When your pharmacy hands you a pill that looks completely different from what you’ve been taking, it’s normal to feel uneasy. Maybe it’s a smaller white tablet instead of a large blue capsule. Maybe the name on the bottle is unfamiliar. You’re not alone. Millions of people switch from brand-name drugs to generics every year-mostly because it saves money. But what really happens when you make the switch? Is it safe? Will it still work? Here’s what you can actually expect.
Generics aren’t cheap knockoffs-they’re exact copies
The U.S. Food and Drug Administration (FDA) doesn’t allow just any drug to be sold as a generic. To get approval, a generic version must contain the same active ingredient, in the same strength, and work the same way in your body as the brand-name drug. That means if you’re taking lisinopril for high blood pressure, the generic version has the exact same chemical compound as Zestril. The FDA requires it to deliver the same amount of medicine into your bloodstream at the same rate-within a tight 80% to 125% range. This is called bioequivalence.
So why do generics cost so much less? Because the company making the generic didn’t spend millions developing the drug from scratch. The original brand-name maker paid for years of research, clinical trials, and marketing. Once the patent expires, other companies can make the same drug without those upfront costs. That’s why a 30-day supply of brand-name Lipitor might cost $300, while the generic atorvastatin costs $10.
You might notice a difference in how the pill looks
Trademark laws require generics to look different from the brand-name version. That means the color, shape, size, or even the imprint on the pill can change. A blue oval pill might become a white round one. That’s not a mistake-it’s the law. But it’s also one of the biggest reasons people get confused.
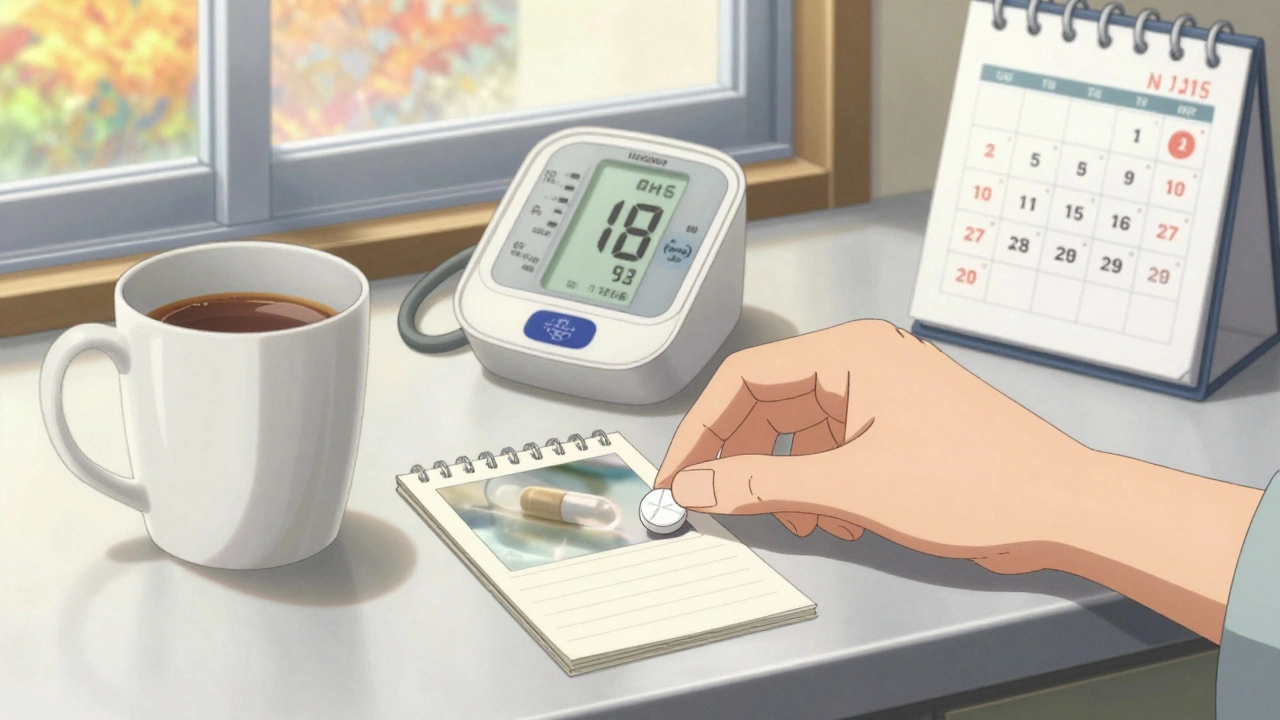
Some patients report feeling like the medicine isn’t working after switching, simply because the pill looks wrong. One woman in Cardiff told me she stopped taking her generic levothyroxine because it was a different shade of yellow than Synthroid. Her TSH levels were fine, but she didn’t trust it. After talking to her pharmacist, she learned the inactive ingredients (like dyes or fillers) were different, but the thyroid hormone was identical. She kept taking it-and her numbers stayed stable.
Pharmacies now often put stickers on bottles to warn you when the pill appearance changes. Some even include a small card explaining the difference. Don’t ignore these. If you’re unsure, ask your pharmacist. A quick check can prevent unnecessary worry-or worse, stopping your medication.
For most people, switching works just fine
Over 90% of all prescriptions filled in the U.S. are for generic drugs. That’s not because doctors are pushing them-it’s because patients and insurers want them. A 2019 report from the Association for Accessible Medicines found that people were 266% more likely to abandon a brand-name drug than a generic, mostly because of cost. Nearly 90% of generic copays are under $20. For brand-name drugs? Only 39% are.
Studies show that for conditions like high blood pressure, diabetes, high cholesterol, and depression, generics perform just as well. A 2022 review of 1,245 patient reviews on Drugs.com showed 78% rated generic medications as “good” or “excellent” for effectiveness. In Massachusetts, where law requires pharmacists to substitute generics unless the doctor says otherwise, 82% of patients reported satisfaction after three months-even though 63% were initially worried.
Bottom line: For most people, switching to a generic doesn’t change how the drug works. It just changes the price tag.
But for some drugs, switching can be risky
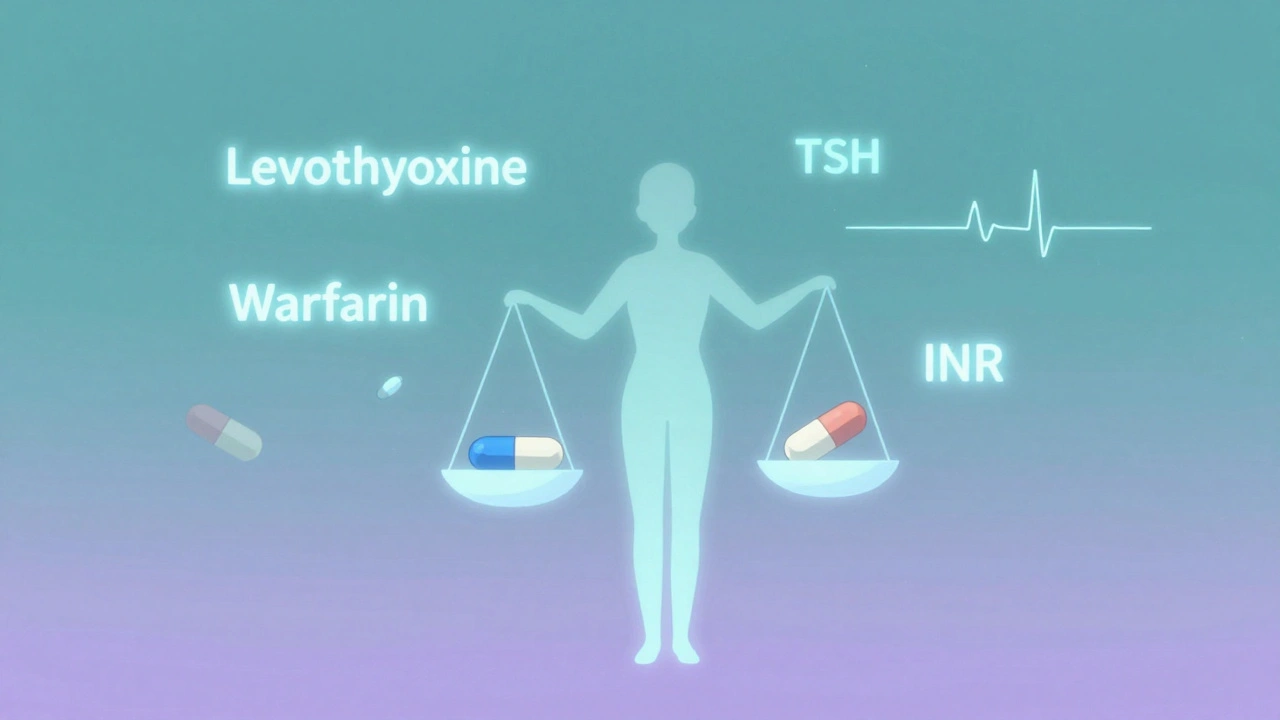
Not all medications are created equal when it comes to substitution. Some drugs have what’s called a “narrow therapeutic index”-meaning the difference between a dose that works and a dose that causes harm is very small. For these, even tiny changes in how the body absorbs the drug can matter.
Drugs in this category include:
- Levothyroxine (for hypothyroidism)
- Warfarin (a blood thinner)
- Phenytoin and other anti-seizure medications
- Lithium (for bipolar disorder)
- Cyclosporine (for organ transplants)
There are documented cases where patients switching from brand to generic levothyroxine saw their TSH levels jump from normal to dangerously high. One Reddit user shared: “Switched from Synthroid to generic. My TSH went from 2.5 to 8.7 in six weeks. I was exhausted, gained 15 pounds, and felt like I was drowning.” After switching back, her levels normalized.
That doesn’t mean generics are unsafe. It means that for these drugs, consistency matters. If you’ve been stable on a specific brand or even a specific generic manufacturer, switching to a different version-even another generic-can throw off your balance. That’s why some doctors write “dispense as written” or “no substitution” on prescriptions for these medications.
Why do generics switch manufacturers so often?
Here’s something most patients don’t realize: Your “generic” pill might come from a different company every time you refill. That’s because pharmacies buy from the cheapest supplier. In places like Saudi Arabia, government systems change generic suppliers every year based on bidding-over 25% of medications switched between brand and generic versions in just five years.
In the U.S., it’s less extreme but still common. You might get one generic this month, another next month. The active ingredient is the same, but the fillers, binders, or coatings can vary. For most people, that’s no problem. But for those with allergies or sensitivities, even small changes in inactive ingredients can cause stomach upset, rashes, or other reactions.
That’s why it’s important to know which generic manufacturer you’re on. If you notice new side effects after a refill, check the name on the bottle. Was it Teva last time and now it’s Mylan? Tell your doctor. You might need to stick with one manufacturer.
What you should do before and after switching
Switching doesn’t have to be scary. Here’s how to do it right:
- Ask your doctor if your medication is safe to switch. Especially if you’re on a narrow therapeutic index drug.
- Don’t assume all generics are the same. If you feel different after switching, note the manufacturer name and symptoms.
- Check your blood levels if you’re on thyroid, warfarin, or seizure meds. Your doctor may want to retest you 4-6 weeks after switching.
- Keep your pill bottle until you’re sure the new version works. The old one can help you compare size and color.
- Call your pharmacist if the pill looks different. They can tell you if it’s the same drug or a new generic.
And if you feel worse after switching? Don’t blame yourself. Don’t stop taking it. Call your doctor. Sometimes, going back to the brand-or sticking with one generic manufacturer-is the right move.
The big picture: Saving money without sacrificing care
Generic drugs save the U.S. healthcare system over $370 billion a year. That’s billions of dollars that go back into hospitals, clinics, and lower insurance premiums. Without generics, many people simply couldn’t afford their meds. A Harvard Health report found that high drug costs cause patients to skip doses, split pills, or go without treatment entirely.
But savings shouldn’t come at the cost of safety. The goal isn’t to force everyone onto the cheapest option. It’s to give people choices-with clear information. For most drugs, generics are just as good. For a few, they require extra care.
What matters most isn’t the brand on the bottle. It’s whether you’re taking your medicine consistently, feeling better, and staying healthy. If switching helps you do that? That’s a win.
Are generic drugs really as effective as brand-name drugs?
Yes, for most medications, generics are just as effective. The FDA requires them to have the same active ingredient, strength, dosage form, and bioequivalence as the brand-name version. Studies show that for conditions like high blood pressure, diabetes, and depression, generics perform equally well in real-world use. The main difference is cost-not effectiveness.
Why do generic pills look different from brand-name ones?
Trademark laws require generics to look different from brand-name drugs to avoid confusion. That means the color, shape, size, or imprint can change. But the active ingredient-the part that treats your condition-is identical. The differences are only in inactive ingredients like dyes or fillers, which don’t affect how the drug works.
Can switching to a generic cause side effects?
It’s rare, but possible. Some people are sensitive to inactive ingredients like dyes, preservatives, or fillers in generics. If you notice new side effects after switching-like stomach upset, rash, or dizziness-it could be due to these changes. Tell your doctor and pharmacist. You may need to switch back or stick with one manufacturer.
Which drugs should I avoid switching from brand to generic?
Avoid switching without medical advice if you’re taking drugs with a narrow therapeutic index-where small changes in blood levels can cause serious effects. These include levothyroxine (for thyroid), warfarin (blood thinner), phenytoin and other anti-seizure drugs, lithium, and cyclosporine. For these, consistency matters. Your doctor may need to write "dispense as written" on your prescription.
What should I do if I feel worse after switching to a generic?
Don’t stop taking the medication. Contact your doctor right away. Note the name of the generic manufacturer on the bottle and describe your symptoms. For certain drugs like thyroid or blood thinners, your doctor may order a blood test to check your levels. You may need to switch back to the brand or stick with the same generic manufacturer you were on before.
Why do pharmacies change generic manufacturers so often?
Pharmacies buy from the lowest-cost supplier to keep prices down. A generic drug can be made by several different companies, and the pharmacy switches based on which one offers the best price at the time. This can lead to changes in pill appearance or inactive ingredients, even if the active drug is the same. For most people, this isn’t a problem-but for those with sensitivities or on critical medications, it can cause issues.
Is it safe to use generics made outside the U.S.?
Yes. The FDA inspects all manufacturing facilities-whether in the U.S., India, China, or elsewhere-that supply drugs to American pharmacies. All generics sold in the U.S. must meet the same quality and safety standards as brand-name drugs. While some patients worry about overseas production, the FDA’s oversight ensures that the final product is safe and effective, regardless of where it’s made.
Final thought: Trust the science, not the label
The fear of generics often comes from misinformation or bad experiences with one specific switch. But the data is clear: for the vast majority of medications, generics work just as well. They’re not second-rate-they’re smart choices. The real issue isn’t whether generics work. It’s whether we’re paying attention to the people taking them.
If you’re on a drug where small changes matter, speak up. If you’re worried about a new pill, ask questions. If you feel different after switching, don’t ignore it. Your health isn’t about the brand on the bottle. It’s about the results you get-and the care you receive along the way.






11 Comments
Man, I switched my blood pressure med to generic last year and thought I was gonna die because it looked like a baby aspirin. Turns out I was fine. My BP’s actually better now. Guess I just needed to chill the hell out.
Pharmacists are the real MVPs here. Always ask ‘em.
I had this weird rash after switching my generic levothyroxine-turned out it was the dye in the new batch. My pharmacist said it was totally harmless but I was so scared I almost quit taking it. Thank god I called my doctor first.
Pro tip: Keep your old bottle until you’re sure the new one doesn’t mess you up. And if you’re on thyroid meds? Don’t switch manufacturers unless your doc says so. Tiny changes = big consequences.
Oh wow so generics are just as good? Shocking. I guess the pharma giants spent $10 billion on ads for nothing.
Meanwhile, people are still paying $300 for Lipitor like it’s a luxury handbag. I mean, come on. We’re not living in 2005. The FDA isn’t a joke. You’re just scared of white pills now? Grow up.
It is of paramount importance to recognize that the pharmacological equivalence of generic medications, as rigorously validated by the U.S. Food and Drug Administration, constitutes a cornerstone of accessible healthcare delivery in the modern era.
That being said, while the active pharmaceutical ingredient remains identical across brand and generic formulations, the excipient composition-though inert in most cases-may, in rare and clinically significant instances, precipitate idiosyncratic adverse reactions in susceptible individuals, particularly those with underlying hypersensitivities or metabolic variations.
Therefore, a nuanced, patient-centered approach to therapeutic substitution is not merely advisable-it is ethically imperative. One must not conflate cost-efficiency with clinical safety, especially in the context of narrow therapeutic index agents such as warfarin, lithium, and levothyroxine.
Moreover, the frequent rotation of generic manufacturers by retail pharmacies, while economically rational, introduces an element of unpredictability that may undermine therapeutic continuity. Documentation of the manufacturer name, and subsequent communication with prescribing providers, is not optional-it is a vital component of self-advocacy.
Let us not forget: the goal of healthcare is not merely to reduce expenditures, but to preserve and enhance patient well-being through informed, consistent, and compassionate care.
Bro, I’m from Nigeria and we don’t even have brand drugs most times. Everything is generic. My dad takes his blood pressure med for 10 years now-same generic, no problem. If you feel weird, check with doc. But don’t panic because pill color changed.
Money matters. You can’t eat if you skip medicine because it cost too much.
Oh so the FDA says it’s the same but my cousin’s TSH went to 12 after switching generics? Coincidence? Nah. I’m not buying it.
And yeah, sure, $10 vs $300-great. But what if your body says no? You think your insurance cares when you end up in the ER because your thyroid went haywire?
Save money? Sure. But don’t pretend it’s risk-free. People die from this shit.
There. Are. No. Exceptions. The FDA. Has. Standards. You. Are. Not. Special. If your body can’t handle a generic, you have a problem with your biology-not the system. Stop blaming the pill. Get your lab work done. Stop being dramatic.
Bro, you think you’re the only one who felt weird after switching? Everyone does. That’s why you check your levels. That’s why you talk to your pharmacist. That’s why you don’t just quit cold turkey because the pill looks different.
Stop being a baby. This isn’t a horror movie. It’s medicine. And if you’re too scared to take a white pill, maybe you shouldn’t be in charge of your own health.
I used to hate generics because they looked like candy. Then I realized I was judging a pill by its color. Funny how that works.
My mom’s on warfarin. We track her INR religiously after every switch. She’s fine. No drama. Just data.
It’s not about brand loyalty. It’s about paying attention. And honestly? If you’re taking meds regularly, you’re already doing better than most.
How quaint. You assume the FDA’s oversight is sufficient, yet you fail to acknowledge the geopolitical arbitrage that underpins generic manufacturing-India’s chemical factories, China’s regulatory gray zones, and the commodification of human biology as a cost-center.
One must ask: if bioequivalence is so absolute, why do physicians in academic centers still prescribe brand-name levothyroxine to critical patients? Because science is not a slogan. It is a practice-and practice demands consistency, not convenience.
Let us not mistake corporate efficiency for clinical wisdom.
My doctor told me to switch to generic statin. I did. Felt fine. No issues. But I kept the old bottle just in case. Smart move.
Don’t let anyone tell you you’re crazy for noticing the pill looks different. You’re not crazy. You’re observant. Just don’t panic. Talk to your pharmacist. They know more than you think.
Write a comment