Transient Ischemic Attack is a brief, reversible episode of neurological dysfunction caused by temporary loss of blood flow to the brain. It’s often called a "mini‑stroke" because the symptoms mimic a stroke but resolve within minutes to hours. When someone you love experiences a TIA, the shock can feel like a full‑blown stroke. The good news? Early action and solid support can dramatically lower the risk of a future stroke and speed up recovery.
Quick Take (TL;DR)
- Call emergency services immediately; a TIA is a medical emergency.
- Schedule a follow‑up with a Neurologist brain‑health specialist who evaluates stroke risk and tailors treatment within 48hours.
- Help your loved one manage Medication prescribed drugs such as antiplatelets, antihypertensives, or statins and track side‑effects.
- Encourage lifestyle shifts: quit smoking, adopt a Mediterranean diet, and get regular exercise.
- Provide emotional backing and connect with a Support group community of TIA/stroke survivors and caregivers for shared experiences.
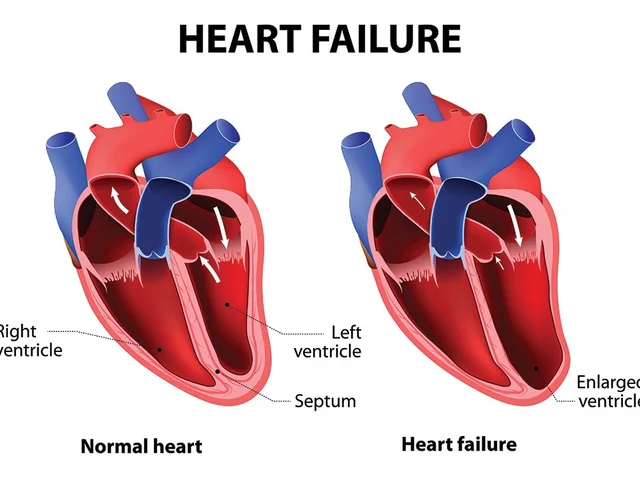
What Exactly Is a TIA?
Think of the brain as a city powered by a network of roads (arteries). A TIA is a temporary traffic jam-blood can’t reach a part of the brain long enough to cause permanent damage, but the traffic slowdown produces classic stroke symptoms: sudden weakness, slurred speech, vision changes, or confusion.
Because the symptoms fade quickly, many people dismiss them. However, a TIA is a major warning sign. Studies from the American Heart Association show that up to 1 in 3 people who have a TIA will suffer a full stroke within a year if risk factors aren’t addressed.
How a TIA Differs from a Stroke
| Aspect | Transient Ischemic Attack | Stroke |
|---|---|---|
| Duration of symptoms | Minutes to 24hours | Persist beyond 24hours |
| Brain damage | None (reversible) | Permanent injury |
| Immediate risk | High risk of future stroke | Immediate life‑threatening event |
| Treatment focus | Risk‑factor control, medication | Acute interventions (tPA, thrombectomy) |
Understanding these distinctions helps you explain the situation to your loved one without causing unnecessary panic.
First‑Hour Action Plan
- Call emergency services (999 in the UK). A TIA qualifies as a medical emergency even if symptoms vanish.
- Stay with the person until help arrives. Note the exact time symptoms began and what they were (e.g., “right‑hand weakness at 10:12am”).
- Do not give food, drink, or medication unless instructed by a professional.
- After hospital admission, ask for a copy of the discharge summary; it will list the Risk factor modifiable elements such as high blood pressure, atrial fibrillation, or high cholesterol that need addressing.
The Role of the Caregiver family member or friend who assists the patient with daily tasks and medical management
Being a caregiver isn’t a full‑time job title; it’s a set of habits you adopt to keep the recovery on track. Your core responsibilities fall into three buckets: medical coordination, lifestyle support, and emotional nurturing.
- Medical coordination: Schedule follow‑ups, manage Medication refills, and keep a symptom diary.
- Lifestyle support: Help plan heart‑healthy meals, join walking sessions, and eliminate smoking triggers.
- Emotional nurturing: Listen without judgment, encourage questions, and watch for signs of anxiety or depression.
When you feel overwhelmed, remember that you’re not alone-most caregivers report feeling “supported” when they have clear checklists and a reliable point of contact, like the patient’s neurologist.
Medical Management: Medications and Appointments
After a TIA, doctors typically prescribe a cocktail of medicines aimed at preventing clot formation and controlling blood pressure. Common classes include:
- Antiplatelet agents (e.g., aspirin, clopidogrel) - thin the blood.
- Statins (e.g., atorvastatin) - lower cholesterol.
- Antihypertensives (e.g., lisinopril) - keep blood pressure in check.
Set up a medication calendar (paper or app) and cross‑check each dose daily. If side‑effects appear-muscle pain from statins, bruising from antiplatelets-call the Neurologist promptly.
Schedule the first post‑TIA appointment within 48hours. During that visit, request a clear plan that outlines:
- Target blood‑pressure range.
- Desired cholesterol levels.
- Recommended physical‑activity goals.
- Any additional testing (e.g., carotid ultrasound).
Write down the plan, and keep it on the fridge where everyone can see it.

Rehabilitation: Physical Therapy and Beyond
Even when symptoms resolve, the brain benefits from structured rehabilitation. Physical therapy targeted exercises that improve strength, balance, and cardiovascular fitness helps re‑establish blood‑flow patterns and reduces future stroke risk.
Typical PT regimens after a TIA include:
- Low‑impact cardio (e.g., stationary bike, brisk walking) for 20‑30minutes, three times a week.
- Balance drills - heel‑to‑toe walks, single‑leg stands.
- Strength training - light resistance bands focusing on the lower body.
Coordinate with the therapist to set realistic milestones, such as “walk 1km without stopping by week 4.” Celebrate each win; small achievements reinforce adherence.
Connecting with a Support group
Emotional recovery is often overlooked. A TIA can trigger fear of another event, leading to anxiety or even depression. Joining a support group-whether in‑person at a local hospital or online via national stroke charities-offers three benefits:
- Peers share practical tips (e.g., best blood‑pressure cuffs for home use).
- Storytelling normalises fears, reducing isolation.
- Groups often host expert Q&A sessions with neurologists and physiotherapists.
Encourage your loved one to attend at least one meeting per month and sit with them if they feel nervous about new faces.
Lifestyle Adjustments that Make a Difference
Research from the British Heart Foundation indicates that lifestyle changes can cut stroke risk by up to 80%. Here’s a checklist you can implement together:
- Diet: Adopt a Mediterranean‑style menu-lots of leafy greens, fish, olive oil, and nuts. Limit processed foods and sugary drinks.
- Exercise: Aim for 150minutes of moderate activity weekly; use a shared calendar to track progress.
- Smoking: If they smoke, explore nicotine‑replacement therapy or local cessation programs.
- Alcohol: Keep consumption under 14units per week for men, 7 for women.
- Stress management: Try mindfulness apps, short walks in nature, or gardening.
Put the plan on the fridge next to the medication calendar-visual reminders work wonders.
Monitoring Progress and Spotting Red Flags
During the first three months, keep a log that captures:
- Date and time of each medication dose.
- Blood‑pressure readings (morning and evening).
- Any new or recurring symptoms (e.g., dizziness, headaches).
- Exercise duration and perceived effort.
If you notice any of the following, call the neurologist or go to the emergency department:
- Sudden weakness or numbness on one side.
- Speech that becomes slurred or garbled.
- Severe, sudden headache with no known cause.
- Chest pain or shortness of breath (possible cardiac event).
Caregiver Self‑Care: You Can’t Pour From an Empty Cup
Research in the Journal of Stroke & Cerebrovascular Diseases shows that caregivers who schedule regular breaks have better patient outcomes. Here are quick ways to recharge:
- Set a daily 15‑minute “quiet time” - no phone, no chores.
- Swap duties with another family member once a week.
- Join a caregiver‑specific support group; they focus on burnout prevention.
- Maintain your own medical appointments - you’re part of the care team too.
When you’re rested, you’ll notice you’re more patient, more organized, and better at spotting red flags.
Quick Checklist for New Caregivers
- Call 999 at the first sign of a TIA.
- Secure a follow‑up with a neurologist within 48hours.
- Create a medication calendar and log blood pressure daily.
- Schedule physical‑therapy sessions and set weekly activity goals.
- Find a local or online support group and attend at least once a month.
- Implement a heart‑healthy diet and smoking cessation plan.
- Track symptoms, meds, BP, and exercise in a shared notebook.
- Plan regular caregiver “reset” moments to avoid burnout.
Frequently Asked Questions
What is the difference between a TIA and a full stroke?
A TIA causes temporary neurological symptoms that resolve within 24hours and leaves no permanent brain damage, while a stroke results in lasting injury and symptoms that persist beyond 24hours. Both demand urgent medical attention, but a TIA is a warning sign that a stroke may follow if risk factors aren’t addressed.
How soon should I see a neurologist after a TIA?
Ideally within 48hours of the event. Early evaluation allows the doctor to prescribe antiplatelet medication, assess blood pressure and cholesterol, and order imaging to pinpoint the cause.
What medications are commonly prescribed after a TIA?
Typical prescriptions include antiplatelet agents (aspirin or clopidogrel), statins to lower cholesterol, and antihypertensives to control blood pressure. The exact combo depends on personal risk factors such as diabetes, atrial fibrillation, or prior heart disease.
Can lifestyle changes really lower my loved one’s stroke risk?
Yes. Studies show that quitting smoking, adopting a Mediterranean diet, exercising regularly, and maintaining blood pressure below 130/80mmHg can cut the risk of a subsequent stroke by up to 80%.
How can I support my loved one emotionally after a TIA?
Listen without minimizing their fears, encourage questions, and help them join a support group. Validate their feelings and keep communication open. If anxiety or depression seem to develop, suggest a referral to a mental‑health professional.
What red‑flag symptoms mean I should call 999 again?
Sudden weakness or numbness on one side, slurred speech, severe headache, vision loss, or chest pain/difficulty breathing all require immediate emergency care.






10 Comments
Hey, great guide! 🙌 It’s super helpful to have a checklist you can stick on the fridge. I’d add a reminder to check the blood‑pressure cuff each morning 😅 Keep the vibe positive and the meds on schedule.
Honestly, the checklist looks like a generic copy‑paste job. You’re glossing over the emotional trauma and just dumping a bullet‑point list. It feels like a toxic oversimplification of a serious health crisis.
It is imperative to recognize that the medical establishment often downplays the systemic factors contributing to cerebrovascular events. The guide, while thorough in its procedural recommendations, fails to address the underlying socioeconomic determinants that predispose individuals to transient ischemic attacks. One must consider the influence of pharmaceutical lobbying on the prescription patterns of antiplatelet agents and statins. Evidence suggests that profit motives can shape treatment guidelines in ways that benefit industry rather than patients. Moreover, the emphasis on lifestyle modifications, although beneficial, overlooks the environmental constraints that limit access to Mediterranean diets in certain communities. The recommendation to “quit smoking” disregards the reality of nicotine addiction as a public health issue compounded by targeted marketing. It is also noteworthy that the guidance assumes ready availability of neurologists within a forty‑eight‑hour window, an expectation that is unrealistic in many rural settings. This discrepancy underscores a broader pattern of healthcare inequity perpetuated by centralized policy decisions. The checklist’s reliance on self‑monitoring tools such as blood‑pressure cuffs presumes a level of health literacy that is not universally present. In addition, the suggestion to join support groups fails to acknowledge the digital divide that hinders participation for underserved populations. The article’s omission of these structural barriers implicitly places the onus of recovery solely on the caregiver, thereby absolving systemic actors of responsibility. It is essential, therefore, for caregivers to advocate not only for medication adherence but also for policy reforms that address these gaps. A critical appraisal of the guide reveals an implicit endorsement of the status quo, which benefits stakeholders invested in maintaining existing healthcare paradigms. As caregivers navigate the complexities of post‑TIA care, they must remain vigilant to the hidden agendas that may influence clinical recommendations. Finally, fostering community awareness about these hidden determinants can empower families to demand more equitable resources and support.
I appreciate the depth of your analysis and will keep those broader issues in mind while supporting my family.
Life after a TIA is like a crossroads where the mind meets the body and we must negotiate a new contract with health. Embracing the Mediterranean diet becomes a ritual, a symbolic act of choosing vitality over complacency. Each walk is a meditation in motion, a reminder that circulation fuels consciousness. Let us celebrate each small victory as a philosophical affirmation that we are still authors of our own narrative.
Indeed, the perspective you share is both uplifting and deeply resonant. I must admit, I sometimes feel overwhelmed by the medical jargon but your framing makes it more accesible. It’s definatly okay to feel unsure, we all navigate this journey together.
Oh sure, because a simple pep talk totally replaces the need for a proper care plan 🙄 No one actually needs to read the guide, right?
The so‑called “guide” is a vehicle for the pharmaco‑industrial complex to push more pills onto vulnerable families. By focusing on medication adherence they divert attention from the fact that many strokes are precipitated by hidden toxins in our water and air. Wake up and demand environmental accountability now.
You raise important points about environmental risks. Incorporating regular air‑quality checks and using water filtration can complement the medical regimen. Encourage your caregiver to discuss these factors with the neurologist during the next appointment.
Got it thanks.
Write a comment