Muscle Stiffness & Diabetes: Cause Identifier
Your Likely Cause
Causes include:
- Insulin resistance affecting glucose uptake in muscle cells
- Advanced Glycation End-products (AGEs) binding to collagen
- Chronic inflammation and nerve damage
Management strategies:
- Improve blood sugar control
- Include magnesium-rich foods
- Regular stretching routine
Causes include:
- Muscle aches and cramping
- Elevated creatine kinase levels
- Localized muscle tightness
Management strategies:
- Review with your doctor about dosage
- Consider CoQ10 supplementation
- Engage in gentle low-impact activities
Causes include:
- Acute onset after sweating
- Dark urine
- Sudden muscle cramping
Management strategies:
- Rehydrate with water and electrolytes
- Stretch immediately after activity
- Maintain consistent hydration
If you’ve ever woken up with legs that feel like a board or notice that everyday movements leave you sore, you might wonder why it’s happening. For many people living with muscle stiffness diabetes, the answer lies in how the body’s sugar regulation messes with muscle tissue, nerves, and circulation. Below you’ll find a clear picture of why this link exists and practical steps you can take to loosen up and feel better.
Why Diabetes Can Make Muscles Stiff
Understanding the root cause helps you target the right solutions. Diabetes, especially Type 2 Diabetes is a chronic condition where the body either resists insulin or doesn’t produce enough, leading to persistently high blood glucose levels, triggers a cascade of changes that affect muscles.
- Insulin Resistance reduces the ability of muscle cells to take up glucose, forcing them to rely on alternative energy pathways that produce more waste products. Those waste products can accumulate and stiffen muscle fibers.
- High blood sugar (hyperglycemia) leads to the formation of Advanced Glycation End‑products (AGEs) chemical compounds that bind to collagen in connective tissue, making it less flexible. When collagen in muscle sheaths hardens, movement feels restricted.
- Chronic low‑grade Inflammation is a hallmark of uncontrolled diabetes and contributes to muscle fiber damage and scar formation. Inflammation also sensitizes nerve endings, amplifying the perception of tightness.
- Peripheral neuropathy, a nerve‑damage complication of diabetes, reduces proprioception (the sense of where your body parts are). Without accurate feedback, muscles may stay contracted longer than needed, creating a feeling of stiffness.
All these mechanisms intertwine, so you often see muscle stiffness alongside other diabetes‑related symptoms like tingling, fatigue, and slow wound healing.
Common Triggers That Worsen Stiffness
Even if you manage your blood sugar well, certain everyday factors can flare up stiffness.
- Medication side effects: Drugs such as Statins cholesterol‑lowering medicines that can occasionally cause muscle aches and reduced flexibility are frequently prescribed to diabetics. If you notice new tightness after starting a statin, talk to your doctor.
- Dehydration: High glucose draws water out of cells, leaving muscles under‑hydrated and more prone to cramping.
- Sedentary lifestyle: Sitting for long periods lets muscles stay in shortened positions, especially the hip flexors and hamstrings, leading to chronic tightness.
- Improper footwear: Poor arch support can force calf and foot muscles to overwork, adding to overall stiffness.
Exercise & Stretching Strategies That Actually Work
Movement is medicine, but the right kind matters.
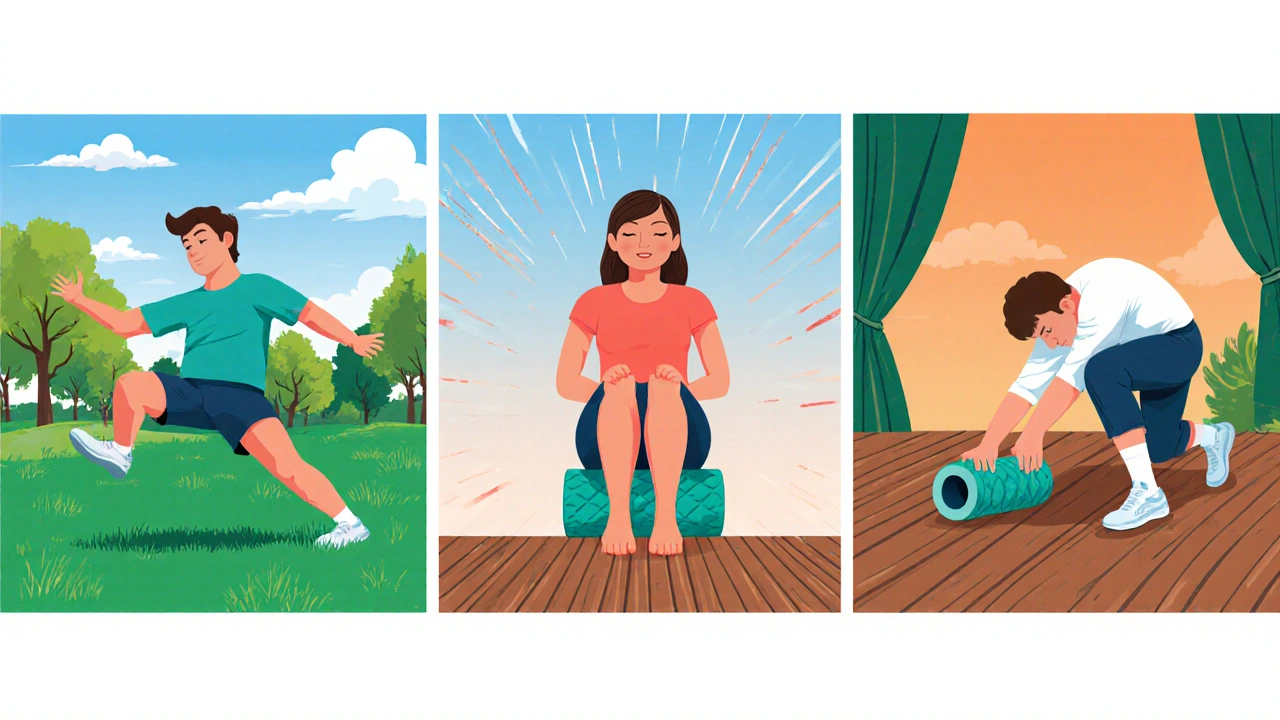
- Dynamic warm‑ups: Before any activity, spend 5‑10 minutes mobilizing joints with leg swings, arm circles, and gentle lunges. This increases blood flow and prepares muscle fibers for work.
- Targeted static stretches: After exercise, hold each stretch for 30‑45 seconds. Focus on:
- Hamstrings - seated forward bend.
- Quadriceps - standing heel‑to‑butt stretch.
- Calves - wall push‑up with one foot back.
- Upper back - clasped‑hands round‑back stretch.
- Strength training with controlled tempo: Use light to moderate weights (10‑15 reps) and pause 2‑3 seconds at the top of each movement. This builds muscle endurance without over‑tightening fibers.
- Low‑impact cardio: Walking, cycling, or swimming for 150 minutes per week promotes circulation, helping glucose get into muscle cells more efficiently.
- Foam rolling: Spend 2‑3 minutes on each major muscle group daily. Rolling breaks up adhesions in fascia, reducing the sensation of a “board‑like” muscle.
Consistency is key. Even short, daily sessions beat occasional marathon workouts when it comes to preventing stiffness.
Nutrition, Hydration & Supplements
What you put into your body directly influences muscle health.
- Stay hydrated: Aim for at least 2‑2.5L of water daily, more if you exercise heavily. Adding a pinch of sea salt can help retain fluids.
- Magnesium: This mineral relaxes muscle fibers. Foods like almonds, pumpkin seeds, and leafy greens are natural sources. If you’re deficient, a 200‑300mg magnesium glycinate supplement before bed can improve night‑time muscle relaxation.
- Vitamin D: Low levels are linked to musculoskeletal pain. A daily dose of 1,000‑2,000IU, especially in winter months, supports muscle function and bone health.
- Balanced protein: Include lean meats, fish, beans, and dairy to supply amino acids needed for muscle repair. Aim for 0.8‑1.0g protein per kilogram of body weight per day.
- Limit processed sugars: Reducing spikes in blood glucose curtails AGE formation, keeping connective tissue more supple.
Medical Interventions & When to Seek Help
Sometimes lifestyle tweaks aren’t enough, and professional care is required.
- Review your diabetes medication regimen: Drugs like Metformin a first‑line oral agent that improves insulin sensitivity and can reduce inflammation are generally neutral for muscle tone, but dosage adjustments may help if blood sugar swings are extreme.
- Physical therapy: A licensed therapist can design a personalized program that addresses specific tight spots, uses modalities like ultrasound, and teaches proper body mechanics.
- Blood sugar monitoring: Keeping fasting glucose under 130mg/dL and HbA1c below 7% (or your doctor’s target) dramatically reduces the biochemical drivers of stiffness.
- Screen for peripheral neuropathy: Early detection via monofilament testing lets you intervene before nerve damage worsens muscle control.
- Medication review for statin side effects: If statins are suspected, doctors may switch to a different lipid‑lowering agent or prescribe a lower dose.
If stiffness interferes with daily activities, causes sharp pain, or is accompanied by swelling, red skin, or sudden weakness, seek medical attention promptly.

Quick Management Checklist
- Check blood glucose before and after exercise; aim for stable readings.
- Hydrate throughout the day; add electrolytes if you sweat heavily.
- Do a 5‑minute dynamic warm‑up before any activity.
- Stretch major muscle groups for at least 30 seconds post‑workout.
- Incorporate foam rolling or self‑myofascial release 3‑4 times a week.
- Consume magnesium‑rich foods daily; consider a supplement if you’re low.
- Schedule a physiotherapy assessment if stiffness persists >2 weeks.
Comparison of Common Causes of Muscle Stiffness
| Cause | Typical Onset | Main Symptoms | Effective Management |
|---|---|---|---|
| Diabetes‑related | Gradual, months-years of poor glycemic control | Diffuse tightness, occasional tingling, reduced flexibility | Improved glycemic control, targeted stretching, magnesium, physio |
| Statin‑induced | Within weeks of starting therapy | Muscle aches, localized tightness, sometimes elevated CK levels | Dose adjustment, co‑enzyme Q10 supplementation, gentle low‑impact exercise |
| Dehydration‑related | Acute, after intense sweating or inadequate fluid intake | Cramping, sudden stiffness, dark urine | Re‑hydrate with water + electrolytes, stretch immediately after activity |
Frequently Asked Questions
Can high blood sugar alone cause muscle stiffness?
Yes. Persistent hyperglycemia promotes AGE formation and low‑grade inflammation, both of which stiffen connective tissue and reduce muscle elasticity.
Is it safe to stretch if my blood sugar is low?
If you’re experiencing hypoglycemia symptoms (dizziness, sweating, shaking), postpone intense stretching until you raise your glucose to a safe level. Light mobility work is usually fine.
Do supplements like magnesium really help?
Clinical studies show magnesium can decrease muscle cramps and improve sleep quality, which indirectly reduces stiffness. Aim for a form with high bioavailability, such as glycinate or citrate.
What role does physiotherapy play?
A physiotherapist assesses muscle length, joint range, and nerve function. They prescribe personalized stretches, strengthening drills, and manual therapy techniques that address the specific ways diabetes affects your musculoskeletal system.
When should I see a doctor about muscle stiffness?
If stiffness lasts more than two weeks, worsens despite home care, is accompanied by swelling, redness, fever, or sudden weakness, schedule a medical evaluation. These could signal infection, deep‑vein thrombosis, or severe neuropathy.







20 Comments
Stiff muscles can really slow you down.
Keep moving even small steps help loosen up 😊
Diabetes‑related muscle stiffness stems from a cascade of metabolic disturbances.
When insulin resistance limits glucose uptake, muscle cells switch to less efficient fuel sources.
The by‑products of those pathways accumulate and can interfere with normal contractile function.
Advanced glycation end‑products, or AGEs, chemically bind to collagen in the extracellular matrix.
This binding reduces the elasticity of the connective tissue surrounding fibers.
Chronic low‑grade inflammation, common in hyperglycemia, further damages muscle proteins.
Nerve damage, or peripheral neuropathy, also contributes by altering feedback loops.
Together these mechanisms create a feeling of tightness that persists even at rest.
Improving glycemic control is the cornerstone of any treatment plan.
Regular aerobic exercise enhances insulin sensitivity and promotes glucose transport into muscles.
Incorporating dynamic warm‑ups before activity prepares the muscles for movement.
Static stretching after workouts lengthens the shortened fibers and improves range of motion.
Magnesium‑rich foods such as almonds, pumpkin seeds, and leafy greens help relax muscle cells.
Supplemental magnesium glycinate before bed can further reduce nighttime cramps.
If stiffness continues, a physical therapist can design a personalized program targeting the affected groups.
Lastly, staying well‑hydrated supports cellular function and prevents the dehydrative component.
By addressing blood sugar, nutrition, activity, and recovery, most people see a noticeable reduction in stiffness.
Enough with the fluff – if you’re on statins and feel tightness, demand a dose review now.
Don’t wait for weeks of agony to prove a point.
CoQ10 isn’t a miracle, but it can cut the pain.
Staying hydrated and moving a little each day can make a big difference.
Even a short walk helps.
From my experience, the combination of low‑impact cardio and consistent foam rolling creates a noticeable loosening of tight muscles.
I schedule a 10‑minute mobility routine every morning, focusing on hip flexors, hamstrings, and upper back.
The dynamic warm‑up primes the circulation, while static holds after the workout restore length.
When blood sugar stays in range, I notice the stiffness recedes faster, likely because the muscles get proper fuel without excess waste products.
It’s a simple habit, but the cumulative effect over weeks is impressive.
Yo man, dehydratin can mak u feel like a board. Drink water + electrolytes after sweatin. Also try some magneisum nuts lol.
Our people need proper health education – no more ignoring diabetes effects.
Looks like another generic health post.
It's good to see practical steps laid out without hype.
Consistency is key.
Let's keep each other motivated – a quick stretch break every hour can keep the stiffness at bay! 💪
Oh great, another "miracle" list – as if popping magnesium will fix everything. 🙄
From a physiological standpoint, the AGE formation is the primary driver of collagen cross‑linking, which directly reduces tissue compliance.
Therefore, targeting hyperglycemia is non‑negotiable for any meaningful improvement.
Don't let the stiffness hold you back – crush it with discipline.
If medication is causing pain, speak up and demand alternatives now.
Wow, you really nailed the science, Basu! 😮💨
Reading that deep dive made me realize how every little habit – from a night‑time snack to skipping a stretch – can tip the balance.
I'm definitely going to add magnesium‑rich meals and a short foam‑roll session each evening.
Thanks for the thorough breakdown, it feels like a roadmap out of that “board‑like” feeling.
Meh, same old advice.
Think of your muscles as a rubber band – keep it supple with color‑ful movement and proper fuel.
Krysta, watch the punctuation – "Effective" needs a capital "E" after the colon, and "Co‑Q10" should include the hyphen. Consistency matters.
Incorrect grammar detected.
Justin, love the positivity – keep the emojis coming, they brighten the thread!
Write a comment