Temovate Alternatives Guide
Find the best alternative to Temovate for your skin condition
Select your situation to get personalized recommendations based on medical guidelines and patient experience.
Your Recommended Treatment Options
Risk Level:
Cost Estimate:
Temovate (clobetasol propionate) is one of the strongest topical steroids doctors prescribe for stubborn skin conditions like psoriasis, eczema, and severe dermatitis. It works fast - often clearing flare-ups in under a week. But it’s not the only option. And for many people, it’s not the best long-term choice. If you’ve been using Temovate and are wondering if there’s something safer, cheaper, or more sustainable, you’re not alone.
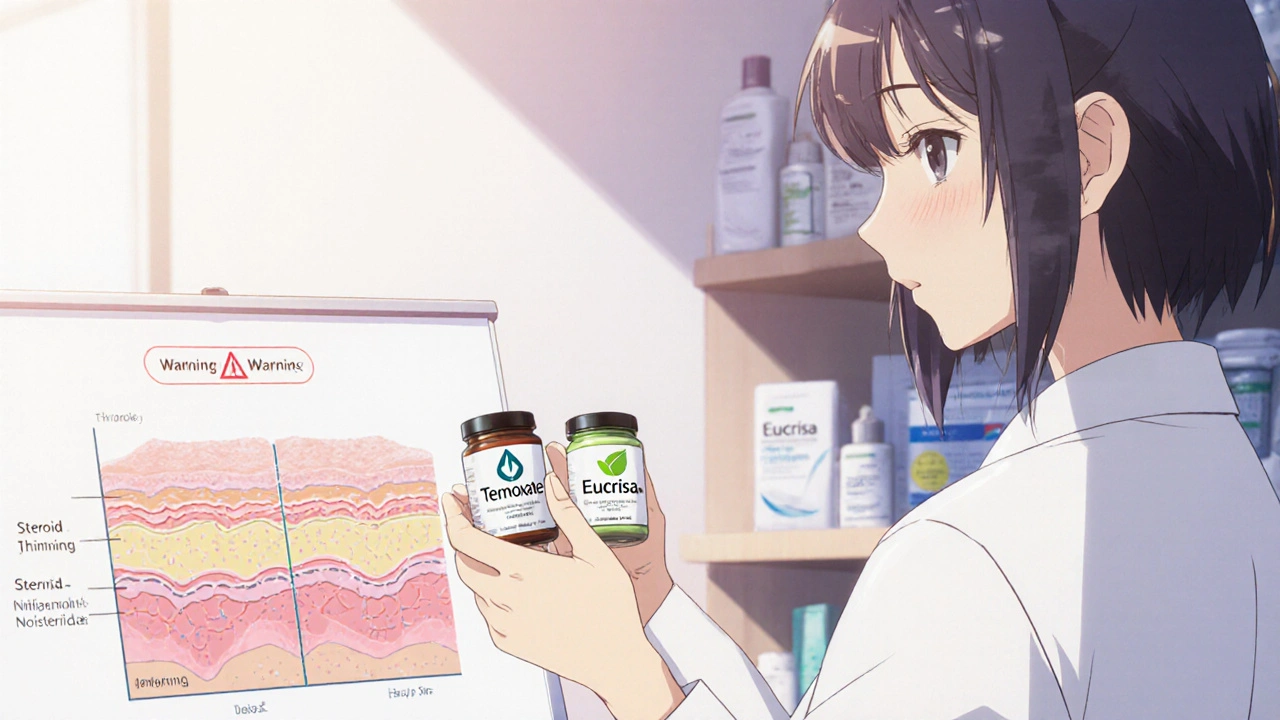
What Temovate Actually Does
Temovate contains clobetasol propionate, a class I corticosteroid - the strongest category approved for topical use in the U.S. It suppresses inflammation by calming overactive immune cells in the skin. That’s why it works so well for thick, scaly patches of psoriasis or red, itchy eczema that won’t quit.
But strength comes with risks. Using Temovate for more than two weeks straight can thin your skin, cause stretch marks, or even trigger rebound flare-ups when you stop. The FDA warns against using it on the face, groin, or underarms unless specifically directed. And children under 12 shouldn’t use it at all.
Why People Look for Alternatives
Most people don’t start looking for alternatives because Temovate doesn’t work. They look because:
- They’ve been using it for months and are scared of side effects
- Their insurance won’t cover it anymore
- They’re pregnant or nursing and need something safer
- They’re tired of applying a steroid every day
- They’ve had a flare-up return worse after stopping
These aren’t rare concerns. A 2023 study in the Journal of the American Academy of Dermatology found that nearly 40% of patients using high-potency steroids like clobetasol for more than 4 weeks reported skin thinning or other adverse effects.
Top Alternatives to Temovate
There are three main categories of alternatives: other steroids, non-steroidal options, and newer targeted therapies. Here’s how they stack up.
1. Other Topical Steroids (Milder Versions)
You don’t always need the strongest option. Many people do just fine with mid-potency steroids like:
- Triamcinolone acetonide (Kenalog) - Class III, good for face and sensitive areas
- Mometasone furoate (Elocon) - Class II, less skin thinning risk
- Fluticasone propionate (Cutivate) - Class II, often used for eczema in kids
These work slower than Temovate - maybe 10 to 14 days to see results - but they’re much safer for longer use. Dermatologists often recommend stepping down from Temovate to one of these after the first flare-up clears.
2. Non-Steroidal Topicals
These don’t contain steroids at all. They’re great for maintenance or when you need to avoid corticosteroids entirely.
- Calcineurin inhibitors - Tacrolimus (Protopic) and Pimecrolimus (Elidel). They block immune signals that cause inflammation. Safe for face and eyelids. Can cause temporary burning when first applied. Not for children under 2.
- PDE4 inhibitors - Crisaborole (Eucrisa). A non-steroidal ointment for mild-to-moderate eczema. Works over weeks, not days. No skin thinning. Safe for kids 3 months and older.
- Tapinarof (Vtama). A newer topical approved in 2022 for plaque psoriasis. Works by activating the aryl hydrocarbon receptor, which calms skin inflammation. Applied once daily. No steroid side effects. Works well for long-term use.
These are often more expensive than steroids, but if you’re using Temovate daily for months, the cost of side effects - both physical and financial - can add up faster.
3. Biologics and Systemic Treatments
If topical treatments aren’t cutting it, you might need something that works from inside your body.
- Biologics - Dupilumab (Dupixent), Tralokinumab (Adbry), Guselkumab (Tremfya). Injected monthly or every few weeks. Target specific immune proteins. Highly effective for moderate-to-severe psoriasis and eczema. Not for mild cases.
- Oral medications - Methotrexate, Cyclosporine, Apremilast (Otezla). Used when skin covers more than 10% of your body. Require regular blood tests.
These aren’t replacements for Temovate - they’re for when Temovate isn’t enough. But they’re becoming the new standard for chronic conditions.
Comparison Table: Temovate vs Alternatives
| Product | Type | Potency | Best For | Time to Work | Long-Term Safety | Cost (Monthly Estimate) |
|---|---|---|---|---|---|---|
| Temovate (Clobetasol) | Topical Steroid | Class I (Highest) | Severe psoriasis, thick plaques | 3-7 days | Poor - skin thinning, rebound | $40-$80 |
| Triamcinolone | Topical Steroid | Class III | Moderate eczema, face, folds | 7-14 days | Good - safer for extended use | $15-$30 |
| Protopic (Tacrolimus) | Non-Steroidal | N/A | Face, eyelids, sensitive skin | 1-4 weeks | Excellent - no thinning | $200-$300 |
| Eucrisa (Crisaborole) | Non-Steroidal | N/A | Mild eczema, children | 2-6 weeks | Excellent - safe for long-term | $150-$250 |
| Vtama (Tapinarof) | Non-Steroidal | N/A | Plaque psoriasis | 2-8 weeks | Excellent - no steroid risks | $1,000+ |
| Dupixent (Dupilumab) | Biologic | N/A | Severe eczema, psoriasis | 2-16 weeks | Good - requires monitoring | $3,000-$5,000 |
When to Stick With Temovate
Temovate still has a place. If you have:
- Thick, stubborn plaques of psoriasis that haven’t budged with anything else
- A sudden, severe flare-up that needs rapid control
- Been cleared by your doctor for short-term use (2-4 weeks max)
Then it’s still one of the most effective tools you have. The key is using it like a fire extinguisher - not a humidifier.
When to Switch
Consider switching if:
- You’ve used Temovate for more than 2 weeks straight
- Your skin looks shiny, stretched, or feels paper-thin
- You’re applying it to your face, neck, or genitals
- You’ve had three or more flare-ups in a year
- Your insurance now requires a prior authorization
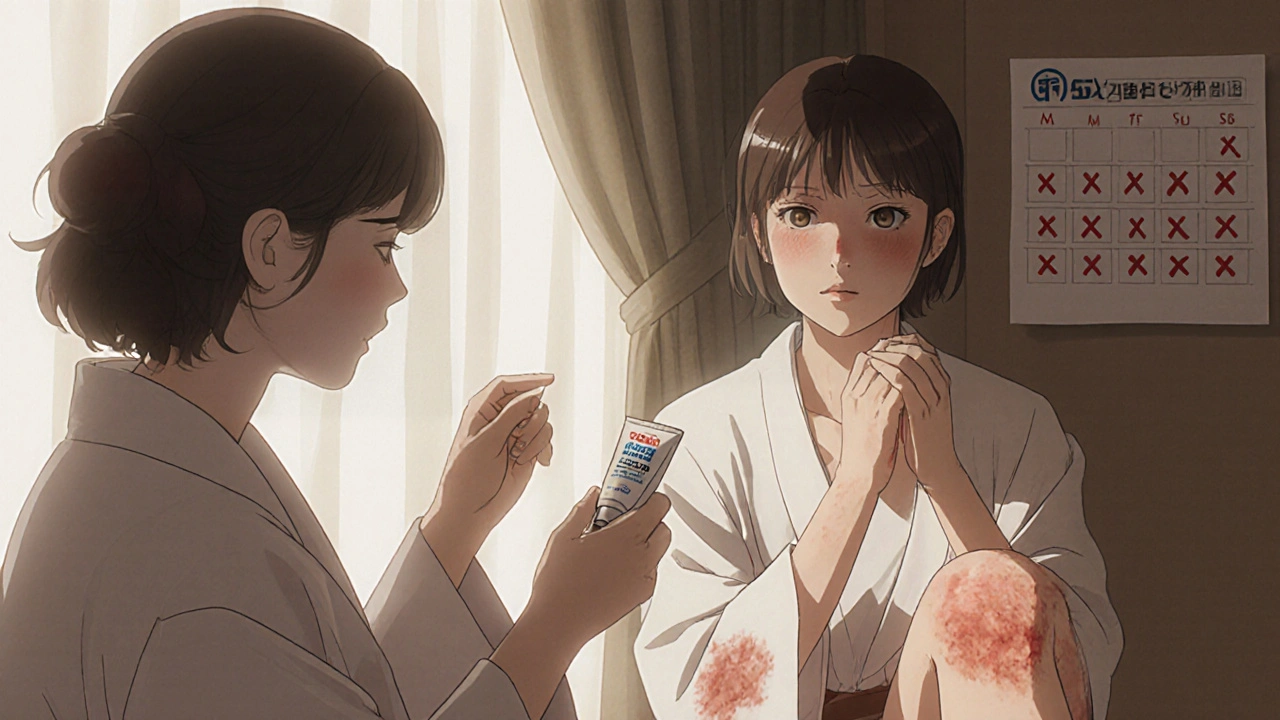
Switching doesn’t mean giving up. It means switching strategies. Most dermatologists use a “steroid ladder” - start high, step down, then move to non-steroidal maintenance.
What to Ask Your Doctor
Don’t stop Temovate cold turkey. That can cause a nasty rebound. Instead, ask:
- “Can we try stepping down to a lower steroid first?”
- “Is a non-steroidal option like Eucrisa or Vtama right for me?”
- “Do I need to test for fungal infections? Steroids can hide them.”
- “Should I be using a moisturizer with ceramides alongside this?”
- “Is there a maintenance plan to prevent the next flare-up?”
Good doctors don’t just prescribe - they plan. If your provider doesn’t talk about long-term strategy, it’s time to ask for a second opinion.
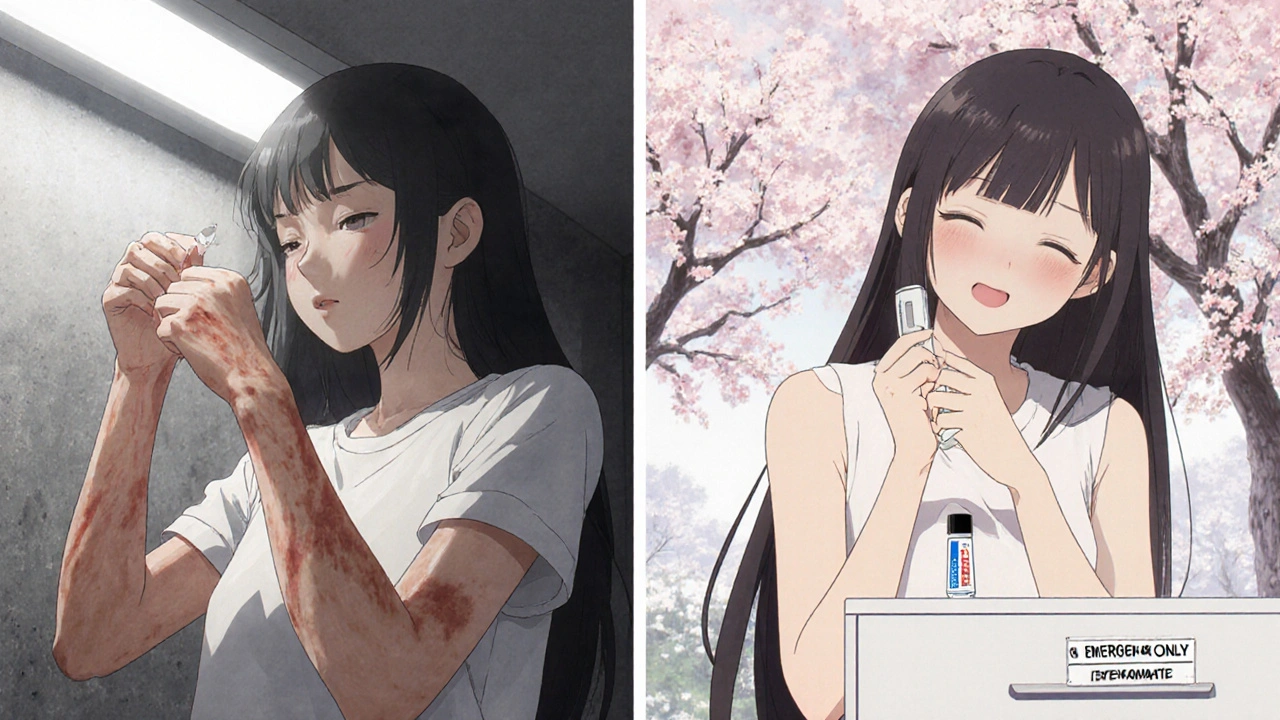
Real-Life Example: Sarah’s Story
Sarah, 34, had psoriasis on her elbows and knees for 8 years. She used Temovate every day for 11 months. Her skin cleared - but her arms got thin, shiny, and bruised easily. When she stopped, her psoriasis came back worse.
Her dermatologist switched her to a twice-weekly regimen of triamcinolone, added Eucrisa on flare spots, and started her on a ceramide-rich moisturizer. After three months, her skin was healthier than it had been in years. She still uses Temovate - but only once every few months, for 5 days at a time.
She didn’t cure her psoriasis. But she took back control.
Bottom Line
Temovate is powerful - but it’s not a lifelong solution. The best outcomes come from using it briefly to calm a flare, then switching to gentler, safer options for daily care. There’s no shame in needing a strong steroid to get started. But staying on it too long? That’s where things go wrong.
Work with your doctor to build a plan that gets you clear fast - and keeps you clear without damaging your skin. You don’t have to choose between relief and safety. There’s a middle path.
Is Temovate stronger than hydrocortisone?
Yes, Temovate is much stronger. Hydrocortisone is a Class VII steroid - the weakest available over the counter. Temovate is Class I - the strongest prescription steroid. Temovate works about 100 times more powerfully than hydrocortisone. Don’t swap them without medical advice.
Can I use Temovate on my face?
Only if your doctor specifically says so - and even then, for no more than 5 days. The skin on your face is thin and sensitive. Using Temovate there can cause acne, redness, or permanent damage like skin atrophy. Safer options like tacrolimus or low-dose steroids are preferred for facial skin.
How long does clobetasol stay in your system?
Topical clobetasol doesn’t stay in your bloodstream long - most of it stays on the skin. But if you use too much or for too long, some can be absorbed. It takes about 24-48 hours for your body to clear the absorbed amount. The real concern isn’t systemic buildup - it’s local damage to your skin.
Are there natural alternatives to Temovate?
Some people try coconut oil, aloe vera, or oatmeal baths to soothe skin. These can help with itching and dryness, but they don’t reduce inflammation like a steroid or PDE4 inhibitor. They’re supportive, not replacements. Don’t use them instead of prescribed medication for active psoriasis or eczema.
What’s the cheapest alternative to Temovate?
Triamcinolone acetonide (Kenalog) is often the most affordable prescription alternative, costing as little as $15 per tube with insurance. Over-the-counter hydrocortisone 1% is cheaper still - but far less effective for severe cases. For long-term use, Eucrisa or moisturizers with ceramides may save money by preventing flare-ups.
Can Temovate cause weight gain or mood changes?
Rarely. Systemic absorption from topical use is minimal. Weight gain or mood swings are more common with oral steroids or long-term injections. With Temovate, the main risks are skin thinning, stretch marks, and rebound flares - not internal side effects.
How do I know if I’m using too much Temovate?
Signs you’re overusing it: skin looks shiny or translucent, you get stretch marks, the area feels fragile or bruises easily, your flare comes back worse after stopping, or you’re applying it to large areas (like more than 10% of your body). If any of this sounds familiar, talk to your doctor about stepping down.






10 Comments
I used Temovate for six months straight because my psoriasis was out of control. Skin started looking like tissue paper. When I finally stopped, the rebound was brutal. Switched to Eucrisa and triamcinolone twice a week-slower, yeah, but my skin’s actually healing now. No more shiny arms, no more bruising. Worth the wait.
just wanted to say eczema warriors unite!! i tried protopic and it burned like hell at first but after 3 days? holy crap it was magic. my face stopped looking like a tomato. no more steroid fear. also, moisturizer with ceramides is non-negotiable. i use ceraVe like its water.
Let me break this down for you because the medical industry doesn’t want you to know this: clobetasol is a controlled substance disguised as a cream. They push it because it’s profitable. The FDA knows the long-term damage. They just don’t care. Biologics? 5k a month? That’s not medicine, that’s a ransom. They want you addicted to the cream so you keep coming back for the next one. And don’t get me started on how they market Eucrisa as ‘safe’-it’s just the new placebo with a fancy name. The real cure? Diet. Gluten. Dairy. Stress. Nobody talks about that because Big Pharma doesn’t sell kale.
Temovate is like using a flamethrower to light a candle. It works, sure, but you’re gonna burn down the whole damn house. I went from daily use to twice a week with triamcinolone and now I keep Vtama in my medicine cabinet like a secret weapon. Only pull it out when the demons come back. Skin’s thicker now. Less red. Less scared. Also, oatmeal baths are underrated. Like a warm hug for your epidermis.
so i started using eucrisa after my derm told me to stop temovate and honestly i think i messed up the applicator? it felt weird and i didnt see results for like 3 weeks and i was about to quit but then one morning i woke up and my elbow looked normal?? like, actual normal skin. i think i just needed to be patient. also i use aquaphor now and its a game changer.
Let’s be candid. The entire dermatological paradigm is a neoliberal construct designed to pathologize normal epidermal variability. Clobetasol propionate, as a class I glucocorticoid, induces glucocorticoid receptor-mediated transcriptional suppression of NF-kB and AP-1 pathways-yet the clinical literature systematically underreports off-target mitochondrial dysfunction. You’re being monetized through iatrogenic dependency. The so-called ‘non-steroidal alternatives’ are merely pharmacoeconomic placeholders. Real intervention requires microbiome modulation via fecal transplant protocols, which are currently suppressed due to regulatory capture by pharmaceutical oligopolies.
OMG I JUST FOUND OUT MY DERMATOLOGIST GAVE ME TEMOVATE FOR 18 MONTHS AND DIDN’T EVEN TELL ME THE RISKS?? I’M CRYING RIGHT NOW. MY FACE IS SHRINKING. I’M GOING TO POST A VIDEO ON TIKTOK ABOUT THIS. MY MOM IS FREAKING OUT. I NEED A LAWYER. WHO DO I SUE??
Hey everyone, I just want to say how proud I am of all of you for being here, learning, and making these tough decisions for your skin. This is real life stuff. I’ve been managing psoriasis since I was 16, and I’ve tried everything-steroids, biologics, light therapy, even acupuncture. The key isn’t finding the perfect cream. It’s finding the right rhythm. Step down. Stay consistent. Listen to your body. And if your doctor doesn’t talk to you like a partner, find one who does. You’re not alone in this. We’re all just trying to get back to feeling like ourselves again. And hey-if you’re reading this and feeling overwhelmed? Breathe. You’ve got this. One day, one application, one moisturizer at a time.
This post is an egregious example of medical misinformation masquerading as patient advocacy. The assertion that ‘stepping down’ from a Class I steroid is universally advisable lacks robust longitudinal evidence. Furthermore, the inclusion of cost data without accounting for insurance tiering, prior authorization delays, and copay assistance programs is economically irresponsible. The recommendation to use Eucrisa for ‘mild eczema’ is clinically inappropriate for patients with moderate-to-severe disease. The author exhibits a dangerous conflation of anecdotal experience with evidence-based practice. I am astonished that this content has not been flagged for regulatory review.
Thank you for sharing this thoughtful overview. I’ve been using tacrolimus for my facial eczema for two years now, and while the initial burning was uncomfortable, the long-term outcome has been far better than any steroid I’ve used. I agree that the ‘steroid ladder’ approach is wise. For those considering alternatives, I’d also suggest discussing phototherapy with your dermatologist-it’s underused, often covered by insurance, and very effective for maintenance. Patience and consistency matter more than speed.
Write a comment