Opioid Dose Calculator
Opioid Dose Calculator
Calculate morphine milligram equivalents (MME) to understand your postoperative ileus (POI) risk. The ERAS guidelines recommend keeping opioid use under 30 MME in the first 24 hours to reduce POI risk.
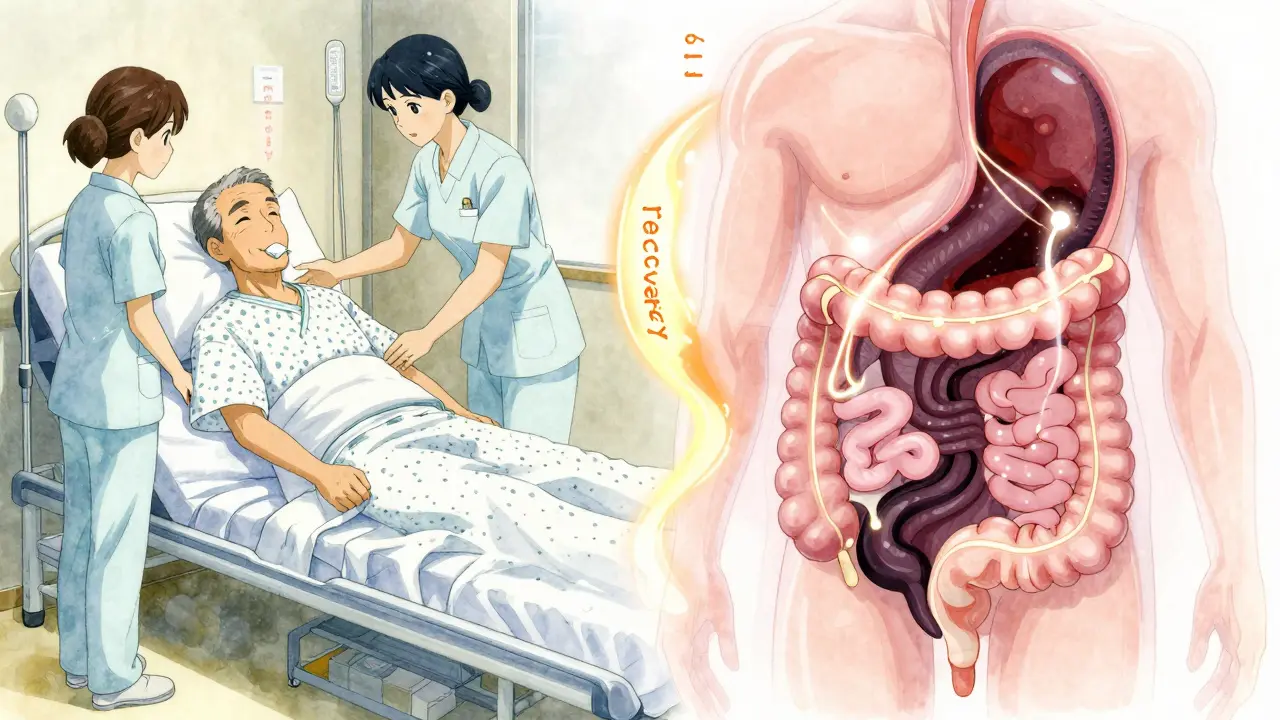
After surgery, many patients expect to feel sore-but not stuck. If you can’t pass gas, eat, or have a bowel movement for days after your procedure, you’re not alone. This is postoperative ileus (POI), a common and frustrating complication that’s often worsened by the very drugs meant to control your pain: opioids.
POI isn’t just discomfort. It’s a real delay in your recovery. Your gut essentially shuts down. Nausea, bloating, vomiting, and no bowel movements for more than three days are red flags. And while surgery itself plays a role, opioids are the biggest driver. They don’t just numb your pain-they slow your intestines to a crawl. Studies show that patients getting high doses of opioids after surgery take nearly three times longer to have their first bowel movement compared to those on lower doses.
Why Opioids Cause Your Gut to Shut Down
Opioids bind to mu-receptors in your gut wall, not just your brain. These receptors control how your intestines contract and move food along. When activated, they reduce muscle movement by up to 70% in experimental models. That’s why you get hard stools, bloating, and that awful feeling of fullness even when you haven’t eaten.
It’s not just the pills you take. Your body releases its own opioids during surgery stress, making things worse. Add to that the inflammation from the cut tissue, and the nervous system signals that shut down digestion, and you’ve got a perfect storm. Most patients start noticing symptoms within 24 to 72 hours after surgery. By day three, if nothing’s moving, it’s officially POI.
Here’s what it looks like in real life: A 62-year-old man had a colon resection. He was on 8 mg of morphine per hour through his IV pump. By day two, he was bloated, nauseous, and hadn’t passed gas. His chart showed 192 morphine milligram equivalents (MME) in 48 hours-way above the recommended limit. He stayed in the hospital five extra days. His pain was controlled, but his gut wasn’t.
The Cost of a Slowed Gut
POI doesn’t just hurt-it costs. The U.S. healthcare system spends about $1.6 billion a year on extended hospital stays because of it. On average, POI adds 2 to 3 days to a hospital stay. For a patient recovering from hip surgery, that means more bed rest, more risk of blood clots, more nursing time, and more bills.
Hospitals are starting to feel the pinch. Medicare penalizes facilities with too many readmissions due to complications like POI. In 2022, 15.7% of general surgery programs faced these penalties-averaging $187,000 per hospital. That’s why big medical centers are changing how they manage pain.
What Doesn’t Work
Old-school fixes like nasogastric tubes (those nose-to-stomach tubes) don’t help much. A Cochrane review found they only cut POI duration by 12%. Passing a tube in doesn’t restart your gut-it just drains fluid and makes you uncomfortable.
Waiting for your body to “get back to normal” also doesn’t work. Gut motility doesn’t magically restart after surgery. You need active intervention.
What Actually Works: Prevention First
The best way to handle POI is to stop it before it starts. That means cutting back on opioids-and replacing them with smarter tools.
The Enhanced Recovery After Surgery (ERAS) guidelines recommend keeping opioid use under 30 MME in the first 24 hours. That’s about three 10mg oxycodone pills or one 10mg hydromorphone dose. Sticking to that cuts POI risk from 30% down to 18%.
Here’s what a successful plan looks like:
- Start before surgery: Give acetaminophen (1g IV) and ketorolac (30mg IV) before the cut. These reduce inflammation and pain without touching your gut.
- Use regional anesthesia: Spinal or epidural blocks cut opioid needs by half. One study showed orthopedic patients on spinal anesthesia had POI rates of just 8.5% vs. 22.3% with general anesthesia and opioids.
- Move early: Get up and walk within 4 hours after surgery. Patients who did this recovered bowel function 22 hours faster than those who stayed in bed.
- Chew gum: Yes, really. Chewing gum tricks your brain into thinking you’re eating. It triggers digestive signals. Nurses on AllNurses reported that patients chewing gum four times a day cut POI duration from 4.1 days to 2.7 days.
- Monitor closely: Track time to first flatus, first bowel movement, and ability to drink 1,000 mL of fluid without vomiting. If you haven’t passed gas by 72 hours or had a bowel movement by 96 hours, it’s time to act.
Treatment Options When POI Happens
If prevention fails, you need targeted treatment. Opioid antagonists are the only drugs proven to reverse the effect.
Alvimopan (Entereg) was approved in 2008 but pulled off the market due to heart risks. A new extended-release version is in late-stage trials and could return by 2026.
Methylnaltrexone (Relistor) is available now. Given as a shot under the skin, it blocks opioid receptors in the gut without affecting pain relief in the brain. Studies show it speeds up bowel movement by 30-40% in opioid-tolerant patients. One dose costs about $147.50. It’s not cheap-but it’s cheaper than an extra three days in the hospital.
It’s not for everyone. Don’t use it if you have a bowel obstruction (which happens in less than 0.5% of cases). And it won’t help if you’re already on very low opioid doses.
The Opioid Tightrope
Here’s the catch: you can’t just stop opioids cold. Pain control matters too. If you drop opioids below 20 MME per day, pain scores jump by 2-3 points on a 10-point scale. That’s not just uncomfortable-it can slow healing.
The goal isn’t zero opioids. It’s minimum effective dose. Use the lowest amount possible for the shortest time. Combine it with non-opioid drugs. Use regional blocks. Avoid long-acting opioids unless absolutely necessary.
One mistake doctors still make: switching from IV to oral opioids too fast. Patients can go into withdrawal-nausea, sweating, anxiety-because their gut is still sluggish and can’t absorb the pills. That’s not POI, that’s opioid withdrawal. It lasts 72-96 hours and can send patients back to the hospital.
Who’s at Highest Risk?
Not everyone gets POI. Some patients are more vulnerable:
- Those having abdominal surgery (colon, stomach, gallbladder)
- Patients who’ve never taken opioids before (opioid-naive)
- People over 65
- Those with diabetes or previous bowel issues
- Patients getting more than 40 MME in the first 24 hours
High-risk patients should get a POI prevention bundle from day one. That means: pre-op acetaminophen, spinal anesthesia if possible, gum chewing, walking within 4 hours, and a plan for methylnaltrexone if opioids are needed.
Why Some Hospitals Still Don’t Get It
Changing habits is hard. In 63% of hospitals that tried to adopt ERAS protocols, anesthesia teams resisted. They were used to reaching for opioids first. Nurses didn’t know how to encourage early walking. Doctors didn’t track opioid doses accurately.
Success comes with structure. The best programs hold daily “POI rounds”-a quick check with surgeons, anesthesiologists, and nurses to review each patient’s progress. They track opioid totals, bowel function, and mobility. Compliance hits 85-90% within a year. Hospital stays drop by 1.8 days. Each patient saves about $2,300.
But disparities remain. Academic centers have 92% adoption of these protocols. Rural hospitals? Only 28%. That means patients in small towns wait 5.1 days for their gut to restart-nearly two days longer than those in big hospitals.
The Future Is Here
AI is now being used to predict who’ll get POI. Mayo Clinic’s model uses 27 pre-op factors-age, BMI, medications, surgery type-to flag high-risk patients with 86% accuracy. That means you can start prevention before you even go under anesthesia.
Other ideas in testing: fecal microbiome transplants to reboot gut bacteria, and naltrexone implants that slowly block opioid receptors in the gut for days. These aren’t standard yet-but they’re coming.
By 2027, experts believe POI prevention will be standard care. The Agency for Healthcare Research and Quality estimates we could save $7.2 billion a year if 90% of hospitals adopt these practices.
It’s not about avoiding opioids. It’s about using them smarter. Your gut isn’t broken-it’s just been silenced. Give it the right signals, and it will wake up.
How long does postoperative ileus usually last?
Without intervention, POI typically lasts 3 to 5 days. With proper prevention-like early walking, gum chewing, and reduced opioids-it can be cut to 2 to 3 days. If it lasts longer than 5 days, other causes like bowel obstruction or infection should be ruled out.
Can I prevent postoperative ileus if I’m on opioids for pain?
Yes. Even if you need opioids, you can reduce your risk. Stick to the lowest effective dose, combine them with non-opioid pain relievers like acetaminophen or ketorolac, get up and walk within 4 hours after surgery, and chew gum several times a day. These steps cut POI risk by up to 35%.
Is methylnaltrexone safe for everyone?
No. Methylnaltrexone is not safe if you have a bowel obstruction, severe abdominal adhesions, or a known allergy to it. It’s also not recommended for low-risk patients who are on very low opioid doses. Always check with your doctor-your medical history matters more than the drug itself.
Why does chewing gum help after surgery?
Chewing gum tricks your brain into thinking you’re eating. That triggers the cephalic phase of digestion-signals that start saliva, stomach acid, and gut motility. Studies show patients who chew gum four times a day after surgery pass gas and have bowel movements nearly two days faster than those who don’t.
What’s the difference between POI and a bowel obstruction?
POI is a temporary lack of gut movement caused by surgery and opioids. A bowel obstruction is a physical blockage-like scar tissue, a hernia, or a tumor-that stops food and gas from moving. POI usually resolves with time and care. Obstruction needs imaging (like a CT scan) and often surgery. If you have severe pain, vomiting, or no gas/bowel movement for more than 5 days, get checked immediately.
How do I know if I’m getting too many opioids after surgery?
Track your total opioid dose in morphine milligram equivalents (MME). If you’re getting more than 40 MME in the first 24 hours, you’re at high risk for POI. For example, 10 mg of oxycodone = 15 MME, 10 mg of hydrocodone = 10 MME, 10 mg of morphine = 10 MME. Ask your nurse or doctor for your total MME-you might be surprised.






8 Comments
Opioids are a crutch. If your gut shuts down because of pain meds, maybe you shouldn't have had the surgery in the first place.
This is such a needed conversation! 🙌 I had POI after my appendix removal and honestly? Chewing gum was the only thing that helped me feel human again. My nurse laughed when I asked for a pack, but I chewed for 15 mins every 2 hours - and bam, gas by day 2. 🍬✨
Let me tell you - this is the kind of info that saves lives. I’m a nurse in a rural ER, and we see this ALL the time. Patients come in bloated, scared, and confused because no one told them opioids could do this. We started doing the ERAS bundle last year - pre-op acetaminophen, gum, walking by 4 hours - and our POI rates dropped from 38% to 14%. The best part? Patients are leaving happier, and we’re not drowning in extra bed days. It’s not magic. It’s just common sense. 💪
And yes, chewing gum works. It’s not a joke. It’s neuroscience. Your brain thinks you’re eating, so your gut wakes up. I’ve even seen patients who couldn’t pass gas for 4 days start moving after just one day of gum. No kidding.
But here’s the real win: when you cut opioids, pain doesn’t spike - it stabilizes. People think they need morphine to be comfortable, but they just need a plan. Acetaminophen + ketorolac + regional blocks? That’s the trifecta. I wish every surgeon read this.
And don’t even get me started on the cost savings. One patient saved us $3,200 in extra days. That’s a new wheelchair, or a month of insulin, or a family dinner. This isn’t just medicine - it’s justice.
Why are we still doing this the old way? We know better. Let’s stop pretending opioids are the only tool in the box.
Wow. So… we’re just supposed to chew gum instead of, I don’t know, treating pain? 😒 Like, sure, let’s all become little digestive puppets and chew our way to recovery while ignoring the fact that surgery HURTS. And what about people who actually need opioids? Are we just supposed to suffer so we can ‘optimize bowel motility’? This feels like medical virtue signaling wrapped in a Cochrane review. Also - ‘gum chewing’? That’s your solution? Next you’ll tell me to hug a tree and recite affirmations to stimulate peristalsis. 🙄
And don’t even get me started on ‘methylnaltrexone’ - $147.50 for a shot? That’s a luxury drug for people who can afford to not be poor. Meanwhile, rural hospitals are still using 1998 protocols. So… what? We just blame the patients? Or the nurses? Or the fact that capitalism won’t let us do what’s right? Yeah. I get it. The answer is always ‘more gum’.
I’m not saying this isn’t important - but we’re making it too complicated. If you’re on opioids after surgery, your gut will slow down. That’s biology. The real issue is that we’re still treating pain like it’s a problem to be erased, not managed. People need to accept that discomfort is part of healing. Maybe if we stopped trying to eliminate every sensation, we wouldn’t need all these interventions.
So let me get this straight - you’re telling me that hospitals are spending billions because doctors are too lazy to stop giving opioids? And the solution is… gum? And walking? That’s it? No wonder healthcare is broken. This isn’t prevention - it’s punishment. You’re asking patients to be their own physical therapists while their bodies are still bleeding. Who’s going to help the 78-year-old with arthritis who can’t even stand up? Who’s going to make sure they chew gum every 2 hours? This isn’t science - it’s guilt-tripping with a white coat.
And methylnaltrexone? That’s a Band-Aid on a gunshot wound. You’re treating the side effect instead of the cause - which is, of course, the opioid. So why not just… stop giving them? Oh right - because then patients will scream. And no one wants to hear that. So we give them a $150 shot and call it progress. Pathetic.
It’s funny how we treat the body like a machine - if it breaks, we fix it with a part. But the gut isn’t a valve. It’s a conversation. Between nerves, bacteria, stress, and memory. Opioids don’t just slow motility - they silence the whole dialogue. And gum? It’s not a trick. It’s a reawakening. The cephalic phase isn’t just about saliva - it’s about the body remembering how to be alive after trauma. We’ve forgotten that healing isn’t just chemical. It’s ritual. Walking. Chewing. Breathing. Presence.
Maybe the real problem isn’t opioids - it’s that we’ve lost touch with the body’s wisdom. We medicate instead of listen. We quantify instead of feel. And now we’re surprised when the gut shuts down?
AI predicts POI? Cute. But can it tell you when a patient’s eyes glaze over because they’re too tired to move? Can it hear the quiet sob when they say, ‘I just want to eat something real’? No. So don’t pretend tech is the answer. The answer is presence. And maybe - just maybe - a piece of gum.
The data is unequivocal. The implementation is abysmal. In the UK, we adopted ERAS protocols in 2019. Compliance in teaching hospitals: 89%. In district general hospitals: 31%. The disparity is not due to lack of evidence - it is due to institutional inertia, poor training, and a culture that still equates opioid administration with compassionate care. Methylnaltrexone is not a ‘luxury’ - it is a clinical necessity for high-risk patients. To deny it is not frugality - it is negligence. We must standardize, audit, and hold institutions accountable. The cost of inaction is measured not only in pounds and dollars - but in days lost, in dignity eroded, and in lives delayed. This is not a suggestion. It is a moral imperative.
Write a comment