Every year, hundreds of thousands of seniors end up in the hospital-not from falls, heart attacks, or strokes-but because of something preventable: medication errors. It’s not always about taking too much. Sometimes it’s taking the wrong pill, mixing drugs that shouldn’t be mixed, or storing pills where a grandchild can reach them. The truth is, managing medications gets harder with age. Bodies change. Memory fades. Doctors add new prescriptions without removing old ones. And caregivers, often stretched thin, are left trying to keep up.
But here’s the good news: simple, practical steps can cut those risks dramatically. Based on the latest guidelines from the National Institute on Aging, the FDA, and geriatric experts, here are five medication safety tips that actually work-for seniors and the people who help them.
Keep a Live, Detailed Medication List
Most seniors take at least one medication. Nearly 40% take five or more daily. That’s not just pills-it’s vitamins, supplements, over-the-counter painkillers, even herbal teas with active ingredients. And if you can’t name them all, or what they’re for, you’re at risk.
Start with a list that includes:
- Full name of each medication
- Exact dosage (e.g., 10 mg, not "one pill")
- How often to take it (e.g., "once daily at breakfast")
- Why it was prescribed (e.g., "for high blood pressure")
- Name and phone number of the prescribing doctor
- Pharmacy contact info
- Start date
- Any known side effects
- Expiration date
Update this list within 24 hours of any change-whether a new prescription, a dose adjustment, or stopping a drug. Bring it to every appointment, even if it’s just a routine checkup. Pharmacists say 92% of dangerous drug interactions are caught when this list is used. Don’t rely on memory. Don’t write it on a napkin. Use a printed sheet or a digital note you can show on your phone. Keep a copy in your wallet and another in a kitchen drawer.
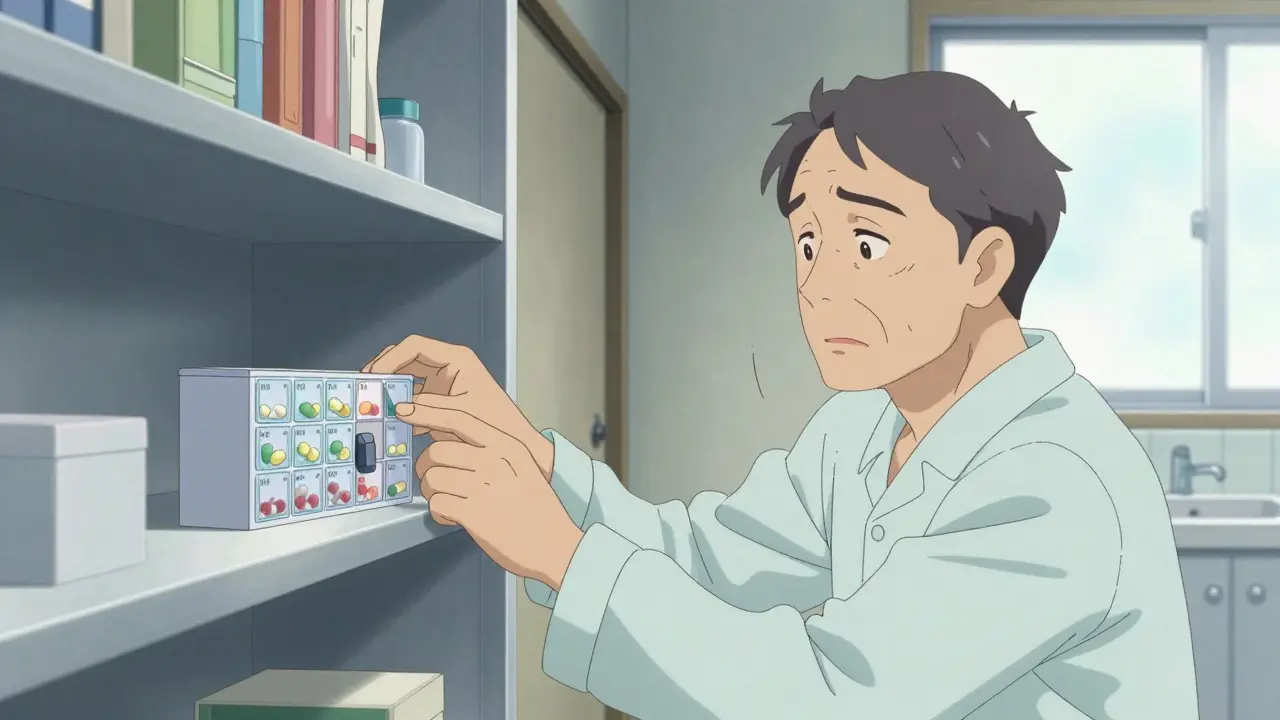
Use a Pill Organizer-But Choose the Right One
Pill organizers aren’t just for show. A 2021 study by the NIA found that color-coded, day-and-time-separated organizers improved adherence by 47% in seniors with mild memory issues. But not all organizers work the same.
Start simple. If someone struggles with small compartments or complex layouts, use a single-day box with AM and PM slots. For those with more complex regimens, go for a 7-day organizer with separate compartments for morning, afternoon, evening, and bedtime. Look for ones with large print labels and easy-open lids.
Some caregivers report success with locked organizers when a loved one doubles up on doses or takes pills at odd hours. One caregiver on Reddit shared how she switched to a locked box after her dad started taking his blood pressure pill twice a day-accidentally. The lock didn’t stop him from taking it; it stopped him from taking it too often.
Don’t rely on apps alone. While tools like Medisafe or Hero (a smart dispenser that alerts caregivers if a dose is missed) help many, 55% of seniors over 75 still prefer paper schedules. If you use a digital tool, pair it with a physical organizer. Tech fails. Paper doesn’t.
Check for Dangerous Interactions
One pill might be fine. Two together? Not always.
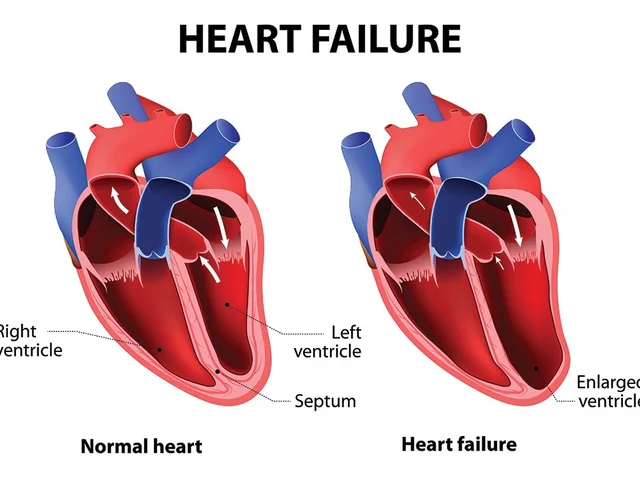
The Beers Criteria®, updated every two years by the American Geriatrics Society, lists 138 medications that are risky for seniors. These include common drugs like benzodiazepines (for anxiety), anticholinergics (for overactive bladder), and NSAIDs like ibuprofen (which can cause kidney damage or stomach bleeding in older adults).
But interactions aren’t just between pills. Grapefruit juice? It interferes with over 85 medications, including statins, blood pressure drugs, and some antidepressants. Alcohol? It clashes dangerously with 150+ drugs-especially sleep aids, painkillers, and diabetes medications. Even OTC cold medicines can spike blood pressure or cause dizziness if mixed with heart meds.
Before starting any new drug-prescription or OTC-ask: "Does this interact with anything else I’m taking?" Then, ask your pharmacist. They’re trained to catch these. Many pharmacies now offer free medication reviews. Take advantage.
Store Medications Correctly (Yes, Even the "Harmless" Ones)
Most people keep their meds in the bathroom. Bad idea.
A 2022 University of Florida study found that 37% of medications lose potency in humid, steamy bathrooms. Heat, moisture, and light degrade pills, creams, and inhalers. The ideal storage? A cool, dry place-like a bedroom drawer or kitchen cabinet-between 68°F and 77°F.
Keep all medications in their original containers. Why? Because labels have critical info: expiration dates, dosage, warnings. Removing them is like throwing away the instruction manual.
And if you have grandchildren visiting? Lock it up. The Poison Control Center reports 60,000 accidental poisonings in children each year from unsecured medications. A locked cabinet or lockbox isn’t overkill-it’s necessary. Even "harmless" supplements like iron or potassium can be deadly to a toddler.
Also, don’t keep expired pills. The average senior home holds $317 worth of unused or expired meds. Dispose of them properly-pharmacies often have take-back bins. Never flush them down the toilet.

Ask the Right Questions at Every Appointment
Doctors are busy. They might not realize you’re taking 12 different pills. So you have to speak up.
Prepare four key questions for every visit:
- Is this medication still necessary?
- What side effects should I watch for?
- Are there cheaper or safer alternatives?
- Could this interact with anything else I’m taking?
These questions aren’t rude-they’re essential. A study from the Alzheimer’s Association found that structured communication like this reduced medication errors by 63% in dementia patients.
Also, ask about deprescribing. That’s when doctors help you stop taking drugs that are no longer needed-or that do more harm than good. For example, if you’re on a statin for cholesterol but have no history of heart disease, your doctor might suggest stopping it. If you’re on a sleep aid that makes you dizzy, they might switch you to a non-drug approach.
And don’t be afraid to ask: "Can we try taking one less pill?" Dr. Michael Steinman, a geriatric specialist at the San Francisco VA, says simplifying a regimen-from four times daily to once daily-can boost adherence from 50% to 90%.
Final Thoughts: It’s About Routine, Not Perfection
Medication safety isn’t about being flawless. It’s about building habits. Studies show it takes 21 to 30 days for a new routine to stick. So pick one tip to start with. Maybe it’s updating your list this week. Or moving your pills out of the bathroom. Or writing down those four questions before your next doctor visit.
And if you’re a caregiver-you’re not alone. 68% of family caregivers say managing medications is their biggest challenge. Use support groups. Talk to pharmacists. Ask for help. The goal isn’t to do everything perfectly. It’s to keep your loved one safe, independent, and out of the hospital.
Small steps. Consistent habits. Clear communication. That’s how you win.
What should I do if my senior parent misses a dose?
Don’t panic. First, check the medication’s instructions-some say to skip the missed dose, others say to take it as soon as you remember. If you’re unsure, call the prescribing doctor or pharmacist. Never double up unless instructed. Use a pill organizer with alarms or a smart dispenser like Hero to prevent future misses. If missed doses happen often, talk to the doctor about simplifying the regimen.
Can I crush pills to make them easier to swallow?
Only if the label or your pharmacist says it’s safe. Many pills-especially extended-release, enteric-coated, or sublingual forms-can become dangerous if crushed. Crushing a time-release pill might release the full dose at once, causing overdose. Always check before crushing. If swallowing is hard, ask about liquid forms, patches, or alternative medications.
Are herbal supplements safe for seniors?
Not always. Supplements like St. John’s Wort, ginkgo, or garlic can interfere with blood thinners, blood pressure meds, and antidepressants. A 2023 AARP survey found 34% of seniors use CBD, which can interact with seizure drugs and liver-metabolized medications. Always list supplements on your medication list and ask your pharmacist about interactions. Just because it’s "natural" doesn’t mean it’s safe.
How do I know if a medication is no longer needed?
Ask your doctor to review all medications at least once a year. This is called a "medication reconciliation." If a drug was prescribed for a short-term issue (like an infection or post-surgery pain) and that issue is resolved, the drug may no longer be needed. The American Geriatrics Society recommends regularly reviewing all prescriptions for risks versus benefits, especially for seniors taking five or more drugs.
Is it okay to use someone else’s leftover medication?
Never. Even if the pill looks the same, the dosage, ingredients, or purpose may be completely different. A pill meant for one person’s high blood pressure could cause dangerously low blood pressure in another. Always get a new prescription. If cost is an issue, ask about generic alternatives, patient assistance programs, or Medicare Part D cost-saving options.





1 Comments
Let me tell you, I used to think pill organizers were for old people who couldn’t keep track - until my dad started taking his blood pressure med twice by accident. Locked box? Game changer. Now he’s got one with alarms, and I get a text if he skips a dose. Tech isn’t perfect, but it’s better than hoping he remembers. Also, I didn’t know grapefruit juice messes with so many meds - now I check every single thing he eats. Small stuff, huge impact.
Write a comment