When you're taking a direct oral anticoagulant (DOAC) like apixaban, rivaroxaban, dabigatran, edoxaban, or betrixaban, it's not just about popping a pill every day. These medications are powerful-designed to prevent dangerous clots in people with atrial fibrillation, deep vein thrombosis, or after certain surgeries. But here’s the catch: DOACs don’t play well with every other drug you might be on. Even if your doctor says they’re safer than warfarin, ignoring interactions can land you in the ER with uncontrolled bleeding-or worse, a stroke.
Why DOAC Interactions Matter More Than You Think
Unlike warfarin, which needs frequent blood tests and strict diet restrictions, DOACs were marketed as "set it and forget it." But that simplicity is misleading. DOACs work best when their concentration in your blood stays within a narrow range. Too little? Risk of clotting. Too much? Risk of bleeding. And many common medications can throw that balance off. The problem? Most people on DOACs are older and managing multiple conditions. Studies show the average patient takes five or more other drugs. That’s not unusual-it’s the norm. And each of those drugs could be quietly changing how your DOAC works.How DOACs Are Processed: The CYP3A4 and P-gp Connection
To understand interactions, you need to know how DOACs move through your body. Two systems do most of the work: the CYP3A4 enzyme and the P-glycoprotein (P-gp) transporter. Think of them as your body’s cleanup crew and security gate. - CYP3A4 breaks down certain drugs in your liver and gut. Rivaroxaban relies on this enzyme for about half its clearance. Apixaban uses it for 20-25%. Dabigatran, edoxaban, and betrixaban? Barely at all. - P-gp pumps drugs out of cells, especially in the gut and kidneys. It affects all DOACs except betrixaban. If something blocks P-gp, your DOAC builds up. If something boosts it, your DOAC gets flushed out too fast. That’s why drugs that interfere with these systems are dangerous. A single medication can turn a safe dose into a risky one.High-Risk Medications That Can Clash with DOACs
Some drugs are red flags. Avoid or adjust carefully.- Dronedarone (used for irregular heartbeat): Strongly blocks P-gp. Don’t take it with dabigatran or rivaroxaban. With edoxaban, cut the dose to 30 mg daily. Apixaban and betrixaban are safer options here.
- Amiodarone: Moderately blocks P-gp. Can raise DOAC levels. Monitor for bruising, dark stools, or unusual fatigue.
- Diltiazem and Verapamil: Both are calcium channel blockers used for high blood pressure or angina. Diltiazem moderately blocks CYP3A4 and weakly blocks P-gp. Verapamil mainly blocks P-gp. For dabigatran, reduce the dose to 110 mg twice daily. Apixaban and rivaroxaban usually don’t need changes-but check with your pharmacist.
- Strong CYP3A4 or P-gp inducers: These include rifampin, St. John’s wort, carbamazepine, and phenytoin. They make DOACs less effective. Avoid them entirely. If you must use them, switch to warfarin under close supervision.
It’s Not Just Prescription Drugs
Over-the-counter meds and supplements can be just as risky.- NSAIDs (ibuprofen, naproxen): Don’t mix them with DOACs unless absolutely necessary. They don’t change DOAC levels, but they irritate your stomach lining. Combine that with thin blood? Higher chance of GI bleeding.
- SSRIs (like sertraline or fluoxetine): These antidepressants affect platelets. They don’t alter DOAC concentration, but they add to bleeding risk. If you’re on both, watch for nosebleeds, gum bleeding, or prolonged bruising.
- St. John’s wort: This herbal supplement boosts CYP3A4 and P-gp. It can slash DOAC levels by up to 50%. One study showed patients on rivaroxaban and St. John’s wort had clotting events within weeks. Don’t take it.
- Grapefruit juice: Blocks CYP3A4 in the gut. Can raise rivaroxaban and apixaban levels. Avoid large amounts. A glass now and then? Probably fine. A whole pitcher daily? Risky.
DOACs Are Not All the Same
You can’t treat them like interchangeable pills. Each has its own interaction profile.| DOAC | Main Metabolism Pathway | High-Risk Interactions | Best Alternative When Interactions Are Present |
|---|---|---|---|
| Apixaban | CYP3A4 (20-25%), P-gp | Dronedarone, amiodarone, strong inducers | Often safest choice with moderate interactions |
| Rivaroxaban | CYP3A4 (50%), P-gp | Dronedarone, rifampin, St. John’s wort, grapefruit juice | Avoid if on strong CYP3A4 inhibitors |
| Dabigatran | P-gp (primary) | Dronedarone, verapamil, amiodarone, ketoconazole | Dose reduction to 110 mg twice daily often needed |
| Edoxaban | P-gp | Dronedarone, verapamil, amiodarone | Reduce dose to 30 mg daily with strong P-gp inhibitors |
| Betrixaban | P-gp | Similar to edoxaban | Less commonly used; monitor closely |
When to Worry About Bleeding (And What to Do)
If you’re on a DOAC and start taking a new drug, watch for these signs:- Unexplained bruising or large bruises
- Bleeding gums when brushing teeth
- Nosebleeds lasting longer than 10 minutes
- Dark, tarry stools or blood in urine
- Headaches, dizziness, or sudden weakness (possible brain bleed)
Renal Function Changes Everything
Your kidneys clear most DOACs. If your kidney function drops-even slightly-your DOAC builds up. That’s why dosing is often lowered in people with moderate kidney disease. But here’s the twist: if you’re on a drug that also harms your kidneys (like NSAIDs or certain antibiotics), your DOAC level can spike even if your dose hasn’t changed. That’s a double hit. Always check your eGFR (kidney function test) when starting or stopping other meds.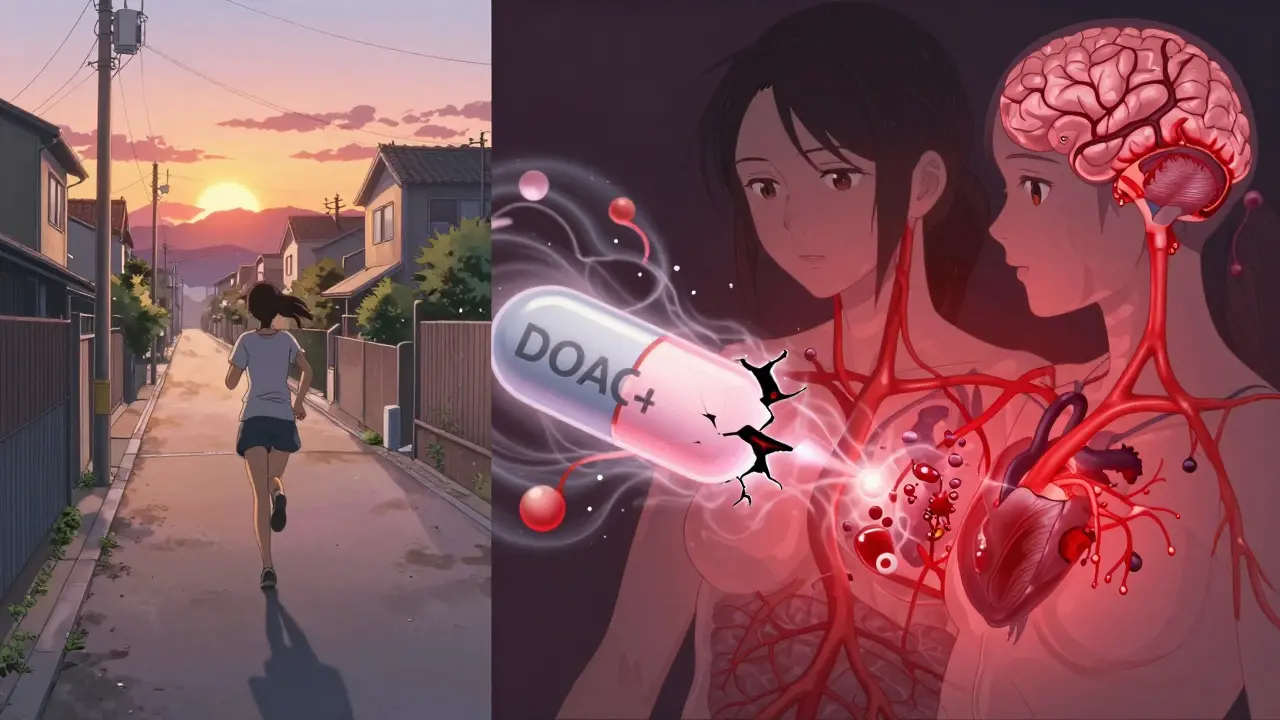
What Your Pharmacist Can Do That Your Doctor Might Not
Doctors are busy. Pharmacists? They’re trained to spot interactions. Every time a new prescription comes in, ask your pharmacist to run a DOAC interaction check. Use tools like Micromedex or Lexicomp-they flag risks in seconds. Also, bring a list of everything you take: vitamins, herbal teas, CBD oil, even antacids. Some antacids (like those with magnesium or aluminum) can reduce dabigatran absorption if taken too close together. Space them out by 2 hours.What’s Next? Personalized Dosing and Monitoring
Right now, we guess DOAC doses based on weight, age, and kidney function. But that’s not enough. Two people with the same profile can have wildly different drug levels. Researchers are exploring therapeutic drug monitoring (TDM) for DOACs-like how we check levels for warfarin or lithium. Early studies show it’s possible. But we don’t have clear guidelines yet. Until then, the best strategy is prevention: know your meds, know your risks, and never assume a new drug is "safe."Bottom Line: Stay in Control
DOACs are a big step forward-but they’re not foolproof. The biggest danger isn’t the drug itself. It’s the hidden interactions you didn’t know about.- Always tell every new provider you’re on a DOAC.
- Ask your pharmacist to check every new prescription.
- Never start or stop anything without checking first-not even aspirin.
- Keep a written list of all your meds and supplements.
- Know the signs of bleeding and act fast.




14 Comments
Been on apixaban for 3 years now. My pharmacist flagged diltiazem as a potential issue when I started it for blood pressure. I didn’t even realize it could mess with my anticoagulant. Always ask your pharmacist. They’re the real MVPs.
It is imperative to underscore the significance of pharmacokinetic interactions in the context of direct oral anticoagulants. The modulation of CYP3A4 and P-glycoprotein pathways by concomitant medications constitutes a clinically significant risk factor for hemorrhagic or thrombotic events. Vigilant medication reconciliation is not merely advisable-it is obligatory.
THE PHARMA COMPANIES DON’T WANT YOU TO KNOW THIS 😱
They made DOACs so you’d forget to check interactions… then you bleed out and they make billions off the ER visit. St. John’s wort? They banned it in Europe for a reason. And grapefruit juice? That’s not a fruit-it’s a Trojan horse. 🚨💊
so like… i read this and i’m like ok but what if ur on like… a lil bit of cbd oil? i mean it’s just for sleep right? but then i saw the part about p-gp and i started sweating. like… is my lavender tea gonna make me bleed internally?? 🤯
The structural and metabolic distinctions among DOACs necessitate individualized clinical consideration. While apixaban demonstrates a relatively favorable interaction profile due to its lower dependence on CYP3A4, the pharmacodynamic variability across populations remains underappreciated in primary care settings. Standardized screening protocols are urgently required.
I’ve seen too many people get scared and quit their meds because they read something online. DOACs are safe if you’re smart. Talk to your pharmacist. Don’t take NSAIDs. Avoid St. John’s wort. Keep a list. Done. Simple.
Apixaban’s 20–25% CYP3A4 metabolism makes it less susceptible than rivaroxaban (50%) to strong inhibitors. However, concomitant P-gp inhibition-e.g., from dronedarone-still requires dose adjustment. Clinical guidelines (ACC/AHA 2023) recommend apixaban as first-line in polypharmacy patients with moderate renal impairment and concomitant P-gp inhibitors.
My dad was on rivaroxaban and started taking ibuprofen for his arthritis. Two weeks later, he had a GI bleed. We didn’t know it was the combo. He’s fine now, but… man. I wish someone had just sat us down and said: ‘Don’t mix these.’ This post? Lifesaver.
Why are we letting Big Pharma sell us these time bombs? In America, we’re just supposed to trust the script? No thanks. I’d rather take warfarin and get tested every week than risk bleeding out because some guy in a lab didn’t test for grapefruit juice.
It is a profound failure of modern medical education that patients are left to navigate pharmacokinetic interactions without adequate guidance. The proliferation of DOACs without corresponding public health infrastructure for medication reconciliation represents a systemic negligence. The onus should not be placed on the elderly patient to memorize CYP3A4 substrates. This is not empowerment-it is abandonment dressed in wellness jargon.
ok but what if ur on a magic mushroom tea and also a doac? like… i heard the mushrooms reset your brain but what if they reset your liver too?? 🤔 i think the gov is hiding the truth about psilocybin and blood thinners…
I’m from Kenya and we don’t have easy access to DOACs here. Most people are on warfarin. But when I moved to the US and got prescribed apixaban, I was shocked how little people knew about interactions. This post should be required reading for every new patient. Thank you.
My eGFR dropped from 65 to 52 last year. My doctor cut my edoxaban dose without me asking. That’s good care. Always get your kidney numbers checked when starting or changing meds.
DOACs are just a way for Big Pharma to replace warfarin with something more expensive and less controllable. They don’t care if you bleed-they care if you buy the next bottle. And don’t even get me started on how they push grapefruit juice ads while hiding the interaction. Wake up, sheeple.
Write a comment