Most people with cirrhosis don’t realize they’re at high risk for liver cancer-until it’s too late. Hepatocellular carcinoma (HCC) is the most common type of liver cancer, and over 80% of cases happen in people who already have cirrhosis. The good news? If caught early, HCC can often be cured. The bad news? Only about 40% of people with cirrhosis get screened regularly. That’s not because doctors don’t know what to do-it’s because the system is broken.
Why Surveillance Matters
If you have cirrhosis, your liver is scarred. That scar tissue doesn’t just slow down liver function-it creates the perfect environment for cancer to grow. HCC doesn’t show symptoms until it’s advanced. By then, treatment options shrink, and survival drops to under 20%. But if you’re screened every six months with an ultrasound, your chances of catching HCC early jump dramatically. Studies show that regular screening can boost 5-year survival from 10-20% to 50-70%.
That’s not a guess. It’s from a 2015 study in Hepatology that tracked over 1,000 cirrhotic patients. Those who stuck with surveillance lived about three months longer on average-and many lived years longer because their tumors were small, contained, and treatable.
Who Should Be Screened?
Not everyone with cirrhosis needs the same level of attention. Major guidelines agree on one thing: all adults with Child-Turcotte-Pugh (CTP) Class A or B cirrhosis should get screened every six months. That includes people with cirrhosis from hepatitis B, hepatitis C (even after cure), alcohol use, or fatty liver disease.
But here’s where it gets tricky. CTP Class C cirrhosis means your liver is failing. Median survival is less than two years. Most guidelines, including the American Association for the Study of Liver Diseases (AASLD), say screening isn’t useful here-unless you’re on a transplant list. The European Association for the Study of the Liver (EASL) took it further in 2023: they now recommend screening only for those with an annual HCC risk of 1.5% or higher.
That’s a game-changer. It means some people with cirrhosis-like those with mild, stable disease-might not need routine scans. But how do you know your risk? Tools like the aMAP score (using age, gender, albumin, bilirubin, and platelets) and the GALAD score (adding AFP-L3 and DCP markers) are being tested to predict who’s most likely to develop cancer. These aren’t standard yet, but they’re coming fast.
What Does Screening Look Like?
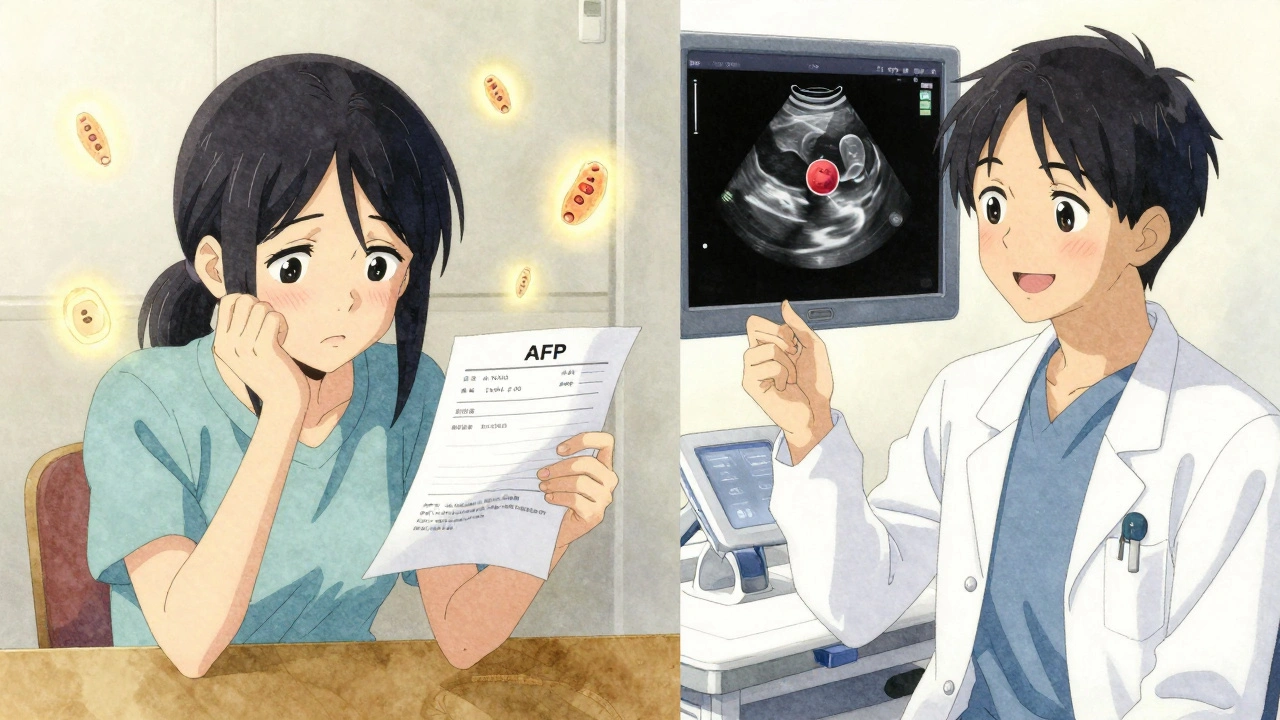
Ultrasound is the backbone of HCC surveillance. It’s cheap, safe, and widely available. The goal? Find any liver mass larger than 1 cm. If you see one, you move to the next step: a contrast-enhanced CT or MRI scan. These scans show how the tumor takes up blood-something HCC does differently than benign nodules.
Some centers add a blood test for alpha-fetoprotein (AFP). But it’s not reliable. AFP can be high in hepatitis flare-ups, pregnancy, or even just after drinking. The AASLD says it’s only a conditional recommendation, and only if levels go above 20 ng/mL. Even then, it’s not a diagnosis-it’s a red flag.
What you don’t want is to skip the scan because you think your liver feels fine. Or because your doctor didn’t bring it up. Or because you missed your last appointment. Nearly 30% of patients miss their surveillance scans. That’s not laziness-it’s often poor follow-up systems.
What Happens If Something Is Found?
If imaging shows a suspicious lesion, you’re not automatically facing a death sentence. The American College of Radiology’s LI-RADS system helps doctors classify findings. A LI-RADS 5 lesion means HCC is almost certain. LI-RADS 4 is highly suspicious. Both need treatment.
Early-stage HCC (BCLC Stage 0 or A) has several curative options:
- Resection: Removing the tumor. Only works if your liver is healthy enough to handle surgery.
- Liver transplant: Best option if you’re eligible. Removes the cancer and the damaged liver. But you need to be on a waitlist-and there’s a shortage of organs.
- Ablation: Burning or freezing the tumor. Done through the skin with a needle. Works best for tumors under 3 cm.
For patients who can’t have surgery or transplant, newer treatments like transarterial chemoembolization (TACE) or radioembolization can control growth for months or even years. These aren’t cures, but they keep people alive longer and improve quality of life.
Why Are So Many People Not Getting Screened?
It’s not a lack of knowledge. Hepatologists know the guidelines. A 2021 study found 92% of liver specialists were aware of them. But only 58% followed them consistently.
Here’s what’s really holding things back:
- No automated reminders: If your electronic health record doesn’t flag you for a scan, your primary care doctor won’t know you need one.
- Poor coordination: Cirrhosis patients often see multiple specialists. No one’s in charge of making sure surveillance happens.
- Patient barriers: Transportation, cost, fear, or misunderstanding. One nurse told me she spends 25 minutes per patient just explaining why the scan matters.
- Disparities: Black patients and those on Medicaid are half as likely to get screened as white, privately insured patients.
Programs that use patient navigators-people whose only job is to remind, schedule, and follow up-have cut missed appointments from 32% down to 14%. That’s not magic. It’s basic care coordination.

What’s Next for HCC Surveillance?
The future of HCC screening isn’t just better ultrasounds. It’s smarter tools.
AI-assisted ultrasound systems like Medtronic’s LiverAssist are already FDA-cleared. They help radiologists spot tiny tumors that the human eye might miss-boosting detection by nearly 20%. In five years, these could be standard in every clinic.
Then there’s MRI. Right now, it’s too expensive and time-consuming for routine use. But new abbreviated MRI protocols-done in 5 to 7 minutes-are cutting costs to under $400. By 2027, high-risk patients might get MRI instead of ultrasound every six months.
Biomarkers are also advancing fast. The GALAD score, which combines five blood markers, detects early HCC with 85% accuracy. The NIH is funding a $15 million study (HESBA) to validate 17 new biomarkers. One day, you might get a blood test every six months instead of an ultrasound.
The SURVIVE trial, launching in 2025, will compare standard screening to risk-based screening in 10,000 patients. If it works, guidelines will change. Screening won’t be for everyone with cirrhosis-it’ll be for those who need it most.
What Should You Do?
If you have cirrhosis:
- Ask your doctor: Am I on a surveillance plan?
- Confirm you’re getting an ultrasound every six months.
- Ask if your center uses LI-RADS for reporting.
- If you miss an appointment, reschedule immediately. Don’t wait.
- Find out if your hospital has a patient navigator for liver disease.
If you’re a caregiver or family member: Help them keep track. Set phone reminders. Drive them to appointments. This isn’t optional. It’s the difference between life and death.
HCC doesn’t have to be a death sentence. But it won’t be caught by accident. It takes action. It takes systems. And it takes people who refuse to let the system fail them.





9 Comments
This post is basically a 2000-word PSA and nobody’s doing anything about it. I’ve seen this exact scenario play out in my dad’s care-doc says 'get screened every six months,' then forgets to mention it again until the next visit. No reminders, no follow-up, just silence. Meanwhile, the cancer grows. It’s not negligence-it’s systemic laziness.
Let’s be clear: if you have cirrhosis and aren’t getting screened every six months, you’re playing Russian roulette with your liver. The data isn’t debatable-survival jumps from 10% to 70% with early detection. The fact that 60% of patients miss scans isn’t a healthcare failure-it’s a moral failure. We have the tools. We have the guidelines. We just don’t care enough to enforce them. And that’s unacceptable.
It’s fascinating how the shift from universal screening to risk-stratified approaches like the aMAP and GALAD scores reflects a broader evolution in precision medicine-moving away from one-size-fits-all protocols toward individualized risk assessment. While ultrasound remains the cornerstone, the integration of biomarkers and AI-enhanced imaging could significantly reduce false positives and unnecessary biopsies. Still, the real bottleneck isn’t technological; it’s logistical. Even the most accurate algorithm won’t help if the patient can’t get to the clinic, can’t afford the copay, or doesn’t understand why the scan matters. The human element remains irreplaceable.
my bro got diagnosed last year with hcc after 2 years of missing his ultrasounds. he thought he was fine ‘cause he wasn’t jaundiced or vomiting. turns out, liver cancer doesn’t give you a warning label. we found out about patient navs through the hospital and holy crap, they saved his life. they called, drove him, translated the docs, even helped him fight the insurance. if your clinic doesn’t have one, ask for one. it’s not a luxury-it’s a lifeline.
I’ve worked in liver clinics for over a decade, and I’ve seen too many patients slip through the cracks because no one was holding their hand. I’m not a doctor, but I’ve sat with people while they cried over their scan results, helped them write down questions for their hepatologist, and reminded them to bring their insurance card. It’s not glamorous, but it’s necessary. If you’re reading this and you’re a caregiver-you’re doing the most important job in the room. Keep showing up. Even if it’s just one text saying, 'Hey, your scan’s tomorrow. I’ll be there.' That’s how people survive.
in india we dont even have access to basic ultrasound in many rural areas let alone LI RADS or GALAD scores and yet we are told to follow american guidelines. my uncle has cirrhosis from hepatitis b and his village clinic has no machine no doctor no nothing. they tell him to go to delhi but he cant afford it. so what do we do? wait for the system to fix itself? or do we start community screening drives? i dont know but this post feels very rich person medicine
my mom got her first ultrasound last month after 4 years of cirrhosis. she was scared to go because she thought they’d just tell her she’s gonna die. turns out the doc found a 7mm nodule. they’re watching it. she’s alive. and honestly? i think she’s alive because i set a phone reminder. i know that sounds dumb. but it worked.
AI ultrasound tools are wild. my cousin’s radiologist used one and said it flagged a spot he totally missed. he was like, 'I’ve done 500 of these and that one slipped by.' now they’re using it on everyone. it’s not perfect, but it’s like having a second pair of eyes that never gets tired. also, if you’re scared of scans? just think of it as a video game where the boss is liver cancer and you’ve got a cheat code: every 6 months. press start.
in India we have no system no money no time but we have family. my father had cirrhosis from alcohol and I took him to the city every six months even though it took two trains and a day. I carried the reports I wrote down the dates I argued with the nurse. I did not wait for the system to work. I became the system. If you are reading this and you have a loved one with cirrhosis do not wait for the doctor to remind you. Be the reminder. Be the navigator. Be the one who says no we are not giving up. This is not about guidelines. This is about love
Write a comment