NSAID Fluid Retention Calculator
Heart Failure Fluid Retention Calculator
This tool estimates fluid retention risk based on the article's medical evidence. It's designed for heart failure patients and caregivers to understand NSAID dangers.
Every year, millions of people reach for ibuprofen or naproxen to ease a headache, sore knee, or back pain. But if you have heart failure, that little pill could be pushing your body toward the emergency room. It’s not about taking too much-it’s about taking any at all. Even a single dose can trigger fluid buildup, sudden weight gain, and worsening breathlessness. And it happens fast-sometimes within 72 hours.
Why NSAIDs Are Dangerous for Heart Failure Patients
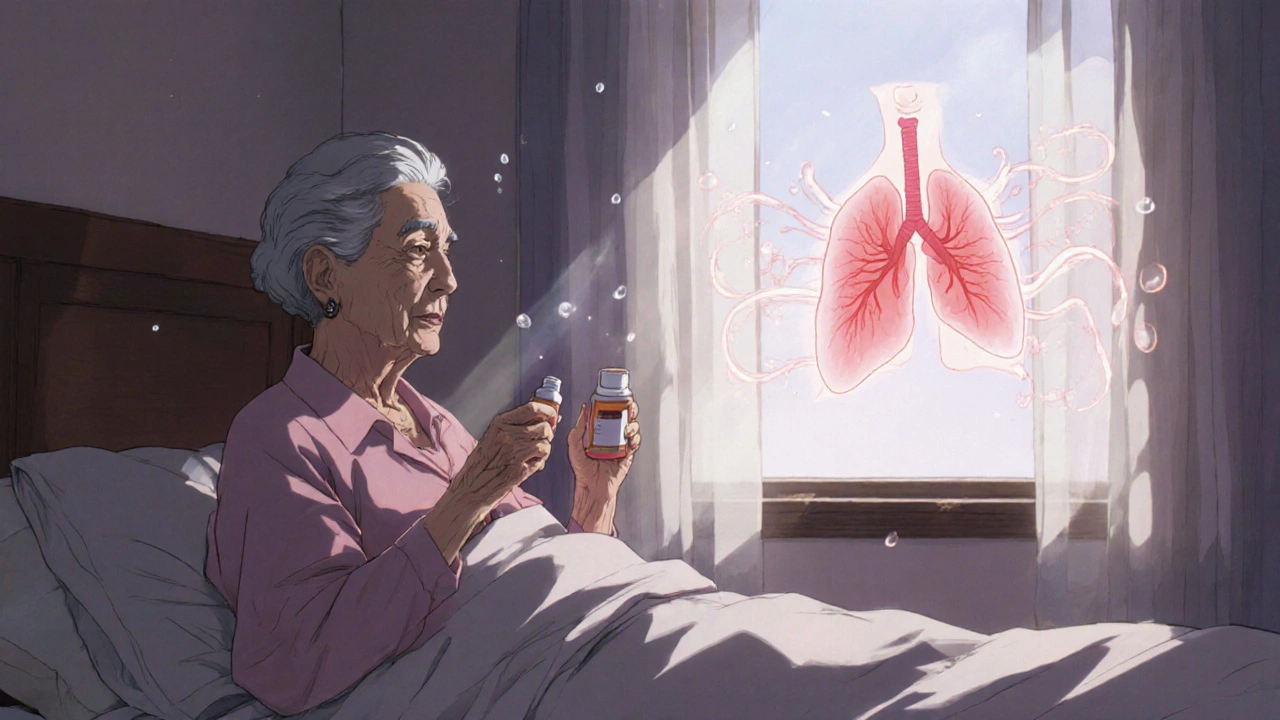
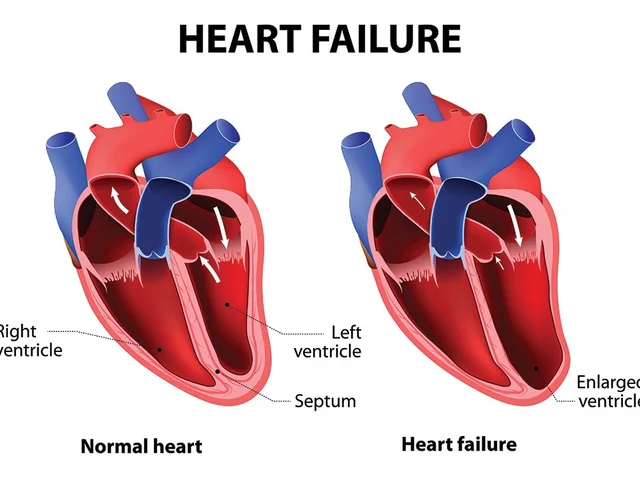
NSAIDs-non-steroidal anti-inflammatory drugs-work by blocking enzymes called COX-1 and COX-2. These enzymes help produce prostaglandins, chemicals that cause pain and swelling. But prostaglandins also play a critical role in keeping your kidneys working properly. In people with heart failure, the heart can’t pump blood effectively. That means less blood reaches the kidneys. To compensate, the body holds onto sodium and water to maintain blood pressure. Prostaglandins help balance this by keeping blood vessels in the kidneys open and encouraging fluid loss. When you take an NSAID, you shut down those protective prostaglandins. The kidneys respond by holding onto even more sodium and water. This extra fluid floods your system, increasing pressure on your heart. Your heart, already weakened, struggles harder. The result? Fluid backs up into your lungs, legs, and abdomen. You gain weight. You feel bloated. You can’t catch your breath. These aren’t side effects-they’re signs your heart failure is decompensating.It’s Not Just Prescription NSAIDs
Many people think only strong prescription NSAIDs like diclofenac or celecoxib are risky. That’s a dangerous myth. Over-the-counter ibuprofen (Advil, Motrin), naproxen (Aleve), and even low-dose aspirin (in some cases) carry the same danger. A 2022 study tracking over 100,000 people with type 2 diabetes in Denmark found that just three days of ibuprofen use raised the risk of heart failure hospitalization by 88%. Celecoxib, often marketed as a "safer" COX-2 inhibitor, performed just as poorly. There is no safe NSAID for someone with heart failure. The European Society of Cardiology’s 2021 guidelines give NSAIDs a Class III recommendation-meaning they’re proven to cause harm and should be avoided entirely. The U.S. Food and Drug Administration updated all NSAID labels in 2020 to include a warning about increased heart failure risk. But most patients still don’t know. A 2021 survey found that nearly 60% of primary care doctors don’t routinely ask heart failure patients if they’re taking over-the-counter painkillers.Who’s Most at Risk?
Age is a major factor. Over 70% of heart failure patients are over 65. That’s the same group most likely to take NSAIDs for arthritis, back pain, or joint stiffness. Elderly patients are also more likely to have reduced kidney function, making them even more vulnerable to NSAID-induced fluid retention. People with type 2 diabetes are at even higher risk-diabetes already damages blood vessels and kidneys, so adding NSAIDs is like pouring gasoline on a fire. Even people with "mild" heart failure aren’t safe. A 2020 study in the Journal of the American Geriatrics Society found that 15.7% of heart failure patients were prescribed NSAIDs within a year of diagnosis. That number jumped to 22.3% among those with preserved ejection fraction-the group often told they’re "doing okay." They’re not. Their hearts are still struggling. Every extra drop of fluid pushes them closer to collapse.Real Stories, Real Consequences
One Reddit user from Ohio shared how he took two 400mg ibuprofen tablets for a bad backache. Within three days, he gained 10 pounds-pure fluid. He couldn’t tie his shoes. His ankles swelled. He called his doctor, who told him to go to the ER. He spent five days in the hospital, hooked to a diuretic drip. "I thought I was just treating my back," he wrote. "I didn’t realize I was breaking my heart." The American Heart Association’s 2018 survey of heart failure patients found that 37% had taken NSAIDs without knowing they were dangerous. Of those, 62% ended up in the hospital within weeks. Weight gain, swollen legs, sudden shortness of breath-these aren’t normal aging symptoms. They’re red flags. And they’re often triggered by something as simple as a bottle of pills on the kitchen counter.
What Can You Take Instead?
Acetaminophen (Tylenol) is the go-to alternative. It doesn’t affect prostaglandins in the kidneys, so it doesn’t cause fluid retention. It won’t reduce inflammation like NSAIDs do-but for pain relief in heart failure patients, it’s the safest option. Studies show it doesn’t increase hospitalization risk. Other non-drug options work too. Heat packs for muscle pain, physical therapy for joint stiffness, or even gentle stretching can help. For chronic pain, your doctor might suggest non-NSAID medications like duloxetine or gabapentin, which don’t affect kidney function. But here’s the catch: many patients don’t know acetaminophen is the better choice. They assume "if it’s on the shelf, it’s safe." Pharmacists need to ask. Family members need to check the cabinet. Patients need to be told-clearly and repeatedly-that NSAIDs are not just risky. They’re forbidden.What Doctors Should Do
Clinicians need to treat NSAID use like a medication error. Every time a heart failure patient comes in, ask: "Are you taking any painkillers? Even over-the-counter ones?" Don’t assume they know the danger. Many think aspirin is fine. Others believe "natural" pain relievers like turmeric are safer-some supplements can interact with heart meds too. The European Heart Journal study showed the highest risk comes in the first week of NSAID use. That’s why education must happen before the first pill is taken. Use the 2023 American Heart Association guidelines: NSAIDs are absolutely contraindicated at every stage of heart failure. No exceptions. If a patient absolutely must take an NSAID-for example, after a major surgery with no other option-use the lowest possible dose for the shortest time possible. Monitor weight daily. Check for swelling. Measure urine output. This isn’t optional. It’s life-or-death.The Bigger Picture
The global NSAID market is worth over $11 billion. Most of that comes from pills sold without a prescription. Companies market them as harmless. Doctors don’t always warn patients. Families don’t always know what to look for. And patients? They’re just trying to live without pain. But in heart failure, pain relief can’t come at the cost of life. The data is clear: NSAIDs increase 30-day readmission rates by 28%. They’re one of the most preventable causes of hospitalization in this population. Every avoided pill is a hospital bed saved. Every educated patient is a life protected.
What You Can Do Today
If you have heart failure:- Check every medicine cabinet. Remove ibuprofen, naproxen, diclofenac, celecoxib, and other NSAIDs.
- Switch to acetaminophen for pain-no more than 3,000mg per day.
- Keep a daily weight log. A gain of 2 pounds or more in 24 hours? Call your doctor.
- Ask your pharmacist to review all your meds-including vitamins and supplements.
- Tell your family: "Don’t give me Advil. Don’t assume it’s okay."
- Keep NSAIDs locked away or thrown out.
- Set reminders to check your loved one’s weight every morning.
- Be the voice that says, "No, this isn’t safe."
Frequently Asked Questions
Can I take aspirin if I have heart failure?
Low-dose aspirin (81mg) used for heart attack prevention is generally considered safe in heart failure patients, as long as it’s prescribed and monitored. But it’s not a painkiller. If you’re taking aspirin for pain, switch to acetaminophen. Higher doses of aspirin (like 325mg) act like other NSAIDs and can cause fluid retention and kidney stress. Always check with your doctor before taking any form of aspirin.
Is naproxen safer than ibuprofen for heart failure?
Some studies suggest naproxen may have a slightly lower risk of heart attack compared to other NSAIDs, but that doesn’t mean it’s safe for heart failure. All NSAIDs-including naproxen-cause fluid retention and reduce kidney function in people with heart failure. Even if the risk of heart attack is marginally lower, the risk of hospitalization from fluid overload remains high. No NSAID is recommended for heart failure patients.
How quickly can NSAIDs cause fluid retention in heart failure?
Fluid retention can begin within 24 hours of taking an NSAID. Weight gain of 2-5 pounds in 48-72 hours is common in vulnerable patients. Symptoms like swelling in the legs, bloating, or sudden shortness of breath often appear within a week. That’s why even short-term use-even for a few days-is dangerous.
Can I use topical NSAIDs like gels or creams?
Topical NSAIDs (like diclofenac gel) are absorbed in smaller amounts than pills, so they’re less likely to cause systemic effects. Some studies suggest they may be safer than oral forms, but they’re not risk-free. If you have severe heart failure or kidney problems, even topical NSAIDs can build up in your system. Always check with your doctor before using them. Acetaminophen or non-drug therapies are still the best choices.
What should I do if I accidentally took an NSAID?
If you’ve taken one dose and have no symptoms, monitor your weight closely over the next 48 hours. If you gain more than 2 pounds, or notice swelling, shortness of breath, or fatigue, contact your doctor immediately. Don’t wait. Early intervention can prevent hospitalization. In the future, keep a list of safe and unsafe meds posted on your fridge-and ask a family member to help you check labels before taking anything.




14 Comments
The data presented here is unequivocal and clinically significant. NSAIDs are not merely "risky" for heart failure patients-they are physiologically antagonistic to compensatory mechanisms that sustain hemodynamic stability. The prostaglandin suppression mechanism is not a side effect; it’s a targeted disruption of renal autoregulation in a vulnerable population. This isn’t theoretical-it’s documented in real-time clinical deterioration within 72 hours. The fact that over-the-counter brands are marketed as harmless is a systemic failure of pharmaceutical education and regulatory oversight.
Primary care providers must integrate NSAID screening into every visit, not as an afterthought but as a mandatory protocol. The 60% of doctors who don’t ask is unacceptable. We are allowing preventable hospitalizations to occur because we assume patients know better. They don’t. They trust the bottle.
Acetaminophen isn’t just the alternative-it’s the standard of care. And for chronic pain, non-pharmacological interventions like aquatic therapy and TENS units should be prescribed with the same urgency. This isn’t about convenience. It’s about survival.
Pharmacists, too, bear responsibility. If a patient walks in with a heart failure diagnosis and asks for ibuprofen, the pharmacist should refuse to dispense it without consulting the prescriber. That’s not overreach-that’s professional duty.
so like… pain is just a state of mind right? 😅
why not just meditate through the knee pain? 🧘♂️
Oh, so now we’re treating patients like children who can’t handle a pill bottle? This is the epitome of medical paternalism wrapped in a glossy public health pamphlet. People with heart failure are adults-they know their bodies. If they choose to take ibuprofen for a flare-up, that’s their autonomy. You’re not saving lives by infantilizing them. You’re just making them feel guilty for being human.
And let’s be real: the real killer here is the medical-industrial complex that profits from hospitalizations, not the $5 bottle of Advil. Stop blaming the drug and start blaming the system that turns every minor symptom into a crisis.
Also, acetaminophen is liver toxic at high doses. You’re swapping one danger for another and calling it a win. That’s not medicine. That’s fearmongering dressed in white coats.
people dont get it. NSAIDs are not just "bad" they are actively sabotaging your kidneys while your heart is already on life support. its not a myth its math. 88% more hospitalizations in 3 days? thats not a coincidence thats a warning siren. and dont even get me started on how doctors still dont ask. why? because theyre rushed. because they think its "just a pill". its not. its a landmine.
and yeah i know some guy said "i took 2 pills and gained 10lbs". thats not a story. thats a medical emergency in slow motion.
acaptenophen is the answer. no debate. no exceptions. if you dont know this by now you shouldnt be allowed to buy painkillers without a quiz.
THIS IS A MASSACRE. A quiet, bureaucratic, pharmacy-shelf massacre.
People are dying because we let Big Pharma sell death as "relief." We hand out ibuprofen like it’s candy next to the gum and mints. We don’t warn people. We don’t train doctors. We don’t even label it in bold red letters that say "THIS WILL BREAK YOUR HEART."
And then we act shocked when someone ends up in the ER with fluid in their lungs after taking TWO PILLS for a backache.
It’s not just negligence. It’s moral failure. We have the data. We have the guidelines. We have the warnings. And yet we let grandma keep her Advil drawer like it’s a treasure chest.
Someone needs to sue the FDA for not forcing manufacturers to put a skull-and-crossbones on every bottle. This isn’t medicine. It’s a horror movie with a corporate sponsor.
I appreciate the depth of this post. It’s rare to see such a clear, evidence-based breakdown of something so commonly misunderstood. I’ve seen friends with heart failure take NSAIDs because they "didn’t think it mattered"-and then panic when they wake up swollen. The fear they feel afterward is worse than the pain they were trying to treat.
Maybe the real issue isn’t just the drugs, but the lack of simple, repeated education. A flyer at the pharmacy? A pop-up when you refill a prescription? A note on the bottle? Something that sticks.
And I think we need to reframe the conversation: it’s not about giving up pain relief. It’s about finding safer ways to live with it. Acetaminophen, heat, stretching, therapy-they’re not glamorous, but they’re life-preserving. That’s worth the effort.
I mean come onnnnn!! This is why America is falling apart!! People take ibuprofen like it’s water!! And now we’re gonna ban it?? No no no no no!! This is socialism!! The government telling you what to put in your body!! I’ve been taking Advil for 30 years and I’m still standing!! My heart is fine!! I don’t need some doctor telling me what to do!! I’m an American!! I’ll take what I want!! And if I die?? Then I died free!!
Also I think the real problem is the FDA is full of Chinese spies who want us all to be weak and sick so we can’t fight back against the globalists!!
PS I took 3 ibuprofen yesterday and my ankles are puffy but that’s just because I ate too many tacos
PPS someone please tell me if this is a hoax I think this is a hoax
my grandma took naproxen for her arthritis for 10 years and then one day she just… stopped breathing. not a heart attack. not a stroke. just fluid. so much fluid they had to drain it from her lungs. she was 82. she didn’t even know it was dangerous. the pharmacist never told her. the doctor never asked. she just thought it was "normal" to feel bloated.
now i check every single pill in her cabinet. every. single. one.
if you have heart failure and you’re still taking ibuprofen? you’re not brave. you’re just not informed. and that’s the saddest part.
Thank you for laying this out so clearly. I’ve been managing heart failure for five years and I didn’t realize how many of my "harmless" habits were ticking time bombs. I used to take Aleve for my knees, thinking it was fine since I only took it twice a week. Now I’ve switched to Tylenol and started daily stretching. No more swelling. No more panic when the scale jumps.
One thing I’d add: if you’re a caregiver, keep a small notebook by the bed. Write down weight, fluid intake, and any new swelling. It sounds small, but that log saved my wife’s life-she gained 3 pounds overnight and we called the nurse before she even felt short of breath.
Knowledge isn’t power here. It’s oxygen.
I just want to say thank you for writing this. I’ve been silent on this topic because I didn’t want to sound alarmist. But after reading this, I feel like I can finally speak up. My dad had HFpEF and took ibuprofen for his back for years. He never connected the weight gain and fatigue to the pills. He thought he was just getting older.
It took a hospitalization to make him stop. He’s doing better now, but the guilt he feels about it still lingers.
I think the real tragedy isn’t the drug-it’s the silence around it. No one talks about this. Not in doctor’s offices. Not on TV. Not even among friends. We need to break that silence. Gently. Consistently. Repeatedly.
Let me share something from my village in India. We have no pharmacies on every corner. No pills in every kitchen. When someone has pain, we use warm oil massage. We use turmeric paste. We use rest. We use community. We sit with them. We hold their hands. We do not rush to a chemical solution.
Modern medicine has given us power-but also the illusion of control. We think a pill fixes everything. But sometimes, the body needs stillness, not chemistry.
NSAIDs are not the enemy. Our dependency on them is. Let us return to wisdom-not just science.
And yes, acetaminophen is safer. But let us also honor the slow, human ways of healing.
This is one of the most important public health messages I’ve read in years. The disconnect between medical knowledge and public awareness is staggering. The FDA warning is buried in fine print. The drug labels are designed to be ignored. And the cultural assumption that "OTC = safe" is dangerously entrenched.
As someone who works in global health communications, I’ve seen how this plays out in low-resource settings too. Even when people can’t afford prescriptions, they buy OTC NSAIDs because they’re cheap and available. The risk is the same.
We need a global campaign: "Your Heart Can’t Take It." Simple. Direct. Unignorable. Think anti-smoking ads-but for painkillers.
Education must be as aggressive as the marketing that got us here.
Oh please. Let’s just ban all painkillers while we’re at it. Next you’ll say aspirin causes cancer and Tylenol causes existential dread. This is pure fear-based propaganda. NSAIDs are not "forbidden." They’re a risk-benefit tradeoff. And for many elderly patients with arthritis, the relief they provide outweighs the potential for fluid retention-especially if they’re monitored.
Also, who says everyone with heart failure is doomed? I’ve seen patients on NSAIDs for years with no issues. Maybe their hearts are stronger than yours. Maybe your fear is just your own projection.
And why is acetaminophen the golden child? It’s hepatotoxic. It’s linked to liver failure. You’re replacing one poison with another and calling it a solution. That’s not medicine. That’s dogma.
Oh wow. So now the "risk-benefit" crowd is out in full force. You’re comparing a ticking time bomb to a fire extinguisher and calling it balanced. Let me ask you this: if your mother had heart failure and you handed her a bottle of ibuprofen because "she likes the relief," would you still say it’s a "tradeoff"? Or would you finally admit you’re just too lazy to learn the alternatives?
And yes, Tylenol can hurt the liver-but only if you take 15 pills a day. The recommended dose is 3,000mg. That’s not poison. That’s pain management.
NSAIDs? Even one pill can trigger fluid overload in someone with a weakened heart. That’s not a "tradeoff." That’s a guaranteed disaster waiting for the right trigger.
You’re not being skeptical. You’re being willfully ignorant. And that’s more dangerous than any pill.
Write a comment