When you’re taking a medication like levothyroxine for hypothyroidism or phenytoin for epilepsy, your life depends on consistency. A tiny change in dosage - even 5% - can trigger a seizure, send your thyroid levels into chaos, or cause dangerous side effects. These are NTI drugs - narrow therapeutic index medications - and they’re not like other prescriptions. Yet, many insurance plans still treat them like ordinary drugs, forcing patients through layers of paperwork just to get the brand-name version they need.
What Makes NTI Drugs Different?
NTI drugs have a razor-thin margin between a safe, effective dose and a toxic one. The FDA defines them as medications where small changes in blood concentration can lead to serious therapeutic failure. That’s not a minor risk. It’s life-or-death. Levothyroxine, carbamazepine, warfarin, digoxin, and cyclosporine are all on this list. There are about 37 of them in total, according to DrugBank. For most drugs, generics are safe, effective, and cheaper. But for NTI drugs, even minor differences in fillers, coatings, or absorption rates between brand and generic versions can cause problems. A patient stable on brand-name levothyroxine for years might suddenly see their TSH levels spike 300% after switching to a generic. That’s not theoretical. It’s documented in real patient data.Why Do Insurers Even Ask for Prior Authorization?
Insurance companies use prior authorization to control costs. For most brand-name drugs with generic alternatives, they’ll deny coverage unless you prove you’ve tried the cheaper version first. It’s called step therapy. But NTI drugs break that rule. Some insurers, like Health Net, explicitly say brand-name NTI drugs don’t need prior authorization at all. They’re listed on higher tiers because they’re more expensive - not because they’re restricted. Other plans, however, still require paperwork. Why? Because many insurers don’t distinguish between NTI drugs and regular ones. They apply blanket policies designed for cost savings, not patient safety. This inconsistency is dangerous. A patient in Alabama might get brand-name Keppra approved instantly. A patient in Texas might wait three weeks for a denial, only to appeal and get approved - after a seizure.The Human Cost of Delays
The numbers don’t lie. A 2024 survey by Patients Rising found that 68% of patients on NTI drugs faced prior authorization delays longer than 72 hours. Nearly 30% reported a direct health event - hospitalization, seizure, or overdose - because they couldn’t get their medication on time. One neurologist on Reddit shared that 73% of their levothyroxine brand requests were initially denied. That’s not bureaucracy. That’s negligence. When a patient’s thyroid hormone levels swing wildly, it doesn’t just cause fatigue or weight gain. It can lead to heart arrhythmias, depression, or even myxedema coma - a rare but fatal condition. The American Academy of Neurology studied 2,450 epilepsy patients and found that unnecessary barriers to brand-name antiepileptics contributed to preventable seizures in 18.7% of cases. That’s nearly 1 in 5 people. Meanwhile, insurers argue that prior authorization prevents overuse. Dr. Mark Linetsky from Prime Therapeutics claims these processes save health plans $2.3 billion annually. But that math ignores the cost of emergency visits, ICU stays, and lost workdays caused by medication switches. The real cost isn’t in the drug price - it’s in the human toll.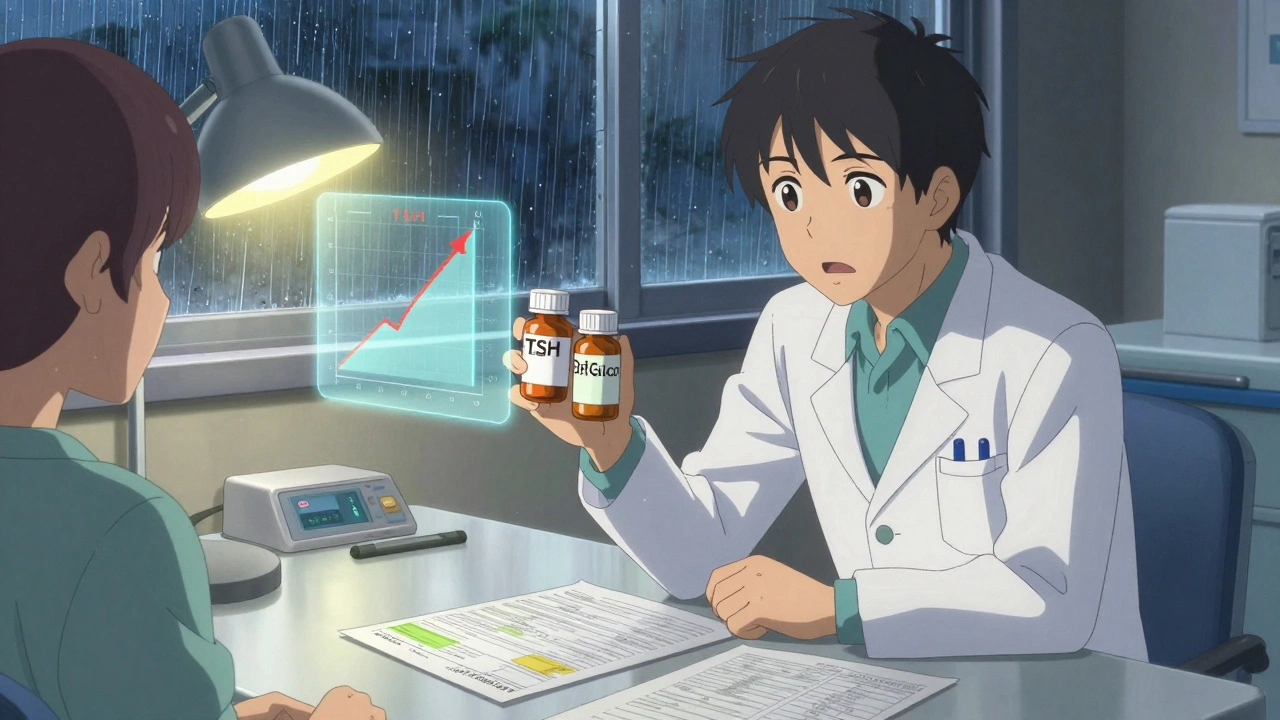
How the System Actually Works (For Prescribers)
If your insurance requires prior authorization for an NTI drug, here’s what you’ll need:- A completed form - often the insurer’s own, sometimes a universal form like Mississippi’s
- Lab results showing unstable thyroid, seizure frequency, or drug levels
- Proof of prior generic failure - like a TSH level that jumped after switching
- Weight, height, and clinical diagnosis details
State Laws Are Starting to Change Things
By 2025, 22 states have passed laws to protect NTI drug access. California’s AB-1428, effective January 1, 2025, bans prior authorization for NTI drugs if the patient was previously stable on the brand-name version. That’s huge. It removes the burden from the doctor and the patient. Eighteen states now require automatic approval if the insurer doesn’t respond within the legal timeframe - up from just seven in 2022. In Mississippi, Medicaid must respond to urgent NTI requests in 24 hours. In North Carolina, if you write “medically necessary” on the prescription, the insurer must cover it. Medicare Advantage plans are also changing. The Improving Seniors’ Timely Access to Care Act, passed in April 2024, mandates real-time electronic decisions - including for NTI drugs. That means no more waiting 48 hours for a phone call.
What You Can Do Right Now
If you’re on an NTI drug and your insurer is making you jump through hoops:- Check your plan’s formulary. Look for the drug name and see if it says “prior authorization required.”
- Ask your pharmacist if the drug is on the NTI exception list. Some plans have internal lists you can’t see online.
- Get your lab results - TSH, INR, drug levels - and bring them to your doctor. Concrete numbers help.
- Use electronic prior authorization if your doctor’s office offers it. It’s 42% faster than fax.
- If denied, appeal immediately. Most approvals happen on appeal.
The Future Is Changing - But Not Fast Enough
Industry analysts predict that by 2026, 75% of commercial insurers will eliminate prior authorization for established NTI drugs. Why? Because the evidence is overwhelming. The cost of delays is higher than the cost of the drug. The risk is too great. But until then, patients are stuck in a broken system. A system that treats a life-threatening condition like a budget line item. A system that lets algorithms decide whether you get your seizure medicine - or your thyroid pill - on time. The truth is simple: NTI drugs aren’t a cost-saving opportunity. They’re a medical necessity. And if your insurer still treats them like any other brand-name drug, you’re not just fighting paperwork. You’re fighting for your health.What are NTI drugs?
NTI drugs, or narrow therapeutic index drugs, are medications where even small changes in dosage or blood concentration can lead to serious side effects or treatment failure. Examples include levothyroxine for thyroid conditions, phenytoin for epilepsy, and warfarin for blood clotting. These drugs require precise dosing and are not interchangeable with generics in many cases.
Why do insurers require prior authorization for brand-name NTI drugs?
Some insurers require prior authorization for brand-name NTI drugs because they apply standard cost-control policies designed for regular medications, even though NTI drugs are different. They may not recognize that switching to a generic can cause dangerous fluctuations in drug levels. However, many insurers - including Health Net - do not require prior authorization for NTI drugs, recognizing their unique risks.
Can I switch from a brand-name NTI drug to a generic without risk?
For many patients, switching from a brand-name NTI drug to a generic can cause dangerous changes in drug levels. Studies show that patients on levothyroxine or antiepileptics often experience unstable lab results, increased seizures, or hospitalizations after switching. The FDA and medical societies warn against automatic substitution for these drugs without clinical oversight.
How long does prior authorization for NTI drugs usually take?
On average, prior authorization for NTI drugs takes 3.2 business days, according to the Journal of Managed Care & Specialty Pharmacy. Electronic submissions are faster, but NTI requests still take 22% longer than standard ones due to extra documentation. In urgent cases, Medicaid plans must respond within 24 hours and provide a 72-hour supply if needed.
What should I do if my insurance denies my NTI drug request?
Appeal immediately. About 82.4% of NTI drug prior authorization requests are approved after an initial denial. Gather lab results, your doctor’s note explaining why the brand is medically necessary, and any history of problems with generics. Use your insurer’s formal appeal process - don’t wait. If you’re in a state with automatic approval laws, mention them in your appeal.
Are there states that protect access to brand-name NTI drugs?
Yes. As of 2025, 22 states have laws limiting prior authorization for NTI drugs. California’s AB-1428 bans prior authorization for stable patients already on brand-name NTI drugs. Eighteen states require automatic approval if insurers don’t respond within mandated timeframes. Medicaid programs in states like Mississippi and North Carolina also have specific protections.
Can my doctor help me avoid prior authorization?
Yes. Your doctor can request the brand-name drug directly and include clinical documentation - like lab results showing instability after a generic switch - to support the request. Some insurers waive prior authorization if the prescription clearly states “medically necessary” or if the patient has a history of adverse reactions to generics. Electronic prior authorization systems also speed up the process.





13 Comments
This is insane. People are dying because some insurance algorithm thinks levothyroxine is just another pill. We're not talking about aspirin here. We're talking about brain seizures and heart failure. And they make you fill out forms? Like this is a DMV appointment?
I've been on brand-name levothyroxine for 12 years. Switched to generic once because my plan forced it. My TSH went from 2.1 to 8.9 in three weeks. I was exhausted, depressed, gained 20 pounds, and my heart started skipping. Took three appeals and two ER visits to get back on brand. No one in insurance understands that this isn't about cost. It's about survival. And they wonder why people hate the system.
Oh look another crybaby with a thyroid problem. The system isn't broken it's working exactly as designed. If you can't afford your meds get a better job. Or move to Canada where they give out insulin like candy. Maybe if you stopped being so entitled you wouldn't need a $100 pill to feel normal.
As someone from Ireland where we have free meds for chronic conditions I can't believe how broken the US system is. I had a friend with epilepsy who had to wait 17 days for a prescription because of prior auth. She had a seizure in a supermarket. No one should have to risk their life because some bean counter thinks generics are good enough. This isn't healthcare it's corporate hostage taking.
Let me get this straight. You're telling me that in 2025 we're still arguing whether a thyroid pill should be covered without a 3-week bureaucratic ballet? The FDA has a whole list of these drugs. Doctors know. Pharmacists know. But the insurance CEOs? They're still stuck in 1998 thinking 'generic equals cheaper equals better'. It's not stupidity. It's malice disguised as efficiency.
Look I get it. But this is why America needs to stop coddling people. If you can't afford your meds then you're not working hard enough. We have a $400 billion pharmaceutical industry and you're whining about $100 pills? Get a second job. Sell your phone. Move to a cheaper state. Stop expecting the government to fix your poor life choices.
I'm a nurse in rural Ohio and I see this every single week. One lady came in crying because she ran out of her seizure meds and had to drive 90 miles to the nearest neurologist just to get a letter to appeal. She missed three days of work. Her kid had to stay home from school. And the insurance denied it again. This isn't about money. It's about dignity. We're treating human beings like insurance forms.
According to CMS data, prior authorization saves $2.3 billion annually. The cost of hospitalizations from NTI switches is estimated at $1.1 billion. So the system is net positive. Also 78% of NTI drug switches are successful without issue. The outliers are rare. Stop sensationalizing. This isn't a crisis. It's a cost-control mechanism.
Wait so you're saying if I switch from brand to generic I might have a seizure? But what if I just take a little more? Or maybe I can just split the pill? I did that with my blood pressure med and it worked fine. Are you sure it's not just anxiety? Maybe you're just stressed and blaming the pill?
Let me offer a Hegelian perspective: the insurance system is the thesis, patient suffering is the antithesis, and the synthesis is inevitable reform. But only if we recognize that capitalism commodifies health. NTI drugs expose the moral bankruptcy of market-driven medicine. We must transcend the binary of brand vs generic and embrace a new paradigm of therapeutic equity.
My sister is on carbamazepine. She switched to generic and had three seizures in two months. We appealed. Got approved on the third try. Took 47 days. Her employer threatened to fire her for missing too much work. Now she's on disability. This isn't just paperwork. It's a life derailer. And the worst part? No one at the insurance company even knows what NTI means.
For those struggling: talk to your pharmacist. Ask if your plan has an NTI exception list. Most do but it's not on the website. Call the insurer directly and say 'I'm requesting an NTI drug exception under state law XX'. Mention California AB-1428 even if you're not in CA. It often triggers faster review. And if denied, appeal with lab results. 82% win on appeal. You're not alone. We've been there.
Everyone is acting like this is a new problem. Newsflash: generics have been around since the 70s. If you can't handle a 5% variation in absorption then maybe you're not stable enough to be on these drugs in the first place. Stop blaming insurers. Blame your doctor for letting you get dependent on a brand-name drug. There's a reason generics exist. To save money. And you're wasting it.
Write a comment