Imagine taking two pills at the same time - one for your blood pressure, another for your depression - and not realizing they’re fighting over the same metabolic highway inside your liver. That’s exactly what happens with CYP450 enzymes. These proteins don’t just break down drugs; they decide whether your medication works, fails, or turns toxic. And they’re always busy. About 90% of the pills you take rely on them to get processed. When two drugs show up at once, one often wins - and the other gets stuck, backed up, or burned out.
Who Are the CYP450 Enzymes?
CYP450 enzymes are a family of liver proteins that act like molecular scissors for drugs. They don’t just chop things up - they transform them so your body can flush them out. The six big players handle nearly all of it: CYP3A4 (50% of drugs), CYP2D6 (25%), CYP2C9 (15%), CYP2C19 (10%), CYP1A2 (5%), and CYP2E1 (4%). CYP3A4 alone processes more medications than all the others combined. It’s the busiest intersection in your body’s drug highway.
These enzymes aren’t just in your liver. About 20-30% of CYP3A4 activity happens in your gut. That’s why grapefruit juice can wreck your statin - it blocks the intestinal version of CYP3A4, letting too much drug into your bloodstream. A single glass can raise simvastatin levels by 30-80%. That’s not a myth. It’s science. And it’s dangerous.
How Do Drugs Compete?
Think of CYP450 enzymes as a limited number of parking spots. Only one car can park in each spot at a time. If you arrive in a flashy sports car (a strong inhibitor), it doesn’t just take a spot - it blocks the whole lot. That’s what happens when you take clarithromycin (an antibiotic) with simvastatin (a cholesterol drug). Clarithromycin binds tightly to CYP3A4, shutting down the enzyme’s ability to process simvastatin. The result? Simvastatin builds up. Muscle breakdown. Rhabdomyolysis. Kidney failure. A 72-year-old woman in a 2022 case study developed this after just three days of combining the two.
Not all competition is that dramatic. Sometimes it’s a slow traffic jam. SSRIs like fluoxetine or paroxetine are moderate CYP2D6 inhibitors. When paired with metoprolol (a beta-blocker), they slow down metoprolol’s breakdown. Nurses report this combo causes bradycardia in 15-20% of patients. Heart rate drops. Dizziness follows. It’s not rare. It’s predictable.
Inhibition vs. Induction: Two Opposite Problems
There are two main ways drugs mess with CYP450: inhibition and induction. Inhibition is like putting a roadblock. Induction is like widening the highway - but too wide.
Inhibition is immediate. It happens when one drug grabs the enzyme’s active site and won’t let go. Reversible inhibition (like fluvoxamine blocking CYP1A2) can cause drug levels to spike within hours. A Reddit user shared how adding fluvoxamine to theophylline therapy caused levels to jump from 10 to 25 mcg/mL - triggering seizures. That’s a 150% increase. One pill. One interaction. One ER visit.
Induction is sneakier. It takes days. Drugs like rifampin (an antibiotic for TB) or St. John’s wort (a herbal supplement) tell your liver to make more CYP3A4 enzymes. Over 3-14 days, your body starts breaking down drugs faster. Birth control pills? They stop working. Cyclosporine? Transplant rejection risk soars. Warfarin? INR plummets. The effect lasts weeks after you stop the inducer. People think they’re safe after quitting St. John’s wort - but the enzyme levels don’t drop overnight.
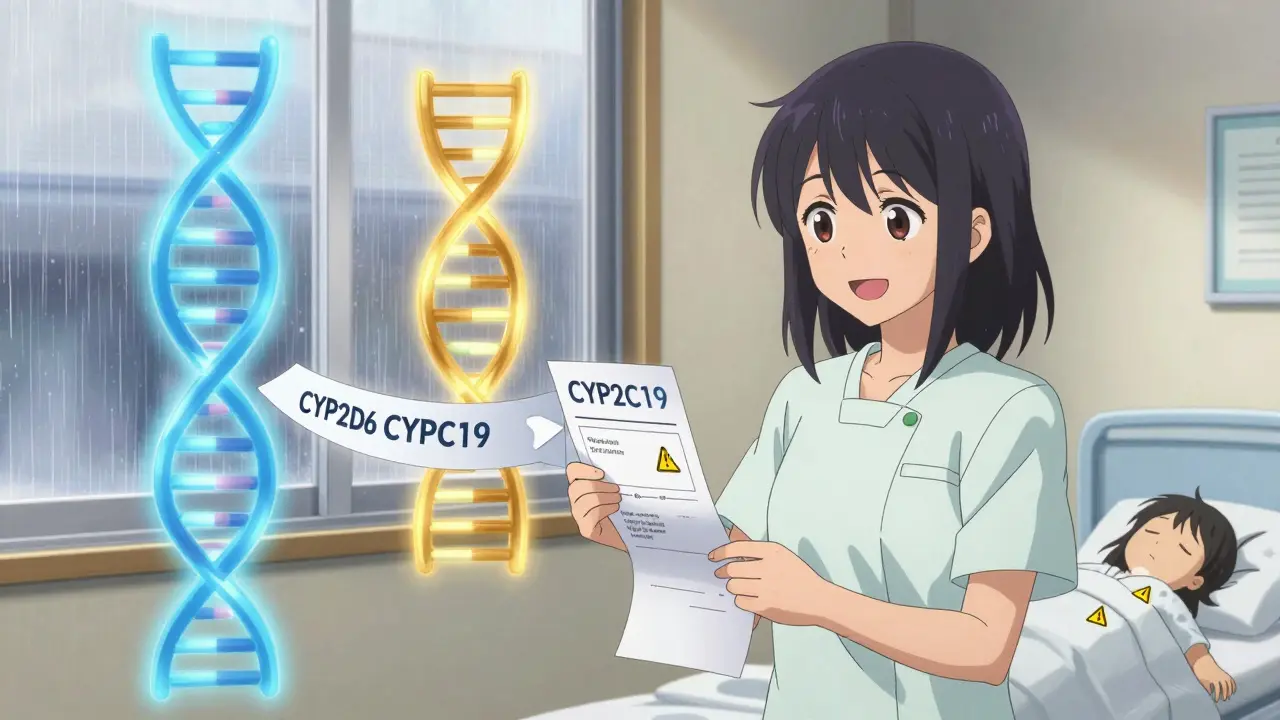
Genetics: Why Your Friend’s Pill Works and Yours Doesn’t
Two people can take the exact same dose of a drug - and one gets sick, the other feels nothing. Why? Genetics.
CYP2D6 is the poster child for this. About 7% of white people are poor metabolizers - their bodies barely touch the enzyme. For them, codeine doesn’t turn into morphine. No pain relief. Meanwhile, ultrarapid metabolizers (1-10% of populations, higher in North Africa and the Middle East) convert codeine to morphine too fast. They get high. Or worse - they overdose on a standard dose.
Same with clopidogrel. It’s a prodrug. It needs CYP2C19 to activate. But 30% of Caucasians and 60% of Asians are intermediate or poor metabolizers. They get the pill. They don’t get the protection. Their stents clot. The FDA recommends testing before prescribing it. Yet most doctors still don’t.
These genetic differences explain why 40-95% of drug response varies between people. It’s not about weight. It’s not about age. It’s about your DNA.
What Drugs Are Most at Risk?
Not all drugs are equal. High-risk drugs have three things in common: they’re metabolized by CYP450, they have a narrow therapeutic window (small difference between effective and toxic dose), and they’re often taken long-term.
- CYP3A4 substrates: Simvastatin, cyclosporine, tacrolimus, fentanyl, midazolam, some calcium channel blockers
- CYP2D6 substrates: Metoprolol, codeine, tramadol, fluoxetine, paroxetine, tamoxifen
- CYP2C9 substrates: Warfarin, phenytoin, ibuprofen, losartan
- CYP2C19 substrates: Clopidogrel, omeprazole, citalopram
Strong inhibitors? Ketoconazole, clarithromycin, fluoxetine, fluvoxamine, grapefruit juice. Strong inducers? Rifampin, carbamazepine, phenytoin, St. John’s wort.
And here’s the kicker: 200 commonly prescribed drugs are sensitive to these interactions. The FDA tracks 27 that are most dangerous. But most doctors never check.
What Can You Do?
Don’t panic. But do be smart.
First, know your meds. Write them down. Include supplements. St. John’s wort isn’t harmless. Neither is goldenseal or green tea extract. They all interact.
Second, ask your pharmacist. Pharmacists are trained to spot these clashes. They use tools like Lexicomp, which catches 95% of major interactions. But only 42% of U.S. pharmacists check regularly - and only 28% of primary care doctors do.
Third, consider testing. Pharmacogenomic panels now cost $250-$500 and give results in 3-7 days. They test CYP2D6, CYP2C9, CYP2C19, CYP3A5, and more. Hospitals like Mayo Clinic and Cleveland Clinic now use them routinely. If you’re on five or more drugs, or have had an unexpected reaction, it’s worth it.
Fourth, use technology. Epic, Cerner, and Allscripts now push real-time alerts in electronic records. If your doctor prescribes a risky combo, the system should flag it. If it doesn’t, ask why.
The Bigger Picture
CYP450 interactions cause 30% of all adverse drug events. They’re behind 15-20% of hospitalizations in people taking five or more medications. That’s not a side note. That’s a public health crisis.
And it’s getting worse. The average Medicare patient takes 5.4 medications. That’s over 10 potential CYP450 clashes per person. Add in herbal products, OTC painkillers, and alcohol - and the risk multiplies.
But it’s fixable. Better labeling. Routine testing. Clinical decision tools. Pharmacist involvement. These aren’t futuristic ideas. They’re happening now. In 2023, 65% of U.S. hospitals have CYP450-based prescribing protocols. AI systems like IBM Watson are predicting interactions with 89% accuracy.
The future isn’t about avoiding drugs. It’s about matching the right drug to the right person. Your genes. Your meds. Your liver. It’s time we stopped treating everyone the same.
Can grapefruit juice really affect my medications?
Yes. Grapefruit juice blocks CYP3A4 in your gut, which means drugs like simvastatin, atorvastatin, felodipine, and some anti-anxiety meds build up to dangerous levels. Even one glass can raise drug concentrations by 30-80%. It’s not just a warning - it’s a medical risk. If you take any statin or blood pressure pill, check with your pharmacist before drinking grapefruit juice.
Why does my antidepressant make my blood pressure pill less effective?
It doesn’t make it less effective - it makes it more powerful. Many antidepressants like fluoxetine and paroxetine inhibit CYP2D6, the enzyme that breaks down beta-blockers like metoprolol. This causes metoprolol to build up in your blood, leading to slow heart rate, dizziness, or fainting. If you’re on both, your doctor should lower the metoprolol dose - or switch to a different antidepressant like sertraline, which has less impact on CYP2D6.
Is pharmacogenomic testing worth it?
If you’re on three or more medications, especially for heart, mental health, or pain, yes. If you’ve had side effects with no clear cause, yes. If you’re taking clopidogrel, codeine, or warfarin, definitely yes. Testing costs $250-$500 and can prevent hospitalization. Some insurers cover it if you’ve had a bad reaction. It’s not a luxury - it’s precision medicine.
Can herbal supplements really interfere with my prescriptions?
Absolutely. St. John’s wort induces CYP3A4 and P-glycoprotein, cutting levels of birth control, cyclosporine, and HIV meds by up to 60%. Goldenseal inhibits CYP3A4 and CYP2D6 - dangerous with opioids or antidepressants. Even green tea can inhibit CYP3A4. Most people think “natural” means safe. It doesn’t. Always tell your doctor what herbs or supplements you take.
Why do some drugs work for me but not my friend?
It’s likely your CYP450 genes. CYP2D6, CYP2C19, and CYP2C9 vary widely between people. One person might be a poor metabolizer - their body barely touches the drug. Another might be ultrarapid - they break it down too fast. That’s why two people on the same dose can have opposite results: one gets no relief, the other gets sick. Genetics explains why one-size-fits-all dosing often fails.
Most people think drug interactions are rare. They’re not. They’re the quiet, invisible cause of thousands of hospital visits every year. The good news? You don’t need to be a scientist to avoid them. Just know your meds. Ask questions. And don’t assume anything is harmless - especially if it’s labeled “natural.” Your liver is working hard. Don’t make it fight a war it didn’t sign up for.






14 Comments
Bro, I took simvastatin and grapefruit juice for a week thinking it was ‘natural detox’-ended up in the ER with muscle pain so bad I couldn’t lift my coffee cup. CYP3A4 don’t play. Never again. 🤡
This is why I always bring my med list to the pharmacy-no shame in asking. Pharmacists are the unsung heroes of safe prescribing. If you’re on five or more meds, you’re basically playing Russian roulette with your liver. Let’s normalize asking, ‘Hey, does this combo kill me?’
Stop taking supplements. They’re not ‘natural’-they’re unregulated poison. Your ‘herbal tea’ is killing you slowly. Get tested or shut up.
Interesting how the FDA tracks 27 ‘most dangerous’ interactions but doesn’t mandate pharmacogenomic screening. The system is designed to ignore biological individuality. We treat people like widgets, then wonder why 30% of hospitalizations are drug-related. The irony is delicious.
My grandma’s on 7 meds and still takes St. John’s wort ‘for her mood.’ I showed her this post. She said, ‘But it’s herbal!’ I just hugged her and called her pharmacist. We gotta protect our people.
Y’all act like this is new. I’ve been telling my patients since 2010 that fluoxetine + metoprolol = bradycardia city. Nobody listens. Doctors think ‘prescribing’ means ‘throwing pills at problems.’ It’s not medicine-it’s gambling with a loaded gun.
Okay so like… imagine your liver is this tiny, overworked barista at 3am, right? And every pill you take is some dude screaming ‘I NEED A LATTE WITH EXTRA ESPRESSO AND A CINNAMON STICK’ while also trying to steal your phone. And grapefruit juice? That’s the guy who pours gasoline in the espresso machine. And your genes? Some people’s liver is a Starbucks, some is a gas station with a Keurig. And nobody’s training the baristas. We’re all just… hoping the machine doesn’t explode. 🤯
My cousin took clopidogrel after her stent and had a clot two weeks later. Turns out she’s a poor CYP2C19 metabolizer. No one tested her. She almost died. This isn’t sci-fi-it’s Tuesday for a lot of us. Please, if you’re on meds, get the test. $500 is cheaper than a funeral.
My brain is a CYP450 enzyme and my meds are my exes… some I can handle, others? They just sit there blocking the whole damn pathway 😔💔. If you’re on SSRIs + statins + painkillers… you’re basically a walking pharmacokinetic disaster. But hey, at least your liver’s got a podcast.
U.S. healthcare is a scam. You pay $200 for a pill and $500 for a test that should’ve been done before you ever got the prescription. Meanwhile, Big Pharma profits off your liver failure. This isn’t medicine-it’s a revenue stream.
Pharmacogenomic testing isn’t ‘optional’-it’s essential. If you’re on warfarin, clopidogrel, codeine, or SSRIs, you’re already in the danger zone. Why are we still using ‘average dose’ protocols in 2025? This isn’t 1985. We have DNA. Use it. Please.
It’s fascinating how the CYP450 system operates as a biologically deterministic framework for therapeutic efficacy, yet the clinical paradigm remains stubbornly reductionist. The epistemological dissonance between molecular pharmacology and population-based prescribing is not merely an oversight-it’s a systemic failure of translational medicine.
Wait, so grapefruit juice is bad? Newsflash: water is bad too. Everything kills you. Chill.
Okay so I read this whole thing and I’m just… confused. Like, if CYP3A4 is the busiest intersection, why isn’t there a traffic light? Why aren’t we all wearing CYP450 helmets? And why does no one ever mention that your gut microbiome also messes with this stuff? Also, what if I just take my meds with orange juice? Is that safe? I mean, orange juice is like… less grapefruity? But still citrus? I think I need a flowchart. Or a therapist. Or both. 🤯
Write a comment