Every time you swallow a pill, your body is doing something incredible. A tiny chemical enters your bloodstream, travels through your veins, and finds a specific spot in your cells - like a key turning in a lock. That’s how medicines work. But knowing how medicines work isn’t just science class trivia. It’s the difference between feeling better and ending up in the hospital.
Medicines Are Keys, Not Magic
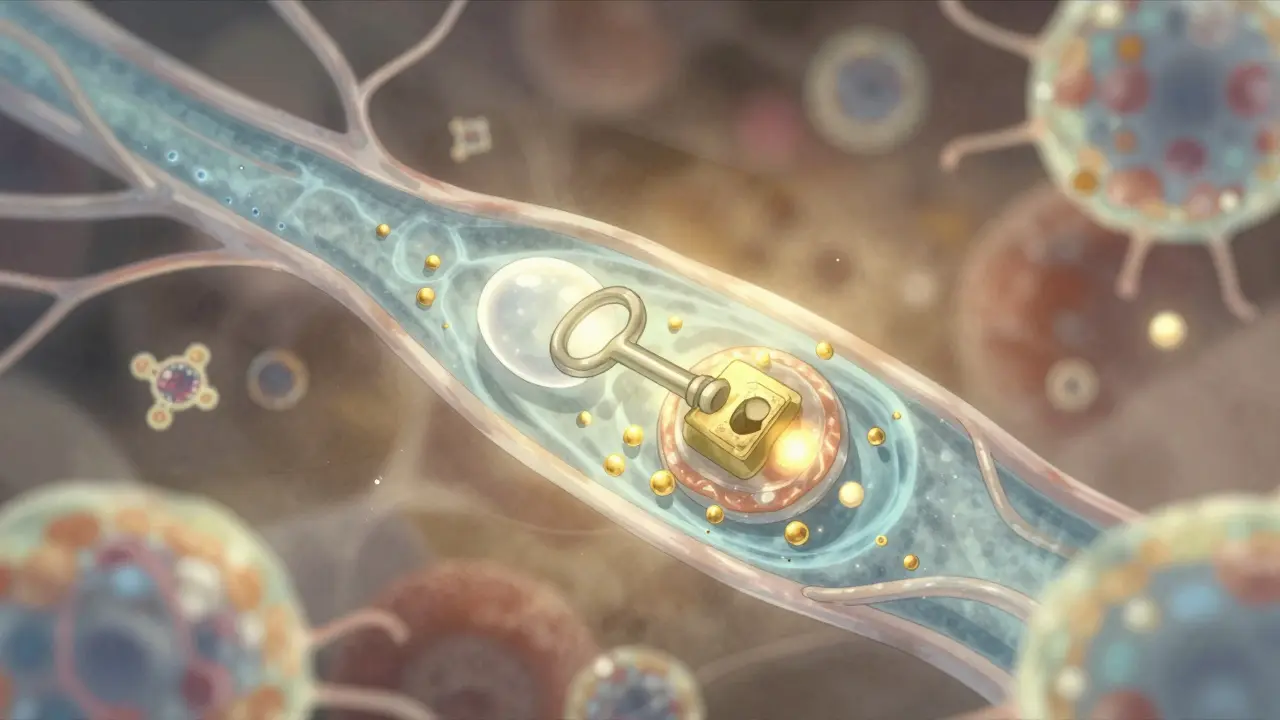
Think of your body as a complex machine with billions of tiny switches called receptors. These receptors control everything from pain signals to heart rate to mood. Medicines don’t magically fix things. They interact with these switches. Some, like aspirin, block a switch that causes inflammation. Others, like fluoxetine (Prozac), stop the body from reabsorbing serotonin, keeping more of it around to lift your mood. This is called the mechanism of action - the exact way a drug changes what’s happening inside you. It’s not guesswork. It’s mapped out in labs, tested in cells, and confirmed in patients. The NIH and FDA now require this level of detail for nearly every new drug. Why? Because without knowing how a medicine works, you can’t predict when it’s safe.Why Some Drugs Are Riskier Than Others
Not all medicines are created equal in terms of safety. Take lithium, used for bipolar disorder. It works, but we still don’t fully understand how. It affects multiple pathways in the brain. That makes it tricky. Too little? Your mood swings return. Too much? You get tremors, confusion, even kidney damage. Doctors must check your blood levels regularly - keeping them between 0.6 and 1.2 mmol/L - to stay in the safe zone. Compare that to statins, like atorvastatin. We know exactly how they work: they block an enzyme (HMG-CoA reductase) that makes cholesterol. Because we understand this, we can monitor your cholesterol levels and adjust the dose. If your levels drop too far, we lower the dose. If they’re still high, we bump it up. It’s precise. It’s predictable. Then there’s warfarin, an old blood thinner. It blocks vitamin K, which your body needs to make clotting factors. But vitamin K is also in spinach, kale, broccoli - lots of greens. If you suddenly eat a big salad every day, your blood gets thinner. If you stop eating greens, you risk clots. Patients who understand this connection are far less likely to have a dangerous bleed or stroke. One Reddit thread with over 4,000 upvotes showed people tracking their greens like a recipe - not because they’re obsessed, but because they learned how the drug actually works.How Your Body Handles Medicine
It’s not just what the drug does to your body - it’s what your body does to the drug. This is called pharmacokinetics. Take morphine. When you swallow it, your liver breaks down about 30% of it before it even reaches your bloodstream. That’s called the first-pass effect. That’s why you need a higher oral dose than an IV dose. Propranolol? Up to 90% gets broken down before it circulates. That’s why some pills are designed to release slowly - so your body doesn’t get overwhelmed. Then there’s protein binding. Most drugs - 95% or more - stick to proteins in your blood. Only the small fraction that’s free can actually do anything. But if you take another drug that also binds to those proteins - say, a common antibiotic like sulfamethoxazole - it can push warfarin off the protein, suddenly flooding your system with too much active drug. That’s why bleeding risk spikes. It’s not the antibiotic causing bleeding. It’s the displacement. And if you don’t know that, you won’t connect the dots.
When Medicines Cross the Line
Some drugs need to get into places your body tries hard to protect. The blood-brain barrier, for example, keeps toxins out of your brain. But if you have Parkinson’s, you need levodopa to get in. That’s why Sinemet® combines levodopa with carbidopa - the carbidopa stops levodopa from breaking down too soon in the gut, letting more of it reach the brain. But sometimes, drugs cross the line when they shouldn’t. Thalidomide, used in the 1950s for morning sickness, was a tragedy. One version of the molecule helped with nausea. The other caused severe birth defects. We didn’t know back then that the body could convert one into the other. Today, we test every single molecular shape - called enantiomers - before approval. That’s why modern drugs like levothyroxine are pure and precise.Why Understanding Your Medicine Reduces Risk
Patients who understand how their medicine works are safer. Period. A 2023 survey by the American Cancer Society found that 78% of patients on trastuzumab (Herceptin) for breast cancer felt more confident when they knew it targeted the HER2 protein. They recognized early signs of heart problems - a known side effect - and reported them sooner. Only 29% of those who didn’t understand the mechanism did the same. On Drugs.com, people taking statins who knew about HMG-CoA reductase inhibition were 3.2 times more likely to notice muscle pain early. That’s important because severe muscle damage (rhabdomyolysis) can be life-threatening. But if you know your drug blocks cholesterol production, and you feel new aches, you call your doctor - not just assume it’s from the gym. Even something as simple as antidepressants: if you stop SSRIs suddenly, you can get dizziness, nausea, brain zaps. Why? Because your brain got used to extra serotonin. If you don’t know that, you think you’re getting sick. But if you understand it’s like pulling the plug on a water pump that’s been running too long, you taper slowly with your doctor’s help.
What You Can Do Right Now
You don’t need a medical degree to stay safe. Here’s what actually works:- Ask your pharmacist: “How does this medicine work in my body?”
- Ask: “What should I watch out for, and why?”
- Ask: “Is there a food, supplement, or other drug I need to avoid - and how does it interfere?”
- Use simple analogies: “Is it like blocking a valve? Or like keeping a signal from shutting off?”





8 Comments
So medicines are basically tiny keys and our bodies are these weird lock systems?? 😅 I always thought pills were magic beans. Now I picture my liver as a bouncer at a club checking IDs before letting drugs in. Also, SSRIs as corked serotonin tubes?? I’m writing that down. 🤯
Understanding mechanism isn’t just useful-it’s ethical. If we don’t know how something alters our biology, how can we consent to its use? This post cuts through the noise. Simple truths matter most.
Warfarin and greens is a perfect example of why patients need context, not just prescriptions. I’ve seen people panic over kale and then ignore their INR levels. Knowledge isn’t power-it’s survival. And yeah, the body’s protein binding thing? Wild. We’re walking chemistry sets.
Western medicine thinks it’s so smart with its ‘mechanisms’ and ‘receptors’-but Ayurveda and Traditional Chinese Medicine have been mapping the body’s energy flows for 5000 years. You think a pill blocking HMG-CoA is deep? Try understanding Prana or Qi. Your ‘precision’ is just a toddler with a microscope. And don’t get me started on how you ignore the mind-body connection while chasing molecular targets.
This is one of the most thoughtful and clinically grounded pieces on patient empowerment I’ve read in recent memory. The emphasis on pharmacokinetics and pharmacodynamics as foundational to safety is not only accurate-it is urgently needed in public discourse. Thank you for framing this not as a technical lecture, but as a call to partnership.
So like... if I take statins and start feeling weird in my muscles... is it just me being lazy or is it the drug?? I mean I went hiking last week so... but also I read that thing about rhabdo and now I’m scared?? Like I don’t even know what that word means but it sounds bad??
Love this. So many people treat meds like candy-pop a pill and hope for the best. But when you understand the why, it becomes part of your daily rhythm. Not scary. Just... respectful. Thank you for making science feel human.
While the mechanistic understanding of pharmaceuticals is indeed commendable, one must also acknowledge the holistic integrity of the human organism. The reductionist approach, though scientifically rigorous, may inadvertently fragment the patient’s experience into biochemical components, neglecting the emergent phenomena of consciousness, emotion, and systemic balance. A truly safe therapeutic paradigm must integrate molecular precision with epistemological humility.
Write a comment