few weeks, your brain gets the message: "We’ve got enough cortisol. Stop making it." Over time, your adrenal glands shrink from lack of use. They don’t just slow down - they go quiet. This isn’t just a problem for people on high doses. Even low-dose prednisone - as little as 5 mg a day - taken for more than four weeks can shut down your natural cortisol production. A 2023 study in Endocrine Abstracts confirmed this. Many patients think they’re safe if they were on steroids for a short time after a cold or flare-up. They’re wrong. The risk is real, even with short courses.What the Symptoms Look Like - And How They’re Mistaken
The early signs of adrenal insufficiency are easy to brush off. You feel tired - really tired. Not just "I stayed up late" tired. More like "I can’t get out of bed" tired. About 85% of people report this as their first symptom. Then comes loss of appetite, nausea, dizziness, muscle weakness, and mood changes like irritability or depression. These symptoms often get misdiagnosed. A 2023 case report described a woman who went to the ER with vomiting and fatigue after stopping dexamethasone. Doctors thought it was a urinary tract infection. It wasn’t. Her blood pressure kept dropping. She was in adrenal crisis. Only when someone asked about her steroid history did they realize what was happening. Sixty-eight percent of patients on online forums say their symptoms were blamed on something else - the flu, anxiety, chronic fatigue, even depression. By the time they get the right diagnosis, they’re often hospitalized. The average delay is over three weeks. That’s three weeks of your body slowly shutting down.When It Turns Critical - Adrenal Crisis
If you ignore the early signs, you risk adrenal crisis. This is life-threatening. Your blood pressure plummets. You become dehydrated. Your electrolytes go haywire. You might feel confused, faint, or slip into a coma. Without treatment, 6% of people in the hospital with adrenal crisis die. Symptoms usually show up 24 to 72 hours after your last dose. But they can hit faster if you’re under stress - an infection, surgery, or even a bad car accident. Your body needs cortisol to handle stress. If you don’t have any, it can’t fight back.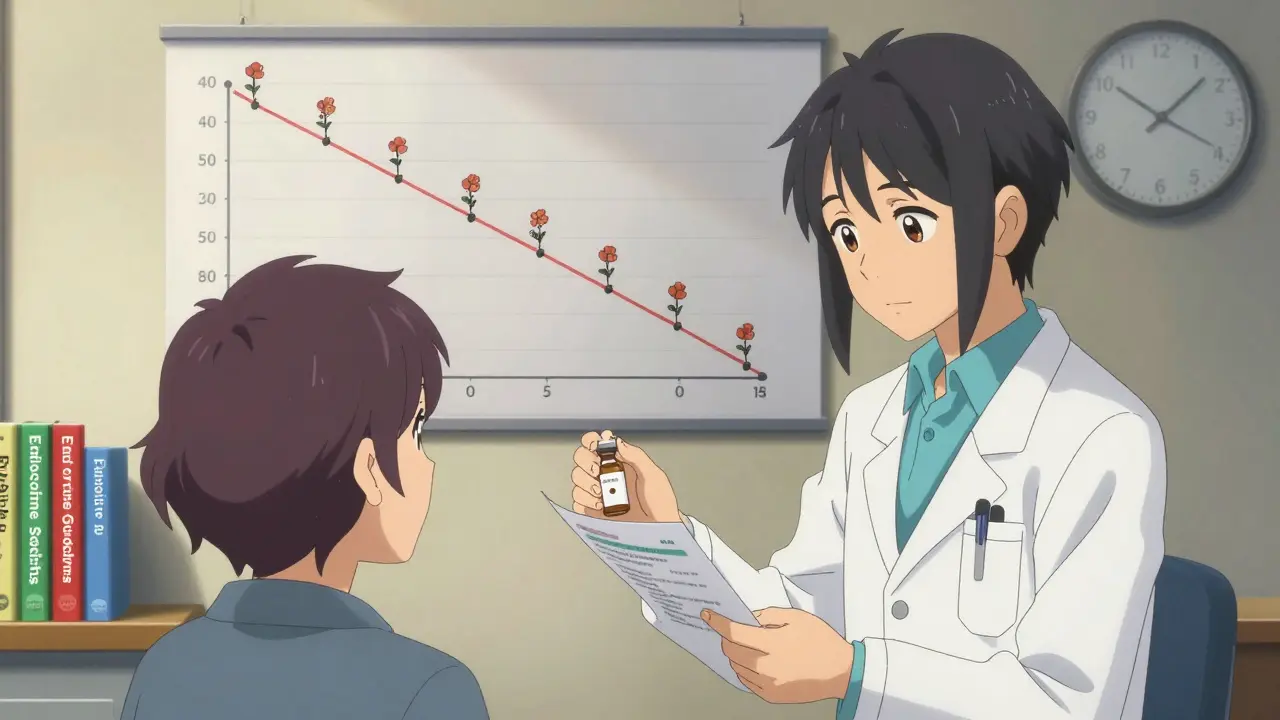
How Doctors Diagnose It
There’s no single test that works for everyone. But the standard first step is a morning blood test for cortisol and ACTH. If your cortisol is below 5 μg/dL within 24 hours of stopping steroids, you’re likely in adrenal insufficiency. Above 10 μg/dL, you’re probably safe. In between? That’s the gray zone - and you need more testing. The ACTH stimulation test is the gold standard. You get a shot of synthetic ACTH, and your cortisol levels are checked before and after. If your adrenal glands don’t respond, they’re not working. But here’s the catch: this test can be misleading if you’re still on steroids or just stopped them. Timing matters. Doctors need to know exactly when you last took your dose.How to Taper Safely - The Right Way
You can’t just stop. You have to come off slowly. But there’s no one-size-fits-all plan. The Endocrine Society says tapering should be personalized. Your doctor should consider how long you’ve been on steroids, your dose, your health, and whether you’ve had adrenal problems before. Here’s a practical guide based on the American College of Physicians’ 2024 toolkit:- If you were on more than 20 mg of prednisone daily: drop by 2.5-5 mg every 3-7 days.
- If you were on 5-20 mg daily: drop by 1-2.5 mg every 1-2 weeks.
- If you’ve been on steroids longer than six months: go even slower. Some patients need months to taper safely.
What You Need to Do Now - Even If You’re Done With Steroids
If you’ve stopped corticosteroids in the last six months, you’re still at risk. Here’s what you need to do:- Carry a medical alert card or bracelet that says you’ve had corticosteroid therapy.
- Have access to an emergency injection of hydrocortisone. Ask your doctor for a prescription - it’s not expensive, and it can save your life.
- Know when to use it. If you’re sick, injured, or under extreme stress, take an extra dose - even if you’re off steroids. Your body still needs cortisol.
- Teach someone close to you how to give the injection. In a crisis, you might not be able to do it yourself.

Why This Is Getting Worse - And What’s Being Done
Corticosteroid prescriptions have gone up 23% since 2015. More people are on them longer. That means more people are at risk for adrenal insufficiency. Yet many doctors still don’t talk about it. That’s starting to change. Since 2021, the FDA requires all systemic corticosteroid packages to include warnings about adrenal insufficiency. The European Medicines Agency now requires patient alert cards in 28 countries. The American Medical Association added adrenal crisis recognition to its mandatory continuing education list in 2024. New tools are coming. AI algorithms can now predict who’s at risk by scanning electronic health records - with 92% accuracy. Point-of-care cortisol tests are in trials and could give results in 15 minutes. That means ER doctors won’t have to guess anymore.What You Should Ask Your Doctor
If you’re prescribed corticosteroids, ask these questions:- "How long will I be on this?"
- "What’s the plan for coming off?"
- "Am I at risk for adrenal insufficiency?"
- "Can I get a prescription for emergency hydrocortisone?"
- "Will you give me written instructions to take home?"
Final Thought: It’s Not Just About Stopping - It’s About Surviving
Corticosteroids save lives. But they can also kill you if you don’t know how to stop them. Adrenal insufficiency from withdrawal isn’t rare. It’s common, preventable, and often missed. You don’t need to be an expert to protect yourself. You just need to know the signs, have the tools, and speak up. If you’ve ever taken steroids - even once - and you’re feeling off, don’t wait. Don’t assume it’s stress or the flu. Ask: Could this be my adrenal glands failing? And if the answer is yes, don’t delay. Get help.Can you get adrenal insufficiency from short-term steroid use?
Yes. Even short courses of corticosteroids - as little as four weeks - can suppress your body’s natural cortisol production. A 2023 study in Endocrine Abstracts found that doses as low as 5 mg of prednisone daily for over a month can cause adrenal suppression. This contradicts older beliefs that only long-term, high-dose use was dangerous. The key is duration, not just dose.
How do I know if I’m having an adrenal crisis?
An adrenal crisis is a medical emergency. Look for sudden, severe symptoms: very low blood pressure, confusion, fainting, vomiting, abdominal pain, and extreme weakness. You may also have a fever or feel like you’re going into shock. If you’ve taken steroids recently and have these symptoms, treat it as a crisis until proven otherwise. Give yourself an emergency hydrocortisone injection immediately and call for help.
Do I need an emergency injection if I’ve been off steroids for months?
It depends. Most people recover full adrenal function within 6-12 months after stopping steroids. But recovery isn’t guaranteed. If you were on steroids for over a year, had high doses, or had multiple courses, your adrenal glands may still be sluggish. If you’re facing major stress - surgery, trauma, infection - it’s safer to use an emergency injection than to risk an adrenal crisis. Talk to your doctor about your personal risk level.
Why don’t more doctors warn patients about this?
Many doctors assume adrenal insufficiency only happens with long-term use, or they think patients will remember the risks. But studies show 47% of patients don’t follow tapering plans - often because they weren’t clearly told what to do. A 2023 JAMA Internal Medicine study found that only 32% of patients received written instructions about adrenal risks. The system is failing patients. That’s why organizations like the Endocrine Society now require patient education as part of standard care.
Can I get adrenal insufficiency from inhaled or topical steroids?
It’s rare, but possible. Inhaled steroids (like those for asthma) and topical creams usually don’t cause adrenal suppression because very little enters the bloodstream. But if you use high-dose inhaled steroids for years, or apply potent topical steroids over large areas of skin for weeks, you can absorb enough to suppress your adrenal glands. People with eczema or severe asthma on long-term, high-dose regimens should be monitored.
Is adrenal insufficiency permanent?
Usually not. Most people’s adrenal glands recover within 6 to 12 months after stopping steroids, especially if they tapered slowly. But recovery can take longer - up to 18 months or more - in people who were on high doses for over a year. Blood tests (like ACTH stimulation) can track recovery. Some patients never fully regain normal function, but that’s uncommon. The key is patience and avoiding stress during recovery.
What’s the difference between primary, secondary, and tertiary adrenal insufficiency?
Primary adrenal insufficiency (Addison’s disease) means your adrenal glands are damaged and can’t make cortisol at all. Secondary is when your pituitary gland doesn’t signal the adrenals to make cortisol. Tertiary is caused by your hypothalamus not producing CRH, which usually happens after long-term steroid use. Tertiary is the most common type after corticosteroid withdrawal. The treatment is the same - replace cortisol - but the cause and testing differ.
Can stress trigger adrenal insufficiency even after stopping steroids?
Yes. If your adrenal glands haven’t fully recovered, any major stress - infection, surgery, physical trauma, or even emotional shock - can push you into crisis. Your body needs cortisol to handle stress. If you’re still recovering, you don’t have enough reserve. That’s why patients are advised to take extra steroid doses during illness or injury, even months after stopping treatment.






8 Comments
I was on prednisone for six weeks after a bad asthma flare. Felt fine after stopping - until I tried to mow the lawn and passed out. Turns out my adrenals were totally shut down. No one warned me. Now I carry hydrocortisone everywhere. Don’t wait until you’re collapsing to learn this stuff.
Simple rule: if you’ve taken steroids for more than a month, assume your body forgot how to make cortisol. Play it safe.
Oh wow, so the medical system’s latest genius move is to give people life-saving drugs… and then pretend they’re magic beans you just spit out when you’re done? Brilliant. I’m sure the 15-minute ER visit where they diagnose you with ‘chronic fatigue’ after you nearly died is totally worth the $2000 copay.
At least the FDA finally added a warning. Took long enough. Next they’ll put a ‘don’t breathe’ sticker on oxygen tanks.
Adrenal suppression is a well-documented iatrogenic phenomenon resulting from HPA axis downregulation secondary to exogenous glucocorticoid exposure. The pituitary reduces ACTH secretion, leading to adrenal atrophy - a reversible but time-dependent process.
Current guidelines from the Endocrine Society and ACP emphasize individualized tapering protocols based on duration, dose, and patient comorbidities. Failure to adhere to these protocols elevates the risk of adrenal crisis, which carries a 6% mortality rate in hospitalized cases.
Emergency hydrocortisone is not optional. It’s a biological necessity for patients with prior systemic steroid exposure. Every primary care provider should be prescribing this as standard of care - not as an afterthought.
As someone who grew up in a country where doctors hand out steroids like candy for sniffles, I can tell you - this isn’t just an American problem. In South Africa, we see it too. People stop their meds after a week because they ‘feel better,’ then end up in the ER with no idea why they’re shaking and vomiting.
It’s not just about the science. It’s about culture. We need to change how we talk about medication. It’s not ‘take it till you feel better.’ It’s ‘take it till your body remembers how to work again.’
And if your doctor doesn’t explain that? Find a new one. Your life depends on it.
you know what’s really going on? the pharma companies dont want you to know your body can heal itself. they make billions off steroids and then act like its normal to be hooked for life. and the docs? theyre just paid to keep the machine running. i got off prednisone and my body came back - but i had to go off-grid, eat raw food, and meditate for 3 hours a day. no one tells you that. they just give you a shot and say ‘good luck’.
they even hide the fact that cortisol is naturally made by your adrenal glands. its like they want you to forget you’re a human and not a robot that needs a battery refill.
Thomas, I’ve been there. I tapered too fast after a 10-week course for my autoimmune condition. Felt fine for two weeks - then got hit with a flu and collapsed. Took me months to recover fully.
The scary part? Most people don’t even realize they’re at risk. Your body doesn’t scream when it’s failing - it just quietly shuts down. That’s why education is everything.
If you’re off steroids, treat yourself like a recovering addict. No stress. No rushing. No pretending you’re fine. Give your adrenals time. They’re not lazy - they’re just rebuilding.
Regarding the ACTH stimulation test - timing is critical. Testing within 24–48 hours of the last steroid dose can yield false negatives due to residual exogenous cortisol. Best practice is to wait 24–72 hours post-last dose, ideally in the morning (8–9 AM), with baseline cortisol and ACTH drawn first.
If cortisol is <5 μg/dL and ACTH >100 pg/mL, that’s secondary adrenal insufficiency. If cortisol doesn’t rise >18 μg/dL after stimulation, adrenal reserve is severely compromised.
Don’t rely on symptoms alone. Lab confirmation is non-negotiable.
Hey everyone - I know this stuff is scary. But you’re not alone. I’ve talked to dozens of people who’ve been through this. The good news? Recovery is possible. Most people’s adrenals come back - if they’re given time and care.
Don’t panic. Don’t feel guilty. Just get the facts. Ask for the emergency kit. Tell your family how to use it. Write down your taper plan. And if your doctor says ‘it’s fine,’ ask them to show you the evidence.
You’re not being paranoid. You’re being smart. And that’s worth celebrating.
Write a comment