Diabetes Medication Selector
Find the most appropriate diabetes medication alternatives based on your specific health needs and priorities.
Your Health Priorities
If you’ve been prescribed Metformin for type 2 diabetes, you’re not alone. It’s been the first-line treatment for over 20 years, used by more than 150 million people worldwide. But what if it’s not working for you? What if you’re dealing with stomach upset, or your blood sugar still won’t budge? Maybe you’ve heard about newer drugs like Ozempic or Jardiance and wonder if they’re better. This isn’t about ditching Metformin-it’s about understanding your options when it’s not enough.
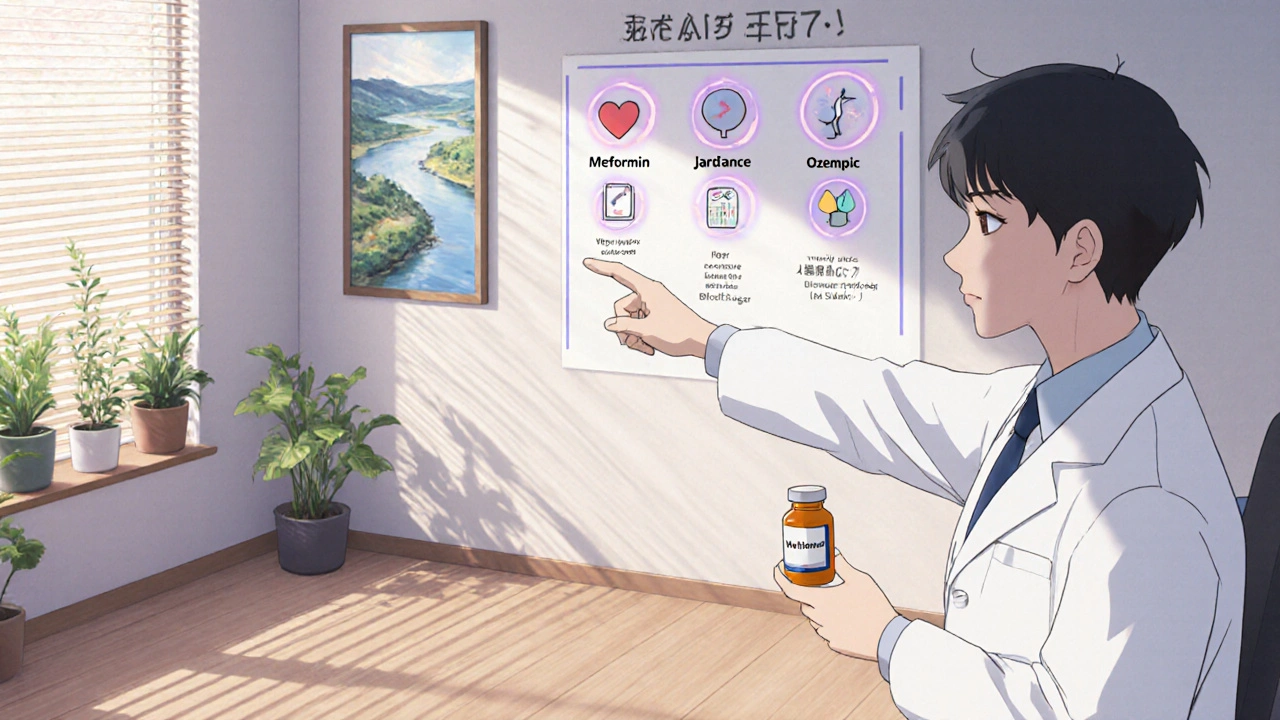
Why Metformin Is Still the Starting Point
Metformin works by lowering how much sugar your liver releases and helping your body use insulin better. It doesn’t cause weight gain. It rarely causes low blood sugar on its own. And it’s cheap-often under $10 a month in the U.S. A 2023 study in The Lancet Diabetes & Endocrinology found that patients on Metformin had a 30% lower risk of heart problems over five years compared to those on other first-line drugs.
But it’s not perfect. About 25% of people can’t tolerate it because of nausea, diarrhea, or bloating. Some people just don’t respond well-even at high doses. Others need more than just blood sugar control-they need weight loss, heart protection, or kidney benefits.
Biguanide Alternatives: Still in the Same Family
There aren’t many other biguanides like Metformin. Phenformin was pulled from the market in the 1970s because of lactic acidosis risk. So if you’re looking for something chemically similar, you’re mostly stuck with Metformin. But there are other classes of drugs that do similar things-and sometimes better.
SGLT2 Inhibitors: Lower Blood Sugar and Protect Your Heart and Kidneys
Drugs like Empagliflozin (Jardiance), Dapagliflozin (Farxiga), and Canagliflozin (Invokana) work differently. They tell your kidneys to dump excess sugar out through urine. That means you lose 100-200 calories a day as sugar-leading to modest weight loss (5-10 lbs on average).
These drugs don’t just lower blood sugar. They reduce heart failure hospitalizations by up to 30% and slow kidney disease progression in people with diabetes. A 2024 analysis of 12 trials showed SGLT2 inhibitors lowered the risk of kidney failure by 40% compared to Metformin alone.
Downsides? You might get more yeast infections or urinary tract infections. You need to drink more water. And there’s a small risk of diabetic ketoacidosis, especially if you’re sick or cutting carbs too hard.
GLP-1 Receptor Agonists: Weight Loss and Stronger Blood Sugar Control
These are the drugs you’ve seen advertised-Semaglutide (Ozempic, Wegovy), Liraglutide (Victoza), Dulaglutide (Trulicity). They mimic a gut hormone that tells your pancreas to release insulin only when blood sugar is high. They also slow digestion and reduce appetite.
People on GLP-1 agonists lose an average of 10-15% of their body weight. That’s more than most other diabetes drugs combined. In trials, Semaglutide reduced HbA1c by 1.5-2.0%-better than Metformin’s typical 0.5-1.5%. They also cut heart attack and stroke risk by 20-25% in high-risk patients.
But they’re injectable. They cost $800-$1,200 a month without insurance. And side effects include nausea, vomiting, and constipation-especially at first. Some people can’t tolerate them at all.
DPP-4 Inhibitors: Mild, But Safe
Drugs like Sitagliptin (Januvia), Linagliptin (Tradjenta), and Saxagliptin (Onglyza) boost your body’s own GLP-1 by blocking the enzyme that breaks it down. They’re pills, weight-neutral, and low risk for low blood sugar.
But they’re not powerful. On average, they lower HbA1c by only 0.5-0.8%. That’s less than Metformin. They don’t help with weight loss or heart protection. They’re usually used as add-ons when Metformin isn’t enough but GLP-1s or SGLT2s aren’t an option.
Thiazolidinediones: Effective but Risky
Pioglitazone (Actos) makes your body more sensitive to insulin. It lowers HbA1c by about 1.0-1.5% and can improve cholesterol. But it causes weight gain, fluid retention (worsening heart failure), and increases fracture risk in women.
It’s rarely used today unless someone has severe insulin resistance and can’t take other drugs. It’s also been linked to a small increase in bladder cancer risk, so it’s avoided in people with a history of that.
Sulfonylureas: Old School, But Still Used
Drugs like Glimepiride (Amaryl) and Glipizide (Glucotrol) force your pancreas to make more insulin. They’re cheap and work fast.
But they cause weight gain and low blood sugar-sometimes dangerously so. A 2022 study in JAMA Internal Medicine found people on sulfonylureas were 4 times more likely to have severe hypoglycemia than those on Metformin. They don’t protect the heart. They’re mostly used when cost is the biggest barrier and other drugs aren’t available.
Insulin: When Everything Else Fails
Insulin isn’t an “alternative” to Metformin-it’s often the next step when Metformin and other pills don’t control blood sugar anymore. About 30% of people with type 2 diabetes will need insulin within 10 years.
Modern insulins like Insulin Glargine (Lantus) or Insulin Degludec (Tresiba) are long-acting and cause fewer lows than older versions. But you still have to inject them. You’ll need to check your blood sugar more often. And weight gain is common.
Insulin is powerful. It’s not a failure-it’s a tool. Many people feel guilty needing it. But if your pancreas is worn out, insulin is the only thing that can get your sugar under control.
When to Consider Switching from Metformin
You don’t need to switch just because you’re on Metformin. But consider alternatives if:
- Your HbA1c stays above 7.5% after 3 months on the max dose (2,000 mg/day)
- You can’t tolerate the side effects and antacids or slow-release versions don’t help
- You need to lose weight and Metformin isn’t helping
- You have heart failure, kidney disease, or a high risk of heart attack
- Your doctor says your pancreas isn’t making enough insulin anymore
Switching doesn’t mean Metformin failed. It means your body changed-and your treatment should too.

Cost and Access: What You Can Actually Get
Metformin costs $5-$15/month. SGLT2s and GLP-1s? $300-$1,200/month without insurance. Many people can’t afford them.
But there’s help. Most manufacturers offer patient assistance programs. Some pharmacies sell Semaglutide for $250/month with coupons. Medicare Part D often covers SGLT2s and GLP-1s if you have heart or kidney disease.
Don’t assume you can’t get the newer drugs. Talk to your pharmacist. Ask about manufacturer coupons. Ask if your insurance requires step therapy-sometimes you have to try Metformin first, but you can appeal.
Combining Drugs: The Real Strategy
Most people don’t take just one drug. The American Diabetes Association recommends starting with Metformin, then adding a second drug based on your needs:
- Need weight loss? Add a GLP-1 agonist.
- Heart or kidney disease? Add an SGLT2 inhibitor.
- Just need a little more help? Add a DPP-4 inhibitor.
Some people take Metformin + SGLT2 + GLP-1 together. That’s not rare. It’s becoming standard for high-risk patients.
What’s Not an Alternative
Don’t fall for the hype. Berberine? Cinnamon? Apple cider vinegar? Some studies show tiny, short-term drops in blood sugar-but nothing close to Metformin’s effect. They’re not regulated. They can interact with other meds. And they don’t protect your heart or kidneys.
These aren’t alternatives. They’re distractions. If you’re serious about managing diabetes, stick with evidence-based medicine.
Final Thought: It’s Not About the Best Drug. It’s About the Right Drug for You.
Metformin is a great first choice. But it’s not the only choice. The right drug for you depends on your body, your goals, your risks, and your budget.
There’s no shame in needing something stronger. There’s no shame in needing something gentler. What matters is that you and your doctor are working together-not just following a script.
Your diabetes management isn’t a one-size-fits-all puzzle. It’s a custom fit. And the pieces you need might not be the ones you started with.
Can I stop Metformin and just use a GLP-1 agonist like Ozempic?
Yes, but only under medical supervision. Some people switch entirely to GLP-1 agonists like Semaglutide, especially if they need weight loss or can’t tolerate Metformin. But GLP-1s don’t work the same way-they don’t reduce liver glucose production like Metformin does. Your doctor may still recommend keeping Metformin if your blood sugar is high, because the two work well together.
Is Metformin safer than newer diabetes drugs?
Metformin has a long safety record, but newer drugs like SGLT2 inhibitors and GLP-1 agonists have proven safety profiles too. In fact, they reduce risks of heart attack, stroke, and kidney failure better than Metformin in high-risk patients. The biggest risk with Metformin is lactic acidosis, which is rare but serious in people with kidney disease. Newer drugs avoid that risk entirely.
Do any alternatives help with weight loss like Metformin does?
Metformin helps some people lose 5-10 pounds, but not everyone. GLP-1 agonists like Ozempic and Wegovy cause much more weight loss-often 10-20% of body weight. SGLT2 inhibitors like Farxiga lead to 5-10 pounds of loss. So if weight loss is your goal, Metformin isn’t the strongest option. The newer drugs are.
Why do doctors still start with Metformin if newer drugs are better?
Because Metformin is cheap, effective, and has decades of data showing it reduces complications. Newer drugs are better for specific goals-like heart protection or weight loss-but they’re expensive. Doctors start with Metformin because it’s the best value for most people. If you need more, they add on. It’s not about what’s newest-it’s about what’s right for your situation.
Can I switch from Metformin to a natural supplement instead?
No. Supplements like berberine, cinnamon, or chromium may show small, temporary effects in studies-but they’re not regulated, don’t protect your organs, and can interfere with other medications. There’s no evidence they prevent heart attacks, kidney failure, or nerve damage like FDA-approved drugs do. Relying on supplements instead of proven medication puts your health at serious risk.


8 Comments
metformin gave me diarrhea so bad i thought i was gonna die. switched to ozempic and now i just feel normal. also lost 22 lbs. no more 3am bathroom runs. best decision ever.
Interesting breakdown. I’ve been on metformin for 8 years and it’s been fine, but my A1c’s creeping up. Might talk to my doc about adding an SGLT2i-heard they help with blood pressure too.
It’s important to emphasize that while newer agents offer superior cardiovascular and renal outcomes, metformin remains foundational due to its safety profile, affordability, and long-term data. The decision to switch or add should be individualized, not driven by marketing or social media trends.
Stop pretending metformin is ‘safe.’ It’s a dirty drug that ruins your gut and does jack for weight loss. Meanwhile, GLP-1s are the future-and anyone still pushing metformin as the gold standard is either paid by Big Pharma or too lazy to read the 2024 ADA guidelines. Also, ‘natural supplements’? Please. You’re not healing your diabetes with apple cider vinegar. You’re just delaying the inevitable amputation.
Regarding the use of SGLT2 inhibitors: the mechanism of action-renal glucosuria-induces a caloric deficit, which, in turn, contributes to modest weight reduction; however, the concomitant risk of euglycemic diabetic ketoacidosis (euDKA), particularly in the context of low-carbohydrate dietary adherence or acute illness, necessitates patient education and vigilant monitoring. Furthermore, the incidence of genitourinary mycotic infections is statistically significant (p<0.01) in clinical trial cohorts.
Oh my goodness, I’ve been on metformin for five years and my doctor just told me to switch to Jardiance because of my kidney numbers. I didn’t know it could help kidneys, I thought it was just for sugar. Now I’m reading all these studies and I feel like I’ve been living in the 1990s. Also, I’m terrified of injections-I’ve never given myself a shot. Do they really hurt? I’ve heard people say it’s like a mosquito bite but I don’t believe them. And what if I forget? I’m already bad at taking pills on time. I’m so overwhelmed. Why does everything have to be so complicated?
Hey Rika, you’re not alone. I was scared of the Ozempic pen too. First shot felt weird, but honestly? It’s way easier than you think. The needle’s tiny. And you only do it once a week. My doc gave me a demo video-I watched it three times and then did it while watching Netflix. You got this. And your kidneys will thank you.
I switched from metformin to semaglutide last year after my heart attack. I lost 30 pounds. My BP dropped. My A1c went from 8.4 to 5.9. People say ‘it’s just for weight loss’-but it saved my life. I don’t care if it’s expensive. My insurance covered it after I appealed. If you’re scared of the cost, ask your pharmacist about the savings card. Don’t let money stop you from living.
Write a comment