Imagine you’re taking five different medications for three separate conditions. One doctor prescribed one pill, another added a second, and a third just changed the dose-without telling anyone else. You don’t know who to ask when you feel dizzy after dinner. This isn’t rare. It’s happening to millions of people right now.
Why Medication Communication Breaks Down
When you see multiple doctors, pharmacists, or specialists, each one focuses on their piece of your health. But rarely do they all talk to each other. A 2022 NIH study found that 68% of patients seeing more than one provider had at least one medication error because of poor communication. That means nearly seven in ten people are at risk of harmful drug interactions, missed doses, or dangerous overlaps-all because no one checked what everyone else was doing. The problem isn’t that providers are careless. It’s that the system doesn’t make it easy. Electronic health records (EHRs) don’t always talk to each other. A specialist at one hospital can’t see what your primary care doctor wrote in another system. And most patients don’t know how to fix it.The Four Essential Pieces of Every Medication List
If you’re managing multiple medications, the single most powerful tool you have is a clear, updated list. Not a scribble on a napkin. Not a note in your phone. A real, printed, always-current list with four key details for every drug:- Name (brand and generic, if applicable)
- Dosage (e.g., 10 mg, 500 mg)
- Frequency (e.g., once daily, two tablets at bedtime)
- Purpose (e.g., “for blood pressure,” “for nerve pain”)
Who Should Be on Your Care Team
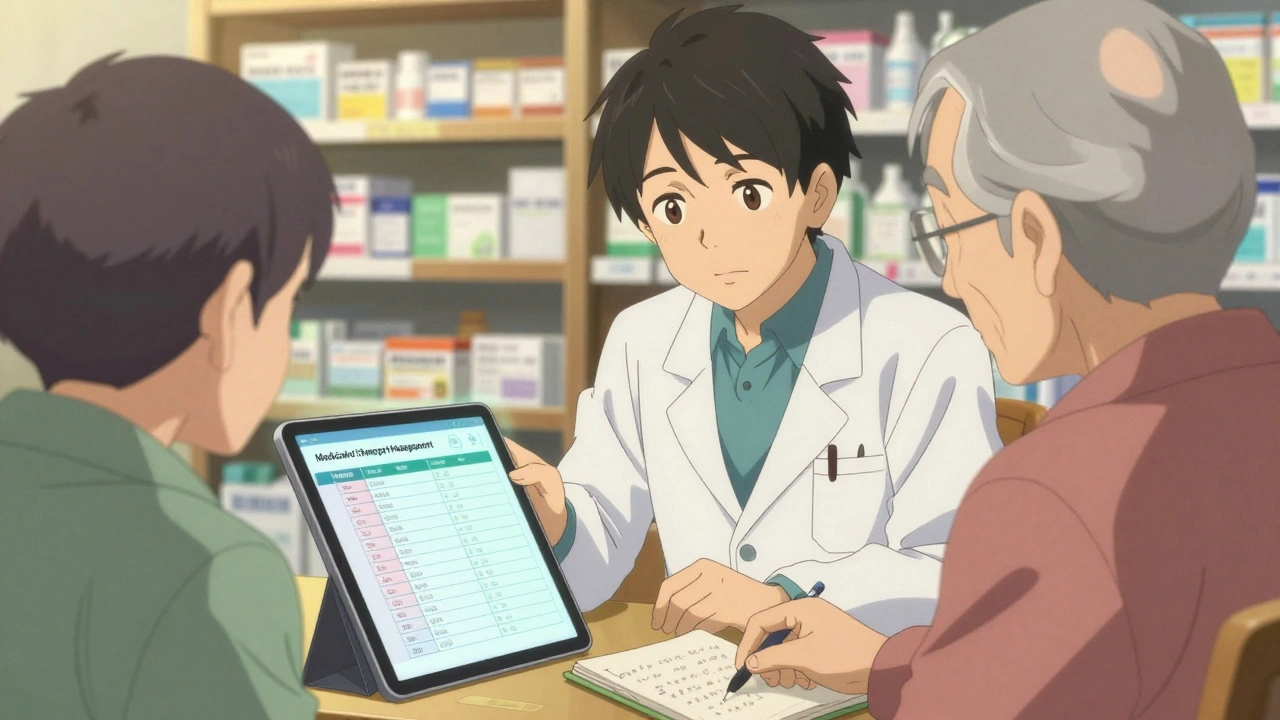
Your care team isn’t just your doctor. It’s your pharmacist, your nurse, your primary care provider, and even your family member who helps you organize pills. But one person should be your anchor: your primary care provider. They’re the only one who sees the full picture. Yet, a 2022 NIH study found that 57% of patients said specialists changed their medications without telling their main doctor. That’s dangerous. Specialists focus on one condition-like heart disease or diabetes-but they don’t always know about the other drugs you’re taking for anxiety, arthritis, or sleep. Pharmacists are your secret weapon. They’re trained to catch drug interactions before they happen. A 2023 analysis by Asteroid Health showed patients who worked directly with a clinical pharmacist had 32% higher adherence to their meds and 63% more confidence in their treatment plan. Many independent pharmacies now offer free Medication Therapy Management (MTM) services. Ask yours if they do it.How to Make Providers Talk to Each Other
You can’t force doctors to call each other. But you can create the conditions for it to happen. Start with this simple script at every appointment:- “Here’s my current medication list. Can you check if anything needs to change?”
- “Are you aware of any other providers prescribing me medication?”
- “Could you please share this list with my primary care doctor or pharmacist?”
The Teach-Back Method: Make Sure You Understand
Doctors give instructions fast. You nod. You leave. Then you’re confused. The Teach-Back Method fixes this. After your provider explains how to take a new medication, say: “Just to make sure I got this right-I’m supposed to take this pill every morning with food, right? And it’s for my joint pain, not my blood pressure?” This isn’t testing them. It’s helping them. AHRQ found this simple technique reduces misunderstandings by 45%. It also signals to providers that you’re paying attention-and that you expect them to be clear.Track Your Body’s Response
Medications don’t just affect your body-they affect your mood, sleep, energy, and digestion. Keep a simple journal. For one week, write down:- What you took and when
- Any new symptoms (dizziness, nausea, rash, trouble sleeping)
- Changes in appetite, mood, or energy
What Works: Integrated Care vs. Fragmented Care
Not all systems are equal. Accountable Care Organizations (ACOs)-groups of doctors and hospitals that share patient data and get paid for keeping people healthy-have dramatically better outcomes. CMS data shows ACO patients had 27% fewer hospital readmissions due to medication errors. Why? Because they have care coordinators who pull together all your records, check for conflicts, and make sure everyone’s on the same page. In contrast, patients in traditional fee-for-service systems-where each provider bills separately-are far more likely to get conflicting prescriptions. The same NIH study found patients with three or more providers were 3.2 times more likely to have dangerous medication overlaps. If you’re on Medicare, ask if your plan is part of a Shared Savings Program. You might already be in a coordinated system and not know it.
What’s Changing-and What’s Coming
The system is slowly improving. The 21st Century Cures Act required EHRs to share data-but only 38% of providers can actually do it reliably in 2025. That’s changing. CMS now requires all Primary Care First practices to implement structured medication reconciliation by January 2024. That means every time you move from hospital to home, or specialist to PCP, someone must check every pill you’re on. AI tools are also stepping in. At Mayo Clinic, new software now scans all your medications in under a minute and flags potential conflicts. That used to take 15 minutes per patient. Now it’s 47 seconds. And pharmacists? They’re becoming the new central hub. By 2025, 78% of independent pharmacies in the U.S. will offer formal medication reviews-free of charge. That’s up from 42% in 2022.Your Action Plan: 5 Steps to Take Today
You don’t need to wait for the system to fix itself. Here’s what you can do right now:- Make your list with the four key details (name, dose, frequency, purpose). Print it. Keep it in your wallet.
- Update it every time a new medication is added, changed, or stopped. Don’t wait for your next appointment.
- Ask every provider if they’ve seen your list-and if they’ve shared it with your primary doctor.
- Use Teach-Back after every new prescription. Say it out loud: “So I’m taking this for ______, ______ times a day, ______.”
- Find your pharmacist and ask if they offer Medication Therapy Management. If they do, schedule a free review.
What Happens When You Don’t Act
Medication errors cause 7,000 deaths a year in the U.S. alone. That’s not a statistic-it’s someone’s parent, sibling, or friend. Most of these deaths are preventable. They happen because no one asked, “What else are you taking?” You’re not being difficult by asking questions. You’re being smart. You’re the only person who’s with you every day. You’re the only one who knows how you feel. Your voice matters more than any algorithm or EHR. Don’t wait for a crisis. Start today. Update your list. Ask your next doctor: “Are you aware of what else I’m taking?”It’s not complicated. But it’s critical.
What should I do if my doctors don’t talk to each other?
You become the bridge. Bring your updated medication list to every appointment and ask each provider: “Can you please share this with my primary care doctor or pharmacist?” If they refuse, ask why. Write down their response. You have the right to coordinated care. If you’re on Medicare, contact your care coordinator or call 1-800-MEDICARE to report communication gaps.
Can my pharmacist really help with multiple prescriptions?
Yes-more than you think. Pharmacists are trained to spot drug interactions, duplicate therapies, and dangerous dosages. Many offer free Medication Therapy Management (MTM) services, where they review all your prescriptions, check for conflicts, and even call your doctors to suggest changes. In 2023, patients who used MTM had 32% better adherence and 63% higher confidence in their treatment. Ask your local pharmacy if they offer this.
How often should I update my medication list?
Every time something changes-whether it’s a new prescription, a dose change, or a medication you stopped. Don’t wait for your annual checkup. Keep the list in your wallet or phone, and update it immediately after any appointment or pharmacy visit. A 2023 Tulane University study showed patients who updated their list after every change had 37% fewer medication errors.
Why do specialists often prescribe without checking my other meds?
Specialists focus on one condition, and many EHR systems don’t share data between hospitals or clinics. A 2022 NIH study found that 57% of patients said specialists changed their meds without consulting their primary doctor. It’s not malice-it’s system failure. But you can fix it by bringing your list to every specialist visit and asking: “Have you seen my full medication list?”
Is there a free tool to help manage multiple medications?
Yes. The CDC and AHRQ offer free printable medication trackers online. Many pharmacies also give out simple forms. You can also use free apps like MyTherapy or Medisafe-but always print a hard copy to bring to appointments. Digital tools can fail. A printed list never does.
What if I’m confused about why I’m taking a certain pill?
Ask your pharmacist or primary care provider to explain the purpose of each medication. If you can’t name why you’re taking it, you’re at higher risk for side effects or stopping it accidentally. Write down the purpose on your list. If a provider can’t explain it clearly, that’s a red flag. Some medications are prescribed out of habit-not need. A 2022 deprescribing study found that nearly half of elderly patients were taking at least one unnecessary drug.






14 Comments
man i been there. five meds, three docs, zero communication. i just started carrying a folded paper in my wallet with the names, doses, and why i take em. last week my cardiologist spotted a duplicate and nixed one. felt like a superhero. no fancy app needed, just paper and guts to ask.
oh wow. another ‘patient empowerment’ manifesto. how quaint. the real issue? healthcare is a profit-driven dumpster fire. your ‘four-point list’ won’t fix a system where EHRs are built by vendors who think ‘interoperability’ is a yoga pose. you’re just teaching people to carry their own funeral planner.
list good. but docs dont care. they got 12 mins per pt. MTM? pharma shill program. ACOs? buzzword bingo. you think paper list fixes EHR fragmentation? lol. system is broken. you just bandaiding.
omg YES!! i use mytherapy app but also print it bc once my phone died and i was like 😵💫 in the ER and had no clue what i was on. my pharmacist even called my dr to fix a conflict!! she’s basically my healthcare wingman 💪💊
this is so important. i’ve been asking my docs to share lists since 2021. one said ‘we don’t do that’ and i just stared. then i emailed the clinic admin. they called me back in 2 days. turns out their EHR could do it-they just never trained staff. small push, big change. also, teach-back? game changer. now i say it out loud like i’m explaining to my dog.
Let me be clear: this entire post is a performative gesture of ‘patient advocacy’ that absolves the system of responsibility. You are not a ‘bridge.’ You are a data-entry clerk for a broken infrastructure. The fact that you’re expected to memorize, print, and evangelize your own pharmacokinetics is not empowerment-it’s institutional abandonment disguised as self-help. And don’t get me started on the ‘teach-back’ method-it’s just another way to make patients police their own medical negligence.
you people are ridiculous. if you can't manage your meds, maybe you shouldn't be on so many. i've been on 8 meds for 12 years and never had an issue. you just need discipline. stop blaming doctors. take responsibility. also, why do you need a list? just remember. it's not rocket science.
i read this and felt seen. not because i’m a medical expert, but because i’ve sat in waiting rooms wondering if the dizziness was from the blood pressure pill or the antidepressant or just… life. no one ever asks you how you feel between visits. this list isn’t about control-it’s about dignity. the fact that we have to fight to be heard says more about the system than it does about us. thank you for writing this. i’m printing mine today.
oh sweetie. you think your little printed list is going to make a difference? darling, your doctor’s EHR probably still uses a dial-up connection from 2007. and your ‘pharmacist’? they’re just the guy who hands you the pills and says ‘take two, not three, unless you’re in a hurry.’ this is theater. cute theater.
list good. ask questions. pharmacist helps. done. no need for drama. simple works.
the problem is not communication-it’s polypharmacy. you're overmedicated. 5 drugs? you're a walking clinical trial. the real solution? deprescribe. stop taking half of them. the system didn't fail you-you failed yourself by accepting prescriptions like they're free candy.
i cried reading this. not because it’s profound-but because i’ve been doing this for 7 years. my mom died from a drug interaction. they never asked her what she was taking. now i carry a laminated card. i’ve had doctors roll their eyes. i’ve had nurses thank me. i’m not brave. i’m just tired of losing people.
why is this even a thing? i mean, really? we’re living in 2025 and people still have to be their own case managers? my cousin got hospitalized because her cardiologist didn’t know she was on a new antidepressant. they said ‘oh, we didn’t have access.’ access? it’s 2025. we have self-driving cars. but not a single system that can share a pill list? i’m done. i’m moving to Canada. or Mars. anyone have a spare rocket?
you got this. start with the list. one step. one day. you’re not alone. i’m rooting for you 💖
Write a comment