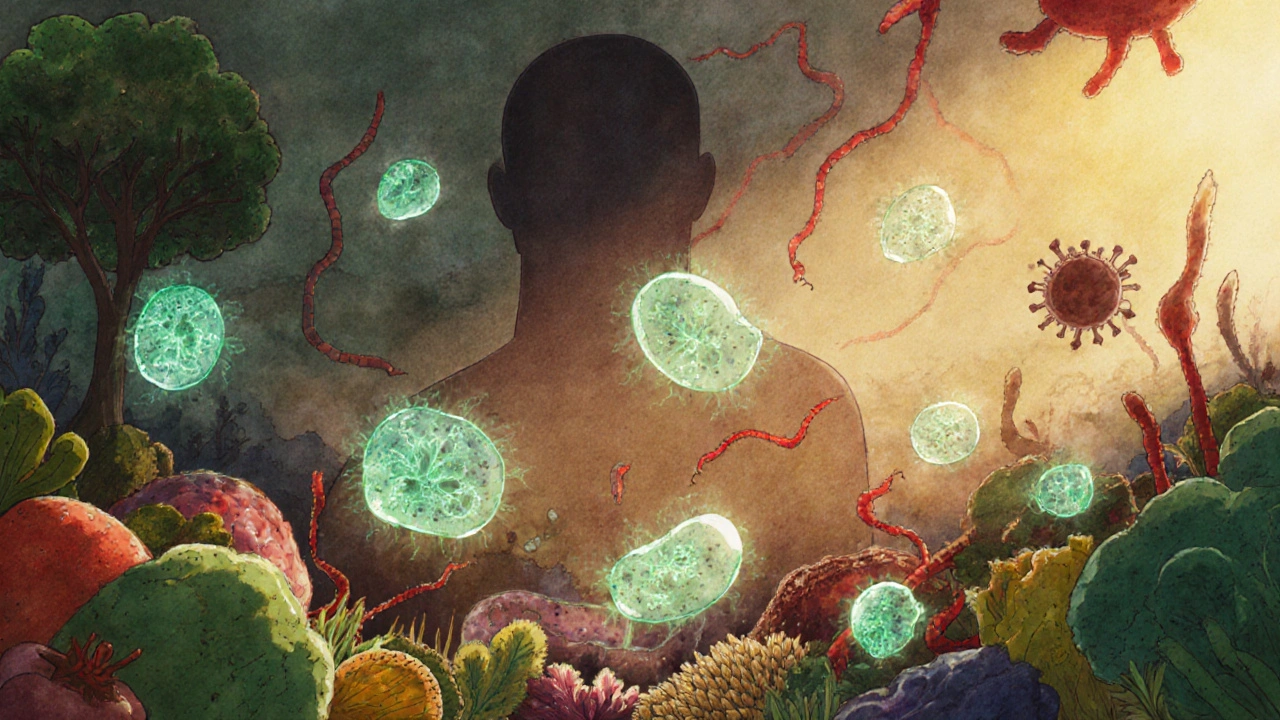
For decades, doctors treated autoimmune diseases like rheumatoid arthritis, lupus, and type 1 diabetes as problems inside the immune system alone. But now, researchers are looking lower-down into the gut. What’s growing in your intestines might be quietly triggering or worsening your autoimmune condition. This isn’t theory anymore. By 2025, over 150 clinical trials are actively testing treatments that target gut bacteria to calm down runaway immune responses. And the data is stacking up: people with autoimmune diseases consistently have different gut microbes than healthy individuals. Not just a little different-gut microbiome imbalances are now seen as a core part of how these diseases start and spread.
What’s Going On in Your Gut?
Your gut is home to trillions of bacteria, viruses, and fungi. Together, they form your microbiome-a living ecosystem that helps digest food, make vitamins, and train your immune system. In healthy people, this system stays balanced. But in autoimmune conditions, that balance breaks. Studies show people with rheumatoid arthritis, lupus, multiple sclerosis, and type 1 diabetes all share a common pattern: their gut microbes are less diverse. One 2025 meta-analysis of nearly 13,000 patients found a 23.7% drop in microbial diversity across all these conditions. That means fewer kinds of bacteria, and the ones that remain are often the wrong ones. Two bacterial groups stand out. Faecalibacterium prausnitzii, a friendly bacterium that reduces inflammation, is missing in up to 41% of patients with autoimmune diseases. Meanwhile, Ruminococcus gnavus, a troublemaker linked to inflammation, shows up 37.5% more often. This isn’t random. These microbes aren’t just passengers-they’re active players in immune dysfunction.How Gut Bacteria Trigger Autoimmunity
It’s not enough to say “bad bacteria cause disease.” Scientists have figured out how. One key mechanism is antigenic mimicry. Some gut bacteria have proteins that look a lot like your own tissues. When your immune system attacks those bacteria, it accidentally starts attacking your joints, pancreas, or nerves too. Another way is through immune cell manipulation. Researchers at Ohio State University found that a specific gut bacterium, segmented filamentous bacteria (SFB), can ramp up T follicular helper (Tfh) cells-cells that drive antibody production. In mice with arthritis and lupus, SFB exposure increased autoantibodies by 68%. That’s a direct link between one gut bug and a systemic autoimmune flare. Even more startling: some bacteria don’t stay in the gut. Yale researchers discovered that Enterococcus gallinarum can break through the intestinal wall, travel through the bloodstream, and reach the liver, spleen, and lymph nodes. In lupus patients, this bacterium was found in extraintestinal tissues in 63% of cases-compared to just 8% in healthy people. Once there, it triggers inflammation far from the gut. This isn’t just correlation. It’s a pathogen escaping its home and starting a fire elsewhere in the body.Differences Between Diseases
While many autoimmune diseases share similar gut imbalances, each has its own fingerprint. Type 1 diabetes patients have 32% fewer butyrate-producing bacteria than those with rheumatoid arthritis. Butyrate is a short-chain fatty acid that calms immune cells. Less of it means less control over inflammation. Multiple sclerosis patients show unique patterns too: their immune systems produce IgA antibodies that specifically stick to certain gut bacteria. That suggests the immune system is actively trying to contain them-but failing. And here’s the twist: not all probiotics help. Lactobacillus reuteri, often marketed as a “good” bacterium, made experimental autoimmune encephalomyelitis (a mouse model of MS) worse by 28% in a 2025 study. Other Lactobacillus strains, however, reduced inflammation. This shows you can’t treat all autoimmune diseases with the same probiotic. The microbiome is too complex for one-size-fits-all solutions.
What’s Being Done About It?
The medical world is racing to turn this science into treatments. Right now, there are 47 biotech companies working on microbiome-based therapies. Vedanta Biosciences and Seres Therapeutics lead the pack, with over 20 candidates in clinical trials. Three main approaches are being tested:- Probiotics: Live bacteria given to restore balance. Twenty-two specific strains are currently in trials for autoimmune conditions.
- Prebiotics: Food for good bacteria. Galactooligosaccharides, a type of prebiotic, boosted regulatory T cells by 34% in early rheumatoid arthritis trials.
- Targeted elimination: Killing the bad actors. Researchers are testing antibiotics or bacteriophages (viruses that eat bacteria) to wipe out Enterococcus gallinarum and other pathogenic strains without harming the rest of the microbiome.
Barriers to Real-World Use
Despite the promise, there are big roadblocks. First, testing is expensive. A full gut microbiome analysis via metagenomic sequencing costs between $1,200 and $3,500. That’s down 63% since 2020, but still out of reach for most. Second, it takes an average of 78 days to get a personalized profile back. Third, research methods are messy. A 2025 review found that 68% of studies use different stool collection methods, and only 12% track patients longer than six months. Without standardization, it’s hard to compare results or build reliable treatments. Also, not all clinics are ready. As of late 2024, only 38% of academic medical centers include gut microbiome testing in lupus care. For rheumatoid arthritis, it’s 22%. For MS, just 15%. That gap between research and practice is wide.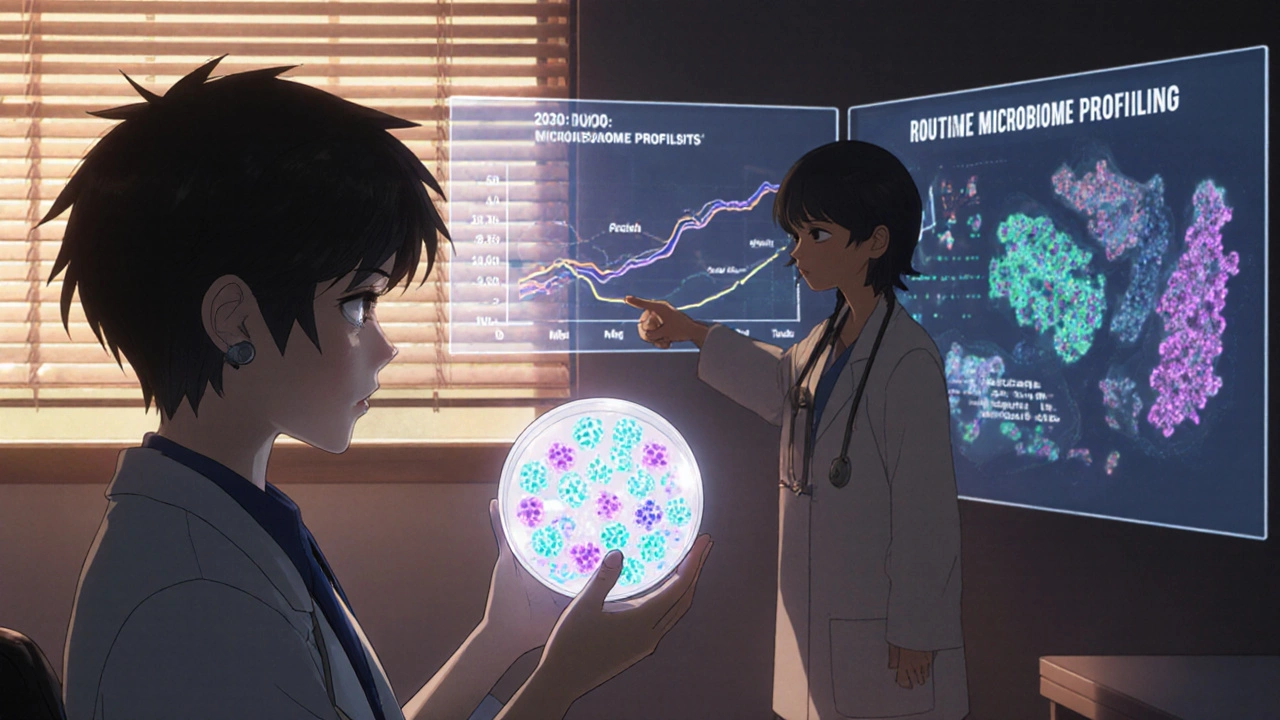
What’s Next?
The future is personal. By 2030, experts predict microbiome profiling will be as routine as blood tests for autoimmune patients. The NIH just launched a $18.7 million initiative to develop three microbiome-modulating therapies by 2028. The Lupus Research Alliance awarded $5.2 million in early 2025 specifically to study gut bacteria’s role in lupus. Global funding for this field hit $847 million in 2024-up 22% from the year before. What’s clear is this: the gut isn’t just a digestive organ. It’s an immune command center. And if you have an autoimmune disease, your gut bacteria might be sending the wrong signals. The next wave of treatment won’t just suppress your immune system. It will retrain it-starting in your intestines.What You Can Do Today
You don’t need to wait for a clinical trial to support your gut health. While no specific diet is proven to cure autoimmune disease, evidence suggests these steps help:- Eat more fiber-especially from vegetables, legumes, and whole grains. Fiber feeds good bacteria and boosts butyrate production.
- Limit ultra-processed foods. They reduce microbial diversity and promote inflammation.
- Consider fermented foods like unsweetened yogurt, kefir, sauerkraut, and kimchi. They introduce live microbes that may help balance your gut.
- Avoid unnecessary antibiotics. They wipe out good bacteria along with bad ones.
- Manage stress. Chronic stress changes gut permeability and alters microbial composition.





8 Comments
The data presented here is methodologically sound, with robust meta-analytic support for reduced microbial diversity across autoimmune cohorts. However, the causal inference remains tenuous without longitudinal, fecal-microbiota-transplant-controlled trials. The reliance on cross-sectional stool analyses introduces significant confounding from dietary, pharmacological, and environmental variables. Until standardization protocols are enforced, clinical translation remains premature.
OMG this is SO cool!! 🌱🤯 I just started eating more kimchi and fiber and my joint pain has already improved!! My gut is finally chillin’ 😌💪 Let’s all feed our bacteria like they’re tiny little pets!!
One must question, the extent to which the microbiome is truly causal-or merely correlative-given the absence of mechanistic specificity across heterogeneous disease phenotypes. The authors, in their enthusiasm, conflate association with pathogenesis. Moreover, the suggestion that probiotics are universally beneficial? Absurd. Lactobacillus reuteri exacerbates EAE? Clearly, the literature is fragmented, and therapeutic extrapolation is reckless.
It is profoundly disturbing that, despite compelling evidence linking gut dysbiosis to systemic autoimmunity, clinical adoption remains abysmally low. This is not merely a scientific gap-it is a systemic failure of medical institutions to prioritize root-cause medicine over symptomatic suppression. Patients are being failed. The data is unequivocal. Why are we still treating the immune system as if it exists in a vacuum?
i just read this and my brain is blown away!! 🤯 so if my gut is unhappy, my body is attacking me?? that makes so much sense!! i’m gonna eat more veggies and stop eating that junk food!! 🥦✨
Man, I’ve been doing the fermented foods thing for months and I swear I feel way better. Not cured, but way less bloated and less brain fog. Didn’t even know the science behind it until now. Thanks for laying it out like this.
They’re hiding the truth. This isn’t about bacteria-it’s about Big Pharma’s control over immune drugs. Why would they let you fix your gut when they make billions suppressing your immune system with toxic drugs? 63% of lupus patients have Enterococcus in their organs? Coincidence? Or is this a cover-up? The FDA won’t approve natural fixes because they can’t patent them. Wake up.
How quaint. Western medicine finally caught up to Ayurveda and Traditional Chinese Medicine, which have understood gut-immune links for millennia. Yet we’re still paying $3,500 for a stool test? In India, we’ve been using turmeric, triphala, and fasting for this since before your ancestors invented the wheel. All this ‘research’ is just repackaging ancient wisdom with a Western price tag.
Write a comment