Anticholinergic Burden Calculator
Add Your Medications
Your Medication List
Your Anticholinergic Burden Score
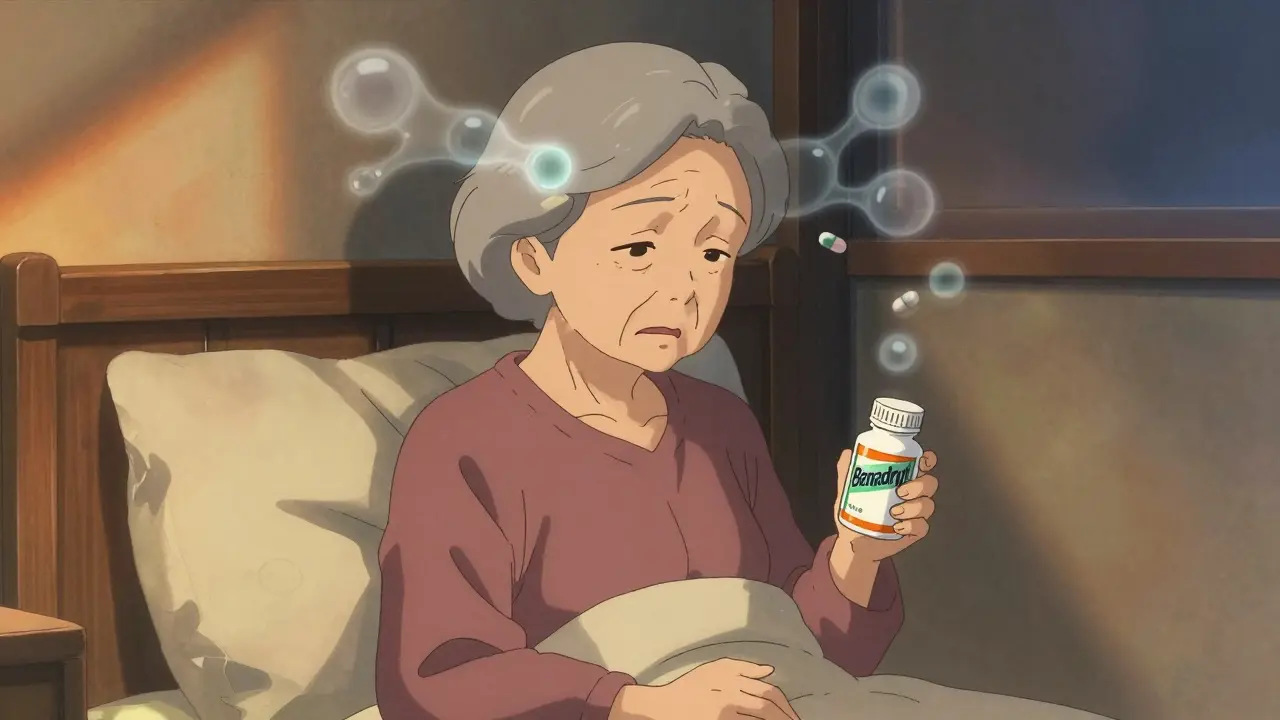
For years, millions of older adults have reached for over-the-counter antihistamines like Benadryl to help with allergies, colds, or trouble sleeping. It’s cheap, easy to find, and seems harmless - until you hear whispers about dementia. Is there real danger? Or is this just another health scare? The truth is more complicated than a simple yes or no, but the evidence is strong enough that doctors are now warning people to think twice before using these drugs long-term.
Why Antihistamines Might Be Riskier Than You Think
Not all antihistamines are the same. There are two main types: first-generation and second-generation. The first-generation ones - like diphenhydramine (Benadryl), doxylamine (Unisom), and chlorpheniramine - cross the blood-brain barrier. That’s why they make you drowsy. But that same property lets them block acetylcholine, a brain chemical essential for memory and thinking. This is called anticholinergic activity. Over time, consistently blocking this neurotransmitter may interfere with how the brain functions. Second-generation antihistamines - such as loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) - were designed to avoid this. They don’t cross into the brain as easily. That’s why they don’t usually cause drowsiness. And crucially, they have almost no anticholinergic effect. If you’re taking an antihistamine regularly, this distinction matters more than you might realize.The Research: What the Studies Actually Say
One of the most cited studies came out in 2015 in JAMA Internal Medicine. Researchers followed over 3,400 people aged 65 and older for a decade. They found that those who took anticholinergic medications - including certain antidepressants, bladder meds, and some antihistamines - had a higher risk of dementia. But here’s the twist: when they looked specifically at antihistamines, the risk wasn’t significant. The real red flags were for drugs used to treat depression and overactive bladder. A 2019 follow-up study by the same team confirmed this. Antihistamines showed no increased dementia risk (hazard ratio of 1.00), while antidepressants raised risk by 29% and bladder meds by 65%. So why do people still worry about Benadryl? Some studies have grouped all anticholinergic drugs together, making it look like antihistamines are dangerous. But when you separate them, the signal fades. A 2022 study of nearly 9,000 older adults found dementia rates were slightly higher in those using first-gen antihistamines - 3.83% vs. 1% in second-gen users - but the difference wasn’t statistically significant. In plain terms: it could’ve been due to chance. Even more confusing, a 2023 analysis from the UK Biobank found no link between antihistamine use and dementia when researchers accounted for sleep disorders. That suggests people who take these drugs for sleep might already be at higher dementia risk because of poor sleep quality - not because of the drug itself.Why Doctors Still Say Avoid Them
Despite the mixed evidence, major medical groups are still warning against first-generation antihistamines in older adults. The American Geriatrics Society’s 2023 Beers Criteria - the gold standard for prescribing in seniors - lists diphenhydramine and doxylamine as drugs to avoid. Why? Because the risk, while not proven, is plausible. And when you’re dealing with brain health, you don’t wait for absolute proof to change course. Think of it like smoking. We didn’t need 100% certainty to warn people decades ago. The pattern was clear enough. Same here. The anticholinergic burden adds up. If someone is taking diphenhydramine nightly for sleep, plus an antidepressant, plus a bladder med, their total anticholinergic load is high. That’s when the risk becomes real. The Anticholinergic Cognitive Burden Scale (ACB) rates diphenhydramine as a level 3 - the highest possible. That means it’s known to cause cognitive side effects. Fexofenadine? Level 0. No effect. So if you’re on multiple meds, swapping out one high-risk drug can make a difference.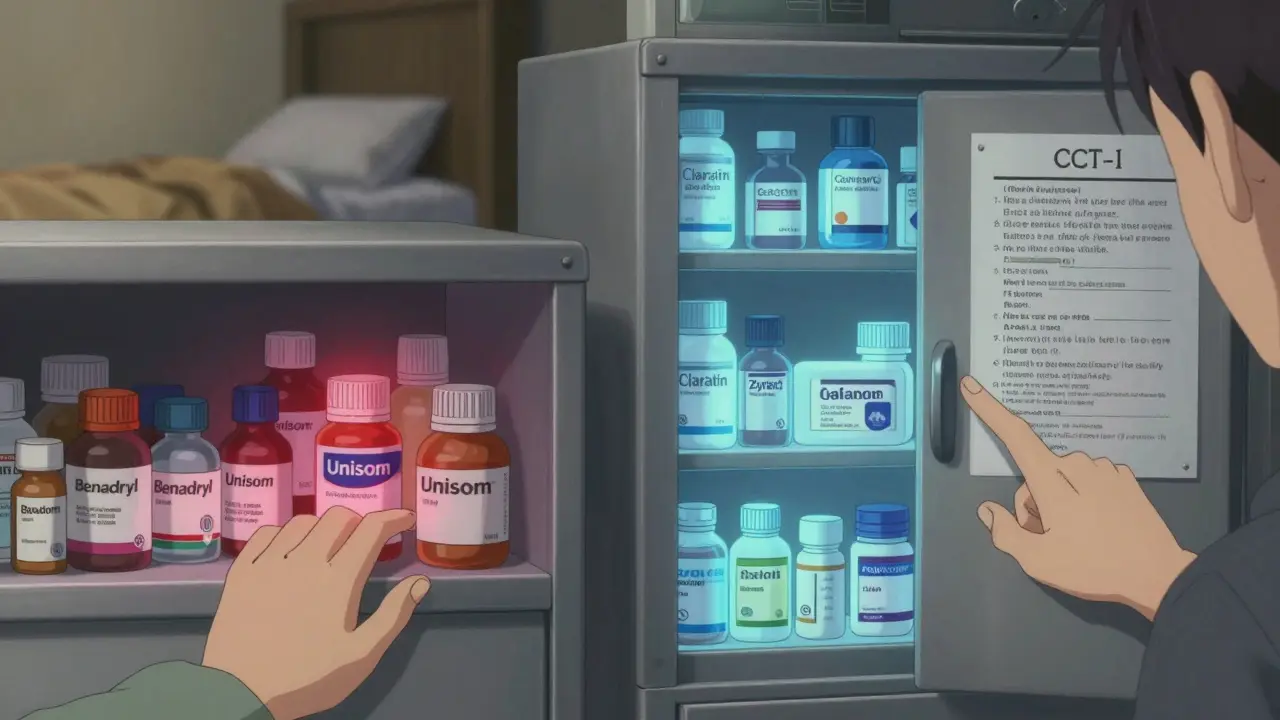
What People Are Really Using These For
Here’s the uncomfortable truth: most older adults aren’t taking these for allergies. They’re using them as sleep aids. A 2022 survey by the National Council on Aging found that 42% of adults 65+ use over-the-counter antihistamines regularly to fall asleep. And 78% had no idea these drugs have anticholinergic effects. Reddit threads and AgingCare.com forums are full of stories like this: “My mom took Benadryl for years. Now she has dementia. Was it the pills?” These aren’t just fears - they’re lived experiences. And while science hasn’t proven causation, the timing is suspicious. Poor sleep, brain fog, confusion - these are early signs of cognitive decline. And if you’re masking them with a drug that worsens them, you’re stuck in a cycle.What to Do Instead
If you’re using diphenhydramine for sleep, you need a better plan. The best alternative isn’t another pill - it’s cognitive behavioral therapy for insomnia, or CBT-I. Studies show it works in 70-80% of older adults. It teaches you how to retrain your brain to sleep without drugs. The problem? It’s hard to find. Therapists are scarce, and Medicare only pays $85-$120 per session. Wait times can be over two months. There are other options. Low-dose doxepin (Silenor) is a prescription sleep aid with minimal anticholinergic activity (ACB score of 1). Melatonin, while not a miracle cure, has no anticholinergic effect and is safe for long-term use. Non-drug strategies like keeping a cool, dark room, avoiding screens before bed, and getting morning sunlight can also help reset your sleep cycle. For allergies, switch to a second-generation antihistamine. Claritin, Zyrtec, or Allegra work just as well without the brain fog. If you’re using them for cold symptoms, ask your doctor if you really need them. Most colds resolve on their own in 7-10 days. You don’t need to take antihistamines for that long.
What’s Changing Right Now
The market is shifting. First-gen antihistamine sales dropped 24% between 2015 and 2022. Second-gen sales grew by nearly 20%. Drug labels are starting to change, too. The European Medicines Agency now requires warnings about “potential long-term cognitive effects” on packaging. The FDA is reviewing all anticholinergic drugs and will release findings in mid-2024. A major new study called ABCO, funded by the NIH, is tracking 5,000 older adults for 10 years. It’s the most detailed look yet at how these drugs affect the brain over time. Results won’t be in until 2033, but early data from the UK Biobank suggest the real culprit might not be the drug - it’s the underlying condition driving its use.What You Should Do Today
If you’re 65 or older and taking diphenhydramine, doxylamine, or chlorpheniramine regularly - stop assuming it’s safe. Talk to your doctor or pharmacist. Ask: Is this still necessary? Is there a safer alternative? Don’t just quit cold turkey - especially if you’re using it for sleep. Withdrawal can cause rebound insomnia. Work with a professional to taper off and replace it with something better. Check your medication list. If you’re taking more than one anticholinergic drug, even low-dose ones, your risk adds up. Use the ACB scale as a guide: anything rated 2 or 3 should be reviewed. Second-gen antihistamines? Fine. Melatonin? Fine. CBT-I? Worth a try. And if you’re a caregiver, don’t wait for a crisis. Look in the medicine cabinet. If you see bottles of Benadryl or Unisom, ask why they’re there. Chances are, it’s for sleep. And there’s almost always a better way.Frequently Asked Questions
Do all antihistamines increase dementia risk?
No. Only first-generation antihistamines like diphenhydramine (Benadryl), doxylamine, and chlorpheniramine have strong anticholinergic effects linked to potential cognitive decline. Second-generation antihistamines - such as loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) - do not cross the blood-brain barrier significantly and have little to no anticholinergic activity. They are considered safe for long-term use in older adults.
Is it safe to take Benadryl occasionally?
Taking Benadryl once in a while - say, for a bad allergic reaction or a single night of poor sleep - is unlikely to cause harm. The concern is long-term, daily, or nightly use over months or years. The brain doesn’t react to occasional exposure the same way it does to chronic blockade of acetylcholine. If you’re using it regularly, it’s time to find a better solution.
What’s the best replacement for Benadryl for sleep?
The most effective non-drug option is cognitive behavioral therapy for insomnia (CBT-I), which works for 70-80% of older adults. For medication, low-dose doxepin (Silenor) is a prescription sleep aid with minimal anticholinergic effects. Over-the-counter melatonin is also safe and doesn’t interfere with brain chemistry. Avoid combining any sleep aid with alcohol or other sedatives.
Why do doctors still prescribe Benadryl if it’s risky?
Many doctors prescribe it out of habit, because it’s cheap, familiar, and patients ask for it. Also, sleep problems are often under-treated, and alternatives like CBT-I are hard to access. But awareness is growing. The American Geriatrics Society now explicitly advises against it for older adults, and more prescribers are switching to safer options. If your doctor recommends Benadryl, ask if there’s a better alternative.
Should I stop taking my antihistamine right away?
Don’t stop suddenly, especially if you’ve been using it for sleep. Stopping can cause rebound insomnia or withdrawal symptoms. Instead, talk to your doctor or pharmacist. They can help you taper off safely and replace it with a non-anticholinergic option. Even switching from diphenhydramine to loratadine for allergies is a simple, low-risk change that can reduce your overall anticholinergic burden.