Every year, thousands of patients in the U.S. receive the wrong medication-not because the pharmacy made a mistake in filling the prescription, but because the wrong person was given it. This isn’t rare. It’s systemic. And it starts with a simple failure: using only one identifier to confirm who the patient is.
Why Two Identifiers Are Non-Negotiable
The Joint Commission, the main body that accredits U.S. hospitals and pharmacies, made this rule official in 2003: you must use two patient identifiers before giving any medication. Not one. Not when you’re busy. Not if the patient says they’re John Smith. You need two distinct pieces of information that belong to that person alone. Acceptable identifiers? Name, date of birth, medical record number, or phone number. What’s not allowed? Room number. Bed number. Location. These change. They’re not tied to the person. Using them is like trying to identify your car by its parking spot-maybe it works today, but tomorrow, it’s someone else’s car in that spot. Why does this matter so much? Because names aren’t unique. There are over 1.2 million people named John Smith in the U.S. alone. Add in common last names like Garcia, Johnson, or Lee, and you’ve got a minefield. A 2023 survey by the American Society of Health-System Pharmacists found that 42% of community pharmacists regularly verify patients using only verbal confirmation-no documentation, no cross-check. That’s not safety. That’s luck.What Happens When You Skip the Second Identifier
In 2020, a study in JMIR Medical Informatics found that up to 10% of serious drug-drug interaction alerts go undetected-not because the system is broken, but because the patient’s record is mixed up. One woman, prescribed a blood thinner, ended up with a duplicate record under her middle name. Her allergy to aspirin was buried in the old record. The new record said nothing. She got aspirin. She had a stroke. This isn’t an outlier. The Emergency Care Research Institute lists patient misidentification as one of the top 10 threats to patient safety. It causes wrong-drug errors, wrong-dose errors, transfusion errors, and even infants being sent home with the wrong family. In pharmacy settings, where prescriptions are filled quickly and staff are under pressure, these errors are especially dangerous. A 2024 Altera Health survey showed that hospitals without a centralized patient index (EMPI) had only a 17% match rate between patient records. That means one in five patients had their records split across multiple files. Imagine trying to know if someone’s allergic to penicillin when their allergy is logged under a different spelling of their name.Manual Verification Isn’t Enough
You might think, “We just ask for name and DOB. That’s two identifiers. We’re good.” But manual checks are flawed. People mishear names. Patients forget their birth year. Staff get distracted. A 2020 review in BMJ Quality & Safety found no strong evidence that double-checking by two staff members reduces errors-unless there’s technology backing it up. Why? Because humans aren’t reliable. We’re tired. We’re rushed. We assume. We think, “Oh, it’s Mrs. Carter again-she always takes lisinopril.” And then you hand her someone else’s medication. The data doesn’t lie. A 2012 study in the Journal of Patient Safety showed that when pharmacies added barcode scanning to verify patient ID and medication, medication errors reaching patients dropped by 75%. That’s not a small win. That’s life-saving.
Technology That Works: Barcodes and Biometrics
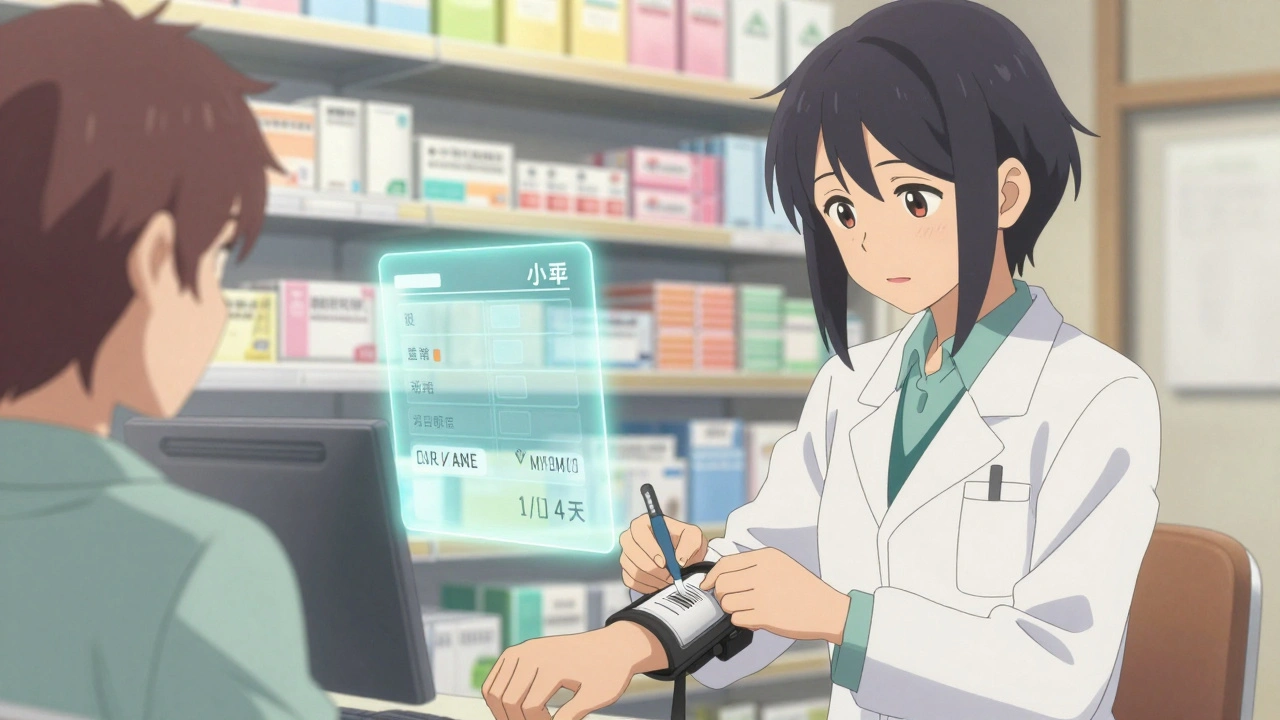
The most effective systems today combine two identifiers with technology. Here’s how:- Barcode scanning: Patient wears a wristband with a barcode. Pharmacist scans it before dispensing. The system matches the patient’s ID to the prescription. If it doesn’t match, it flags the error.
- Biometric ID: Systems like Imprivata PatientSecure use palm-vein scanning. No card, no memory, no name to spell. Just scan your hand. In 2024, this system achieved a 94% match rate. Without it? Only 17%.
- EMPI systems: Enterprise Master Patient Indexes tie all a patient’s records together-no matter how many times they’ve been seen, or what name was used. Hospitals with EMPI reduce duplicate records by over 80%.
Real-World Failures and Fixes
A patient was brought to a hospital unconscious. Staff couldn’t find his record. They created a new one. Days later, they found his old record-under his middle name. It listed a life-threatening allergy to vancomycin. He’d been given it twice already. He survived by luck. That’s not a glitch. It’s a design flaw. And it’s fixable. The Institute for Safe Medication Practices recommends:- Using a “timeout” before high-risk meds-like chemo or insulin-where everyone stops, confirms both identifiers, and says them out loud.
- Documenting every verification. The Joint Commission found that 37% of non-compliant pharmacies didn’t even record the check.
- Training staff to treat identification like a sterile procedure-no shortcuts, no assumptions.
What’s Changing in 2025 and Beyond
The Office of the National Coordinator for Health IT launched a pilot in January 2025 to test a national patient identifier system. It’s voluntary. It’s opt-in. But it’s the first real step toward a future where your medical record follows you-not your name, not your birthdate, but a unique code tied only to you. Why now? Because duplicate records cost hospitals $40 million a year in reconciliation and error correction. Because 8-12% of patient records are split across systems. Because without accurate identification, interoperability is impossible. The World Health Organization, the ECRI Institute, and Harvard Medical School all agree: this isn’t about paperwork. It’s about survival.What You Can Do-As a Pharmacist, Patient, or Caregiver
If you work in a pharmacy:- Never skip the second identifier. Even if the patient says, “You know me.”
- Insist on barcode scanning. If your pharmacy doesn’t have it, push for it.
- Document every check. If it’s not written down, it didn’t happen.
- Always bring your ID card with your full name and date of birth.
- Ask: “Are you checking my name and birthdate before giving me this pill?”
- If you’ve been to multiple clinics, ask if your records are linked. Say: “I’ve had care at X Hospital and Y Clinic-can you make sure my allergies are in one place?”





12 Comments
Just read this and cried a little. My grandma almost got the wrong heart med because they only asked for her name. She’s 87, doesn’t remember her DOB, and they just went with ‘yeah, that’s her’. We’re lucky she’s still here.
Thank you for writing this. 💔
Two IDs. That’s it. No magic. No AI. Just stop being lazy.
It’s not hard. It’s not expensive. It’s just human.
Do the thing.
I’ve worked ER triage for 14 years and I’ve seen too many cases where someone gets a double record because they used ‘Linda’ instead of ‘Linda Marie’ or their middle name was dropped on one form.
It’s not about being perfect. It’s about being consistent. Every time. No exceptions. No ‘but she’s been here before’. That’s how people die.
We need to stop treating patient ID like a suggestion. It’s a lifeline.
Look, I get it. You want to save time. You’re tired. You’ve got 12 patients waiting. But here’s the cold truth: skipping the second identifier isn’t efficiency-it’s negligence dressed up as hustle.
The Joint Commission didn’t make this rule because they hate pharmacists. They made it because people are dying. 42% of pharmacies are just winging it? That’s not a system. That’s Russian roulette with pills.
And don’t give me that ‘we’re understaffed’ excuse. Understaffed doesn’t mean under-ethical. You don’t get to cut corners because your boss won’t hire more people. That’s not leadership. That’s surrender.
Barcodes aren’t optional. Biometrics aren’t futuristic. They’re basic. If your pharmacy still uses ‘room number’ or ‘last name + birth year’ as a system, you’re not a pharmacy-you’re a liability.
And the fact that 37% of non-compliant pharmacies don’t even document their checks? That’s not incompetence. That’s arrogance. You think no one will find out? Someone always does. And when they do, it’s not a lawsuit-it’s a funeral.
Stop pretending this is about paperwork. It’s about whether someone wakes up tomorrow-or if their family has to explain why their mom got aspirin instead of blood thinners.
I’ve seen the charts. I’ve read the autopsies. There’s no ‘accident’ here. Only avoidable failures. And we’re the ones who keep letting them happen.
Do better. Or get out.
As a nurse, I’ve seen this play out too many times. I’ve watched people get the wrong meds because someone assumed ‘it’s the same guy who came in last week’. No. It’s not. And if you don’t verify, you’re not a healthcare worker-you’re a gamble.
My hospital went full barcode + EMPI last year. Errors dropped 70%. Not because we’re smarter. Because we stopped trusting memory.
Stop being proud of your ‘experience’. Use the tools. They exist for a reason.
The systemic failure here isn’t just about identifiers-it’s about how we’ve normalized risk in healthcare. We’ve turned safety protocols into checkboxes instead of sacred rituals.
It’s not enough to say ‘we do two identifiers’. We need to cultivate a culture where skipping one is socially unacceptable, not just policy-violating.
Imagine if pilots skipped pre-flight checklists because they were ‘in a hurry’. We wouldn’t tolerate it. Why do we tolerate it here?
Y’all are overcomplicating this. Two IDs. Scan the wristband. Say it out loud. Write it down.
That’s it. No app. No AI. Just do the damn thing.
And if your boss says ‘we don’t have time’-tell them the cost of one error is 10x the cost of hiring one extra tech.
You got this. Keep pushing.
Okay but like… why do we even have names if we can’t just trust ‘em? I mean, if you’re John Smith, you’re John Smith. Why make it harder? My cousin got the wrong meds once and he just laughed it off. He’s fine.
Maybe we’re just being too dramatic?
Also, biometrics? That’s creepy. I don’t want my palm scanned like I’m in a sci-fi movie.
Why are we letting the government dictate how we run pharmacies? This is America. We don’t need some federal agency telling us to scan wristbands. We’re not in Sweden.
Let people take responsibility. If you’re John Smith, you should know your own DOB. If you can’t remember it, that’s your problem.
Stop infantilizing patients. And stop turning every mistake into a national crisis.
Also, ‘EMPI’? Sounds like a communist database. I’m not giving the state my medical ID.
Y’all are so woke about this. Like, I get it. You want to save lives. But this is America. We don’t have time for all this paperwork. I’ve seen patients lie about their name to get free meds. Should we let them win?
Also, why are we spending millions on palm scans when we could just pay nurses more? This is performative safety. It looks good on a PowerPoint. Doesn’t fix the real problem: we don’t pay people enough to care.
And don’t even get me started on ‘EMPI’. That’s just the government tracking us under the guise of ‘safety’.
My pharmacy doesn’t scan. We say ‘name and DOB’. 99% of the time it’s fine. The 1%? That’s just life.
Wait-so you’re saying we should trust a barcode more than a human? That’s insane. What if the barcode is smudged? What if the scanner breaks? What if the system crashes?
Humans have intuition. Machines don’t. I’ve worked in pharmacies for 20 years. I know when someone’s lying. You can’t scan that.
And what about elderly patients who don’t have wristbands? Are we just gonna say ‘sorry, you’re not verified’ and send them home?
This whole thing feels like tech bros trying to fix a human problem with gadgets.
Bro. You’re arguing against the thing that saves lives.
Barcodes don’t lie. Humans do.
And if your scanner breaks? You stop. You don’t wing it. That’s not ‘intuition’-that’s gambling with someone’s life.
And yes-elderly patients get wristbands too. You don’t get to skip because it’s ‘hard’.
Do better.
Write a comment