When it comes to losing weight with medication, the landscape has changed dramatically in just the last few years. If you’ve been following weight loss news, you’ve probably heard a lot about GLP-1 agonists-drugs like Wegovy, Zepbound, and Saxenda. They’re the new stars in town, promising dramatic results. But what about the older options you might have heard of before, like phentermine or orlistat? Are they still worth considering? The truth isn’t as simple as ‘newer is better.’ It’s about matching the right tool to your body, budget, and lifestyle.
How GLP-1 Agonists Actually Work
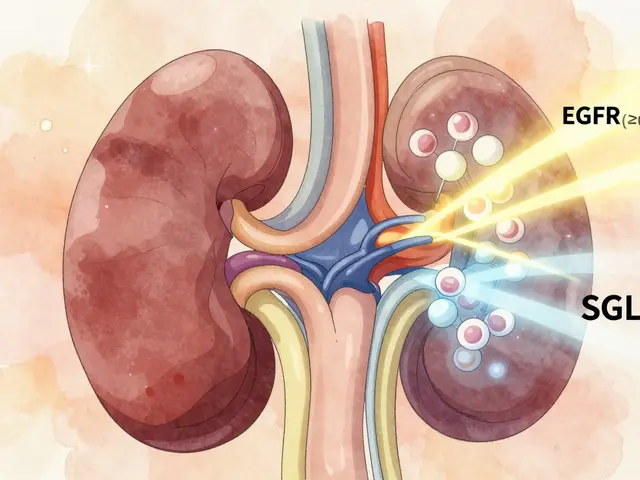
GLP-1 agonists don’t just suppress your appetite-they talk directly to your brain and gut. These drugs mimic a natural hormone called glucagon-like peptide-1, which your body releases after eating. This hormone tells your brain you’re full, slows down how fast your stomach empties, and helps your pancreas release insulin when needed. The result? You feel satisfied sooner, eat less, and your blood sugar stays steadier.
Drugs like semaglutide (Wegovy) and tirzepatide (Zepbound) are the most powerful in this class. In clinical trials, people lost an average of 15% to 21% of their body weight. That’s not a few pounds-it’s often 30 to 50 pounds or more. Tirzepatide, which also targets GIP (another gut hormone), pushed results even higher, with some users losing nearly 21% of their weight over a year. These aren’t just small improvements. They’re life-changing numbers for people with obesity.
What the Older Drugs Do-and Don’t Do
Before GLP-1 agonists, the main options were pills like orlistat (Xenical), phentermine-topiramate (Qsymia), and naltrexone-bupropion (Contrave). These work very differently. Orlistat blocks fat absorption in your intestines, so about 30% of the fat you eat passes through your body undigested. That means greasy stools, frequent bathroom trips, and the need to be very careful about your diet. It’s effective, but unpleasant for many.
Phentermine is a stimulant that reduces appetite by affecting brain chemicals. It’s been around since the 1950s and is still used, often short-term. Qsymia combines phentermine with topiramate, an anti-seizure drug that also reduces cravings. Contrave pairs an antidepressant (bupropion) with an opioid blocker (naltrexone) to target reward pathways in the brain. These drugs typically help people lose 5% to 10% of their body weight. That’s meaningful, but nowhere near the 15%+ seen with GLP-1 drugs.
Real-World Results Are Not What Trials Suggest
Here’s the catch: the numbers you see in clinical trials don’t always match what happens in real life. In trials, people are closely monitored, given support, and stick to the plan. Outside the lab, things get messy. A 2024 study from NYU Langone Health followed over 50,000 people on GLP-1 drugs and found that after six months, the average weight loss was only 4.7%. After a full year, it rose to 7%. That’s still better than most older drugs, but far below the 15-20% seen in trials.
Why the drop? Two big reasons: side effects and cost. Nausea, vomiting, and stomach discomfort affect 20% to 50% of users, especially when starting or increasing the dose. Many people can’t tolerate it and quit. And then there’s the price. Without insurance, Wegovy or Zepbound can cost $1,300 a month. Even with coupons, most people still pay hundreds out of pocket. Many insurance plans only cover these drugs if you have diabetes or a BMI over 40. For people with a BMI of 32 or 35 without other health issues, getting coverage is often impossible.
Cost and Access: The Hidden Barrier
Older medications are a different story. Phentermine costs $10 to $50 a month. Orlistat (Alli, the over-the-counter version) runs about $40 a month. Qsymia and Contrave are pricier-around $100 to $150-but still far below GLP-1 drugs. Insurance coverage for older drugs is also much more consistent. Many plans cover them with low copays, even for weight loss alone.
But here’s the irony: even though older drugs are cheaper and easier to get, they’re being prescribed less. In early 2024, IQVIA reported that GLP-1 agonists made up 78% of all new weight loss prescriptions. The rest? Only 15% went to older pills. Why? Because doctors and patients are drawn to the higher results-even if they’re harder to sustain.
Administration: Injections vs. Pills
Another big difference? How you take them. GLP-1 agonists like Wegovy and Zepbound are injected once a week. Saxenda requires a daily shot. That’s a hurdle for people who hate needles or have trouble with injections. Even though the needles are small and the process is simple, the psychological barrier is real.
Older drugs? All are pills. You take them once or twice a day with water. No training needed. No supplies to carry. For many, that simplicity makes a huge difference in sticking with treatment.
Who Benefits Most From Each Option?
If you’re looking for the biggest possible weight loss and can handle injections, side effects, and high costs, GLP-1 agonists are your best shot. They’re especially helpful if you also have type 2 diabetes-these drugs improve blood sugar and protect your heart, too.
If you’re more concerned about cost, don’t want injections, or have mild to moderate weight to lose, older drugs might still be the right fit. Phentermine can give you a quick jump-start. Orlistat works if you’re willing to cut back on fatty foods. Qsymia and Contrave offer solid results with less risk than surgery.
And if you’ve tried everything and still haven’t reached your goals? Bariatric surgery remains the most effective long-term solution. A 2024 study showed people who had surgery lost 24% of their body weight after two years-nearly triple what most people achieve with GLP-1 drugs alone.
Side Effects: What to Expect
GLP-1 agonists come with a well-known set of side effects: nausea, vomiting, constipation, diarrhea, and sometimes dizziness. These are usually worst during the first few weeks as your body adjusts. Most people get used to them. But for some, the discomfort is too much. One Reddit user described feeling like they had gastroparesis-food just sat in their stomach for hours. That’s rare, but it happens.
Older drugs have their own issues. Orlistat causes oily spotting and urgent bowel movements. Phentermine can raise your heart rate and blood pressure, so it’s not safe for people with heart problems. Qsymia carries a black box warning for birth defects-women must use birth control while taking it. Contrave can increase the risk of seizures and suicidal thoughts in rare cases.
There’s no perfect drug. The goal is to find the one that balances results with tolerability.
What’s Next? The Future of Weight Loss Drugs
The pipeline is full of new options. Retatrutide, a triple agonist that hits GLP-1, GIP, and glucagon receptors, showed 24.2% weight loss in early trials. MariTide, a new antibody therapy, is now in Phase 3 testing and could be a game-changer. These drugs may offer even better results with fewer side effects.
But the big question isn’t just about science-it’s about access. Will insurance ever cover GLP-1 drugs for more people? Will prices drop when patents expire after 2030? Will generics become available? Until then, these drugs remain out of reach for many who could benefit.
What Should You Do?
If you’re considering weight loss medication:
- Start with your doctor. Don’t self-prescribe or buy online. These are prescription drugs for a reason.
- Ask about insurance coverage. Find out if your plan requires prior authorization or has BMI restrictions.
- Be honest about your tolerance for side effects and injections.
- Think long-term. Weight loss drugs work best when paired with lifestyle changes. Stop the drug, and most people regain the weight.
- Consider all options. Surgery, older pills, and GLP-1 drugs aren’t rivals-they’re tools in a larger toolkit.
There’s no single best drug. The best one is the one you can stick with-and that’s different for everyone.
Are GLP-1 agonists better than older weight loss drugs?
Yes, in terms of weight loss effectiveness. GLP-1 agonists like Wegovy and Zepbound typically lead to 15-21% body weight loss in trials, while older drugs like orlistat or phentermine usually result in 5-10%. However, GLP-1 drugs require weekly injections, cost over $1,000 a month, and cause more side effects like nausea. Older drugs are cheaper, taken as pills, and may be better for people who can’t tolerate injections or have limited insurance coverage.
Can you take GLP-1 agonists without having diabetes?
Yes. Wegovy and Zepbound are FDA-approved specifically for chronic weight management in adults with obesity or overweight, even without diabetes. However, insurance often requires a diagnosis of obesity (BMI ≥30) and sometimes a related condition like high blood pressure or sleep apnea to approve coverage. Some doctors prescribe them off-label for people with lower BMIs, but insurance may deny payment.
How long do you need to take GLP-1 agonists?
These drugs are meant for long-term use. Weight loss stops when you stop taking them-most people regain the weight within a year of discontinuation. Studies show up to 70% of users stop within the first year due to cost, side effects, or lack of results. If you find a drug that works and you can afford it, continuing indefinitely is often the best way to maintain weight loss.
Why are GLP-1 agonists so expensive?
GLP-1 agonists are biologic drugs, meaning they’re made from living cells, which makes them complex and costly to produce. Companies like Novo Nordisk and Eli Lilly have invested billions in research and development. Without generic competition, they set high prices. Monthly costs range from $1,000 to $1,400, and insurance often doesn’t cover them for weight loss alone. Patient assistance programs exist but have income limits and annual caps.
Do older weight loss drugs still work?
Yes, but results are more modest. Orlistat helps people lose 5-10% of body weight by blocking fat absorption. Phentermine-topiramate (Qsymia) and naltrexone-bupropion (Contrave) typically lead to 8-10% weight loss. They’re less effective than GLP-1 drugs but are far cheaper, easier to access, and taken as pills. For people who can’t use or afford GLP-1 drugs, they remain valid, evidence-based options.
Is bariatric surgery better than GLP-1 drugs?
For people with severe obesity (BMI ≥40), surgery typically leads to greater and more lasting weight loss. One study found bariatric surgery patients lost 24% of their body weight after two years, compared to 4.7% for GLP-1 users after six months. Surgery also has lower long-term costs and better durability. However, it’s invasive, carries surgical risks, and requires major lifestyle changes. GLP-1 drugs offer a non-surgical alternative for those who want significant weight loss without surgery-but results are less predictable and harder to maintain without ongoing treatment.





1 Comments
omg i just started semaglutide last month and wow the nausea hit me like a truck but i kept going and now im down 12lbs and my jeans fit like they used to in 2019 🥲
Write a comment