Metabolic syndrome isn't a single disease. It’s a cluster of five warning signs that, when they show up together, mean your body is on a fast track toward heart disease, stroke, and type 2 diabetes. You might have high blood pressure, extra belly fat, and elevated blood sugar - but if your doctor only treats each one separately, you’re missing the bigger picture. This is why metabolic syndrome matters: it’s the red flag that says your metabolism is breaking down, and if you don’t act, your heart will pay the price.
What Exactly Is Metabolic Syndrome?
Metabolic syndrome is diagnosed when you have at least three of five specific conditions. These aren’t vague symptoms - they’re precise, measurable numbers that doctors use to spot trouble early.- Abdominal obesity: Waist size over 40 inches for men, 35 inches for women (lower for Asian Americans: 35 inches for men, 31 inches for women)
- High triglycerides: 150 mg/dL or higher
- Low HDL cholesterol: Under 40 mg/dL for men, under 50 mg/dL for women
- High blood pressure: 130/85 mmHg or higher
- Elevated fasting blood sugar: 100 mg/dL or higher
You don’t need to be obese to have it. Even people who look average on the scale can have dangerous fat buildup around their organs - the kind that triggers inflammation and insulin resistance. That’s the real problem. This isn’t just about weight. It’s about where the fat is, and what it’s doing to your body’s wiring.
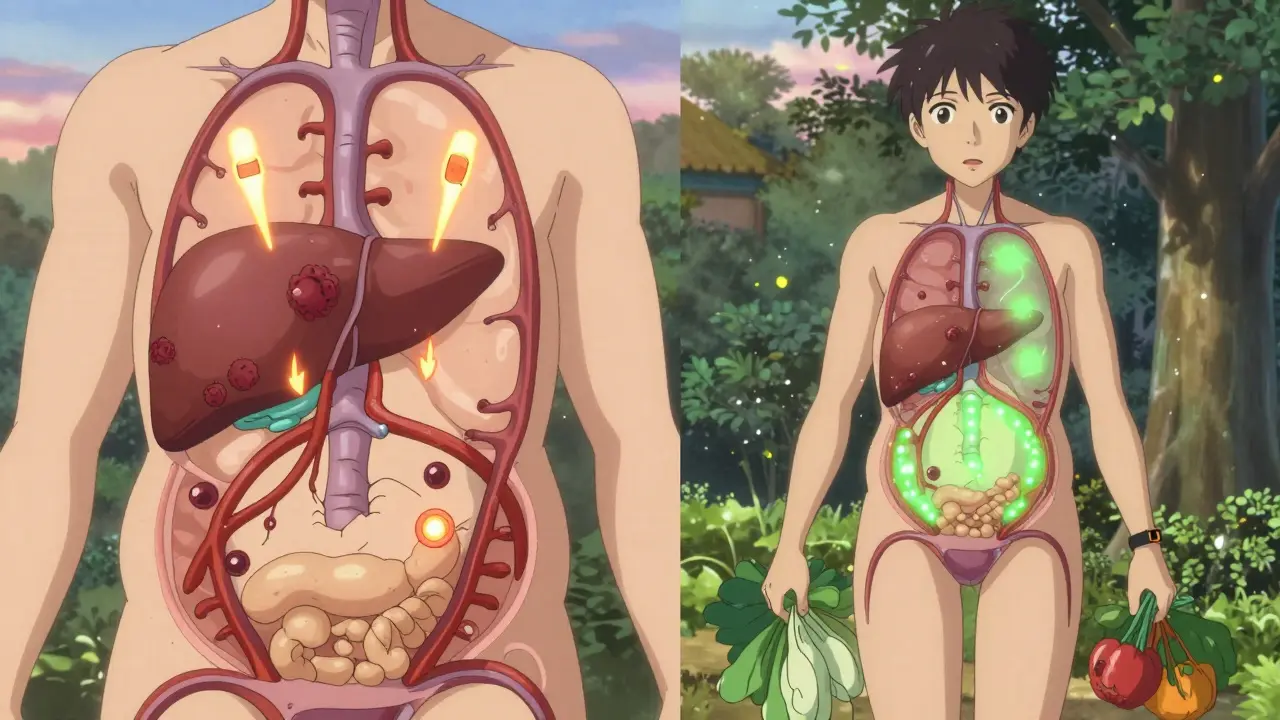
Why It’s More Dangerous Than Single Risk Factors
Having one risk factor - say, high blood pressure - is serious. But having three or more? That’s when the danger multiplies. Studies show people with metabolic syndrome are 1.5 to 2 times more likely to have a heart attack or stroke. Their risk for type 2 diabetes jumps fivefold.That’s because these factors don’t just sit next to each other - they feed off each other. Excess belly fat releases fatty acids that make your liver and muscles less responsive to insulin. Your pancreas then pumps out more insulin to compensate. Over time, your cells stop listening. Blood sugar rises. Fat storage increases. Blood pressure climbs. Inflammation spreads. It’s a domino effect, and it starts in your abdomen.
This is why treating each condition alone - like popping a pill for blood pressure or cholesterol - doesn’t fix the root issue. You’re putting out fires while the whole house is on fire.
The Core Problem: Insulin Resistance
Insulin resistance is the engine behind metabolic syndrome. It’s not just about sugar. It’s about your body’s ability to use fuel properly. When your cells stop responding to insulin, glucose piles up in your blood. Your body tries to fix it by making even more insulin - which then pushes fat into storage, especially around your organs.Dr. Scott M. Grundy, who helped shape the official guidelines, called insulin resistance the "common soil" where all these risk factors grow. That’s why people with metabolic syndrome often have fatty liver, polycystic ovary syndrome (PCOS), or sleep apnea - all linked to the same underlying problem.
Some experts have questioned whether metabolic syndrome is a real condition or just a collection of risks. But large studies, including one from the American Heart Association in 2007, show that having the full cluster predicts diabetes risk better than any single factor alone. The Endocrine Society and the American Heart Association both agree: identifying this pattern saves lives.
Who’s Most at Risk?
About 86.6 million American adults - roughly one in three - have metabolic syndrome. The numbers climb with age: only 20% of people in their 20s and 30s have it, but nearly half of those over 60 do.There are big differences by ethnicity. Hispanics have the highest rate at 38.6%, followed by non-Hispanic whites at 34.2%, non-Hispanic Blacks at 31.8%, and non-Hispanic Asians at 23.5%. But here’s the catch: Asians develop metabolic syndrome at lower waist sizes than other groups. That means someone who looks "normal" could still be at high risk.
Obesity rates have driven this rise. Between 1999 and 2018, the percentage of U.S. adults with abdominal obesity jumped from 46% to nearly 60%. Processed foods, sedentary jobs, and lack of sleep have created the perfect storm.
What Happens If You Ignore It?
Left unchecked, metabolic syndrome doesn’t just lead to heart disease - it accelerates it. The same inflammation that raises your blood pressure also damages your arteries. The extra insulin promotes plaque buildup. High blood sugar gums up your blood vessels like sticky syrup.It’s estimated that 75 to 80% of new type 2 diabetes cases are directly tied to metabolic syndrome. And once diabetes sets in, your risk of heart failure, kidney disease, and nerve damage skyrockets.
The economic cost is staggering. In 2023, heart disease and stroke caused by metabolic syndrome cost the U.S. over $360 billion - $219 billion in medical bills and $143 billion in lost work time.
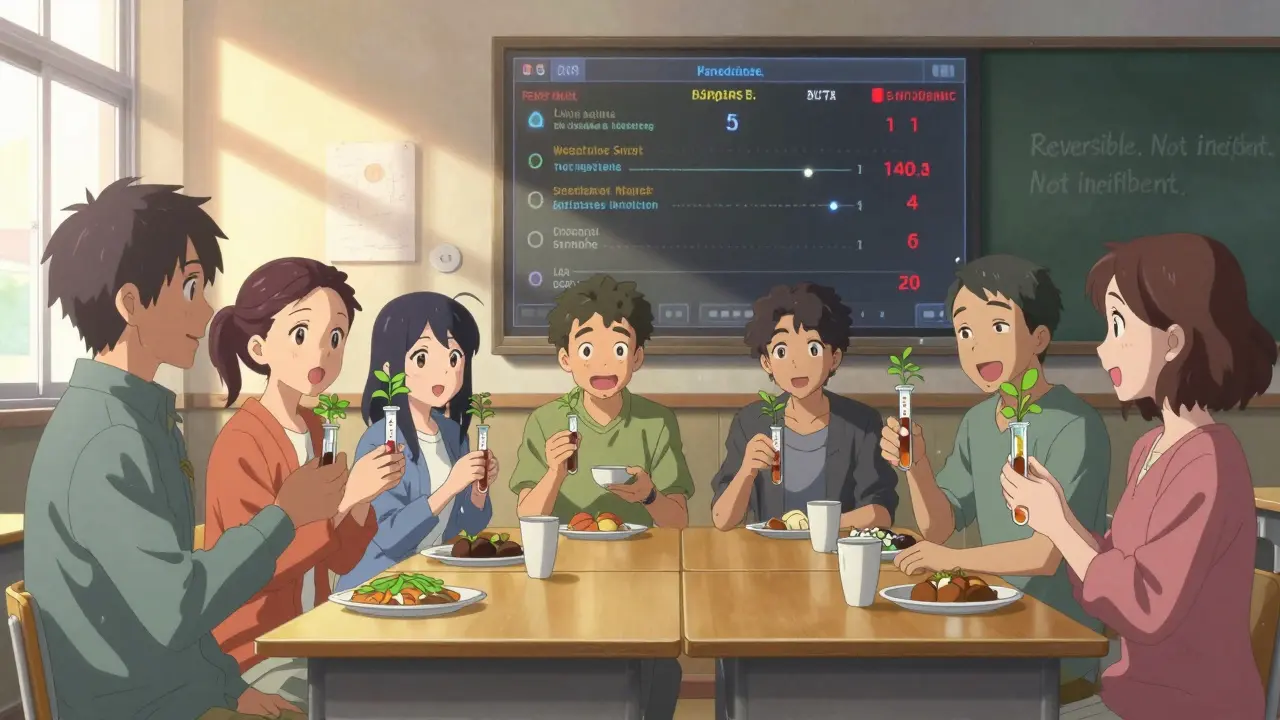
How to Reverse It - Without Pills
The good news? Metabolic syndrome is reversible. And the most powerful tool isn’t a drug - it’s lifestyle change.The Diabetes Prevention Program (DPP), one of the most studied interventions in medical history, showed that losing just 7% of your body weight and getting 150 minutes of brisk walking per week cut the risk of developing diabetes by 58%. That same program reduced metabolic syndrome by 41% over 10 years.
Real people are seeing results:
- Reddit users in r/MetabolicSyndrome reported losing 7.3% of their body weight on average - and seeing 1 or 2 risk factors disappear within 6 months.
- At the Mayo Clinic’s Integrated Metabolic Syndrome Program, 68% of participants reversed their diagnosis after a year of structured coaching.
- A 2018 CDC study found that community health workers helped Hispanic participants lose more weight than standard care - 5.7% versus 4.2%.
What works? Three things:
- Diet: Cut back on sugar, refined carbs, and processed foods. Focus on vegetables, lean protein, whole grains, nuts, and healthy fats. Aim for 1,200-1,500 calories a day for women, 1,500-1,800 for men.
- Movement: Walk 30 minutes a day, five days a week. Strength training twice a week helps too - muscle burns more glucose than fat.
- Consistency: The biggest barrier isn’t willpower - it’s lack of support. People who work with dietitians, exercise physiologists, or group programs stick with it longer.
There’s no magic pill for metabolic syndrome. But there is a powerful one: daily habits.
New Tools Making a Difference
In January 2023, the FDA approved the first digital therapeutic for metabolic syndrome: DarioHealth’s Metabolic+ app. It combines continuous glucose monitoring with personalized coaching. In a clinical trial, users saw their HbA1c drop by 0.6% and waist size shrink by over 3 cm in just six months.Researchers are also exploring genetic markers - like PNPLA3 and TM6SF2 - that help predict who responds best to diet versus exercise. This is the start of personalized prevention.
The American College of Cardiology now recommends that people with metabolic syndrome start statins earlier than usual, because their risk profile is so high. But medication should support lifestyle change - not replace it.
What’s Holding People Back?
Many people don’t even know they have it. A 2022 survey on HealthUnlocked found 68% of users had multiple risk factors but were never told they had metabolic syndrome. Doctors often treat high blood pressure or high cholesterol in isolation, missing the pattern.Another problem? Fragmented care. One doctor handles your blood pressure, another your glucose, another your cholesterol. No one looks at the whole picture. Patients report frustration - feeling like pieces of a puzzle with no one putting them together.
Insurance is another hurdle. Only 28% of Medicare Advantage plans cover full lifestyle programs like the Diabetes Prevention Program. That means many people pay out of pocket for the very interventions proven to work.
Can It Be Cured?
Yes. Not just managed - reversed.The DiRECT trial, published in The Lancet, followed 300 people with type 2 diabetes and metabolic syndrome. Half followed an intensive weight loss program: a low-calorie diet (825-850 calories/day) for 3-5 months, followed by gradual food reintroduction and long-term support. After one year, 46% of participants had reversed both their diabetes and metabolic syndrome. Many were off all medications.
That’s not a miracle. It’s biology. When you lose weight - especially visceral fat - your body regains its sensitivity to insulin. Blood pressure drops. Triglycerides fall. HDL rises. Blood sugar normalizes.
It’s not easy. But it’s possible. And the sooner you start, the better your chances.
Can you have metabolic syndrome without being overweight?
Yes. While abdominal obesity is one of the five diagnostic criteria, some people - especially those with genetic or hormonal factors like PCOS - can develop insulin resistance and other metabolic issues even at a normal weight. The key is waist measurement, not overall weight. A man with a 41-inch waist and normal BMI can still have metabolic syndrome.
Does metabolic syndrome always lead to diabetes?
No, but it greatly increases the risk. About 75-80% of new type 2 diabetes cases are linked to metabolic syndrome. However, with lifestyle changes - especially weight loss and regular activity - you can prevent or delay diabetes entirely. Many people reverse the syndrome before diabetes develops.
What’s the best diet for metabolic syndrome?
Focus on whole, unprocessed foods: vegetables, fruits, legumes, whole grains, lean proteins, nuts, seeds, and healthy fats like olive oil and avocado. Avoid sugary drinks, white bread, pastries, fried foods, and processed snacks. The Mediterranean diet and DASH diet are both proven to improve all five risk factors. Portion control matters - aim for 1,200-1,800 calories daily depending on gender and activity level.
Can exercise alone fix metabolic syndrome?
Exercise helps - a lot - but it’s not enough alone if diet isn’t addressed. A person who walks 30 minutes a day but still eats a lot of sugar and refined carbs won’t reverse their condition. The most effective approach combines movement with dietary changes. Studies show weight loss is the strongest predictor of improvement.
Are medications necessary for metabolic syndrome?
Medications aren’t a cure, but they can help manage individual components while you work on lifestyle changes. For example, statins for cholesterol, ACE inhibitors for blood pressure, or metformin for blood sugar. But no drug treats metabolic syndrome as a whole. Lifestyle change remains the only proven way to reverse it.
What Should You Do Next?
If you’ve been told you have high blood pressure, high cholesterol, or prediabetes - don’t wait. Ask your doctor: "Could I have metabolic syndrome?" Request your waist measurement, fasting glucose, and lipid panel if you haven’t had them recently.If you’re diagnosed, don’t panic. This isn’t a life sentence. It’s a wake-up call. Start small: swap soda for water, take a 20-minute walk after dinner, cook one more meal at home this week. Track your progress - not just on the scale, but on your waist, energy levels, and blood pressure.
Metabolic syndrome is preventable. It’s reversible. And the time to act is now - before your heart pays the price.






14 Comments
Metabolic syndrome isn't just a medical label-it's a systemic failure of how we eat, move, and survive in modern society. The body isn't broken; it's responding perfectly to the environment we've created. Processed carbs, sedentary work, chronic stress, and sleep deprivation? That's not an accident. It's the default setting. And now we're surprised when insulin resistance kicks in? We're basically feeding our cells sugar water while telling them to run a marathon.
The real tragedy is that we treat symptoms like isolated bugs in software, when the whole operating system is corrupted. You can't fix high blood pressure with a pill if your liver is drowning in fructose. You can't lower triglycerides with statins if your pancreas is screaming for help.
It's not about willpower. It's about architecture. Our biology evolved to store fat during scarcity. Now we live in constant abundance. Our genes didn't get the memo. And we're punishing people for being biologically accurate.
I love how this post breaks it down without jargon. My grandma had all five markers and never knew it until she had a stroke. She was ‘just a little overweight’ and ‘always had high BP.’ No one ever connected the dots. We need to stop treating numbers in isolation. This isn’t a checklist-it’s a cry for help from your own body.
I’ve been working with patients who have metabolic syndrome for years. The biggest barrier isn’t knowledge-it’s access. People in food deserts can’t just ‘eat more vegetables.’ They need affordable produce, safe places to walk, and time off work to cook. Policy change has to match medical advice.
They’re lying to you. Metabolic syndrome is a scam invented by Big Pharma to sell statins and metformin. The real cause? Glyphosate in your food and 5G messing with your mitochondria. You want to reverse it? Stop eating anything with an ingredient list longer than three words and unplug your WiFi at night. Also, drink lemon water. It’s been proven since 1923.
It’s frankly irresponsible that the medical community still allows the term ‘metabolic syndrome’ to be used without acknowledging its roots in the obesity epidemic driven by corporate greed and the collapse of public nutrition education. The fact that we’re still debating whether it’s a ‘real condition’ while children are being diagnosed with prediabetes at age 10 is a moral failure of epic proportions. The American Heart Association and Endocrine Society may have consensus, but they’re also funded by pharmaceutical sponsors who profit from lifelong medication regimens. The only cure is systemic change-not individual willpower.
And yet, here we are, blaming the patient for not walking more while their neighborhood has no sidewalks, no grocery stores, and a corner store selling sugary drinks on every block. This isn’t biology-it’s structural violence.
The DiRECT trial? Brilliant. But it only worked because participants had intensive support, access to low-calorie meal replacements, and no financial burden. Most people can’t afford that. So yes, it’s reversible-but only if you’re rich enough to afford the cure.
Who cares? This is just another way for liberals to guilt-trip Americans into eating kale. We used to be strong. We ate bacon, fried chicken, and soda and still built this country. Now we’re afraid of our own shadows. If you want to live longer, don’t eat so much. Simple. No app. No coach. No ‘DarioHealth.’ Just stop being lazy.
OMG I JUST REALIZED I HAVE 4 OF THE 5 THINGS. I’m not even fat but my waist is 38 and my fasting glucose was 102. My doctor said ‘eh, keep an eye on it.’ Like… that’s it?? I’m 34. I don’t want to be diabetic by 40. This post scared me but also gave me hope. Thank you.
❤️ This is so important. I’ve been coaching women with PCOS and metabolic syndrome for years, and the one thing they all say is: ‘No one ever told me this was connected.’ You’re not broken. Your body is trying to survive. Start with one change-swap soda for sparkling water. That’s it. You don’t need to overhaul everything today. Just begin. You’ve got this. 💪
Okay but let’s be real-how many of these people who ‘reversed’ metabolic syndrome were rich white women with time off work, personal chefs, and yoga retreats? The DPP program? Great for people who can afford to quit their job for a year. The CDC study? Only worked because community health workers were paid to babysit people’s diets. Meanwhile, my cousin works two jobs, gets home at 9 PM, and feeds her kids ramen because it’s $1.50. You tell her to ‘cook more meals at home.’ Good luck. This isn’t a health crisis-it’s a class war.
And don’t even get me started on the ‘FDA-approved app.’ Of course they made an app. That’s how tech companies make money off desperation. Meanwhile, Medicare won’t cover a single nutritionist visit. Wake up.
This is just western medicine nonsense. In Nigeria we don’t have this problem. We eat plantains and beans. You eat processed food you get sick. Simple.
I’ve seen patients come in terrified after being diagnosed. They think it’s a death sentence. But the moment they realize it’s reversible, their whole demeanor changes. It’s not about perfection. It’s about progress. One walk. One less soda. One night of sleep. Small steps matter more than we admit.
Wow. So let me get this straight. We’re supposed to believe that eating a donut and sitting at a desk for 12 hours is what’s killing us… but the solution is… more walking? And eating ‘whole grains’? That’s it? No wonder people are skeptical. This reads like a wellness influencer’s PowerPoint. Where’s the real systemic solution? Or is this just another guilt trip disguised as science?
For anyone reading this and feeling overwhelmed: start with one meal. Make it vegetables and protein. No sauce. No sugar. Just food. Do that for a week. Then add a 10-minute walk. Don’t aim for 150 minutes. Aim for 10. Consistency beats intensity every time. You don’t need to be perfect. You just need to begin. And you’re not alone in this.
Replying to @6774: You’re right to be skeptical. This isn’t just about willpower-it’s about power. The people who benefit from metabolic syndrome are the ones selling the pills, the apps, the ‘lifestyle programs’ that cost $500/month. The real solution? Universal healthcare with free nutrition counseling. Subsidized healthy food. Paid time off for wellness. Zoning laws that don’t allow a liquor store on every corner. But those aren’t sexy. They don’t make ads. So we get apps and guilt.
The post isn’t wrong. It’s just incomplete. It tells you what to do, but not who’s stopping you from doing it.
Write a comment