Heart Disease – What It Is and How to Protect Your Heart
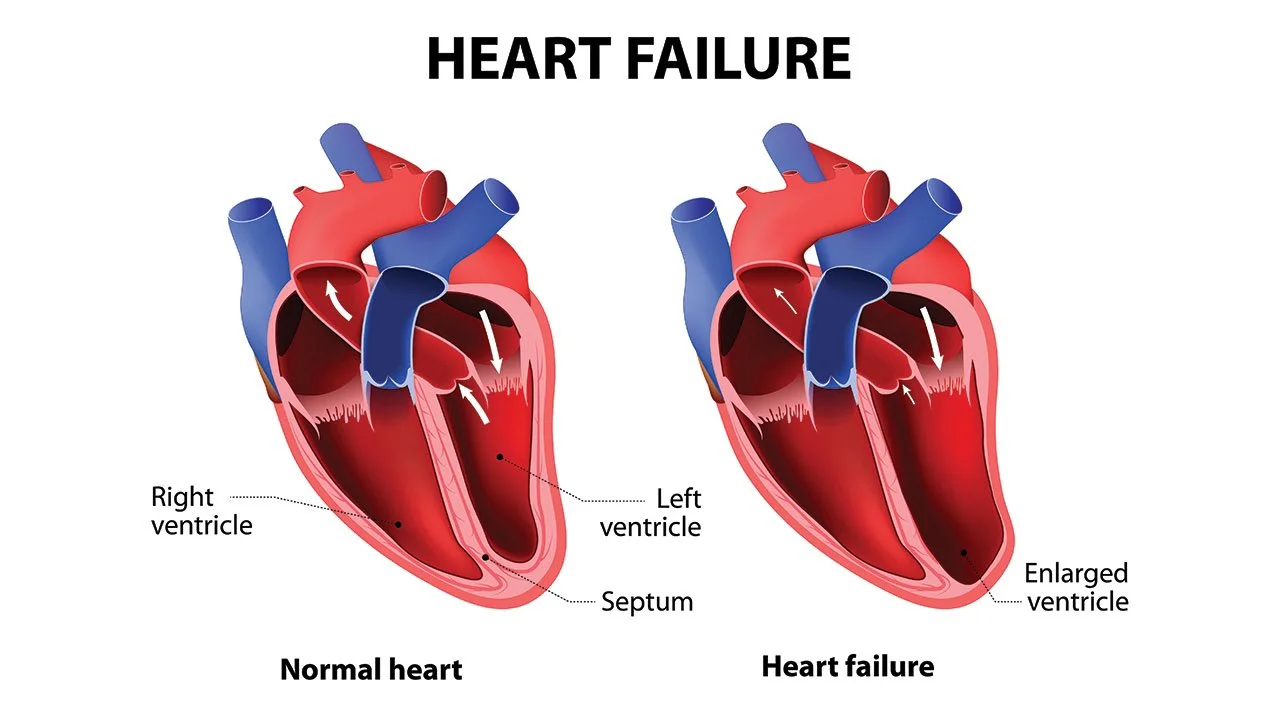
Heart disease is a catch‑all term for conditions that damage the heart or its blood vessels. The most common form is coronary artery disease, where plaque builds up in the arteries and makes it harder for blood to flow. When the heart can’t get enough blood, you might feel chest tightness, shortness of breath, or fatigue. If you ignore the signs, the condition can lead to a heart attack, heart failure, or even death.
Top Lifestyle Tweaks That Lower Heart Risk
First thing to tackle is what you can control. Cutting out smoking is a no‑brainer – even a few cigarettes a day can damage arteries. Next, aim for at least 150 minutes of moderate exercise each week; a brisk walk, cycling, or dancing works just fine. Eating more fruits, veggies, whole grains, and lean protein while trimming sugary drinks and processed snacks helps keep cholesterol and blood pressure in check.
Stress isn’t just a feeling; chronic stress raises blood pressure and can raise inflammation. Simple habits like deep breathing, short walks, or spending time on a hobby can lower stress hormones. Finally, keep an eye on your weight. Losing even five percent of body weight can improve blood pressure, cholesterol, and insulin levels – all big players in heart disease.
Medications You’ll Hear About (Plavix, Lasix, etc.)
If lifestyle changes aren’t enough, doctors often prescribe medicines. Plavix (clopidogrel) is a common blood thinner that stops platelets from clumping together, reducing the risk of clots that could block a coronary artery. It’s especially useful after a stent is placed or if you’ve had a recent heart attack.
For people with fluid buildup from heart failure, diuretics like Lasix (furosemide) help the body get rid of excess water. This eases swelling in the legs and reduces pressure on the heart. If you can’t tolerate Lasix, alternative diuretics such as Torsemide or Bumetanide are also effective and may have fewer side effects.
Other drugs you might encounter include ACE inhibitors, which relax blood vessels and lower blood pressure, and beta‑blockers that slow the heart’s workload. Always talk to your pharmacist about possible interactions – for example, combining Plavix with certain pain relievers can raise bleeding risk.
Monitoring is a big part of treatment. Keep a log of blood pressure, heart rate, and any new symptoms. Simple home devices let you track these numbers and share them with your doctor during check‑ups. Regular blood tests make sure your medication dosage is safe and effective.
Emotional health matters, too. The anxiety that often follows a heart diagnosis can affect sleep, diet, and exercise. Support groups, counseling, or even a chat with a trusted friend can help you stay on track.
Bottom line: heart disease is serious, but it’s also manageable. By quitting smoking, staying active, eating smart, managing stress, and following your doctor’s medication plan, you give your heart the best chance to stay strong. Keep an eye on your numbers, ask questions, and don’t ignore the small warnings – your heart will thank you for it.
The Role of Palliative Care in Chronic Heart Failure Management
- By : Archer Hamilton
- Date : Sep 4 2023
As a health blogger, I feel compelled to discuss the integral role of palliative care in managing individuals with chronic heart failure. This post delves into the complexities of chronic heart disease and highlights palliative care as an effective method in not only mitigating physical symptoms but also offering psychological support. We're going to break down the importance of individualistic care in patient outcomes and analyze the role of physicians and caregivers in this process. Join me in exploring this crucial aspect of heart disease management.