Why Monitoring Rheumatoid Arthritis Matters More Than You Think
Rheumatoid arthritis isn’t just about sore joints. Left unchecked, it can destroy cartilage, erode bone, and cripple mobility in months-not years. That’s why monitoring isn’t optional. It’s the difference between managing symptoms and stopping damage before it’s visible on an X-ray. The tools doctors use-CDAI, DAS28, and imaging-aren’t just numbers on a chart. They’re the only way to know if your treatment is actually working.
Back in the 1990s, rheumatologists guessed. Now, they measure. And that shift has cut joint damage by up to half in patients who stick with regular monitoring. The goal isn’t just to feel better. It’s to reach remission-where disease activity is so low, your joints stop being attacked. But you can’t get there without knowing where you stand.
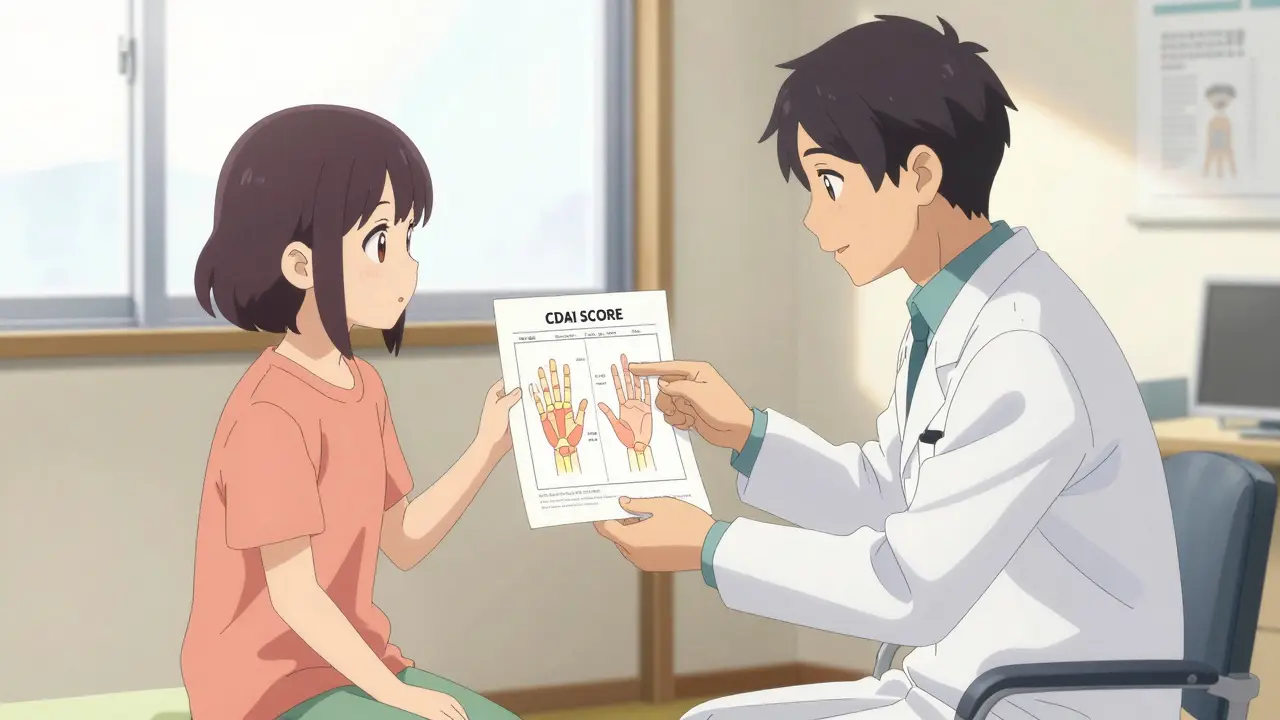
CDAI: The Simple Score That Changed Everything
CDAI stands for Clinical Disease Activity Index. It’s simple: add up four things-how many tender joints you have, how many swollen joints, how bad your pain feels on a scale of 0 to 10, and how bad your doctor thinks your disease is on the same scale. No blood tests. No machines. Just a quick check-up.
That’s why it’s the most used tool in U.S. rheumatology clinics. In 2023, 78% of practices used CDAI in over half their visits. Why? Because it’s fast. It takes less than two minutes. It fits into a regular appointment. And it’s reliable. Studies show it matches what doctors actually see better than any other score.
The numbers tell you everything:
- Remission: Under 2.8
- Low disease activity: 2.8 to 10
- Moderate: 10 to 22
- High: Over 22
If your score jumps from 5 to 15 in three months, your doctor knows your meds aren’t working. No waiting for lab results. No guessing. You adjust treatment right away. And that’s why CDAI predicts future joint damage better than anything else-patients with scores over 22 are over four times more likely to develop new erosions.
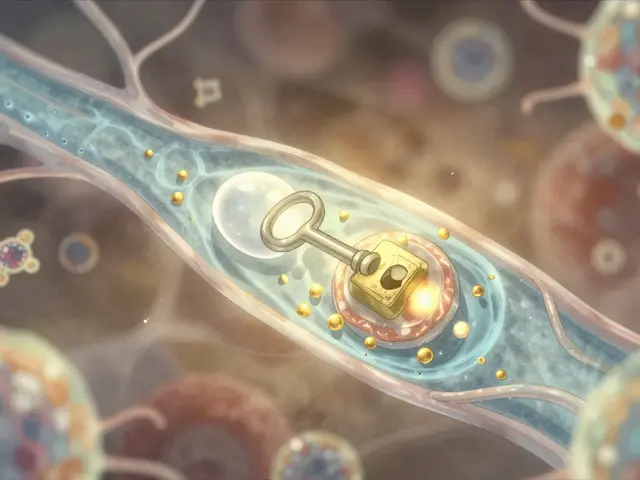
DAS28: The Score That Needs Blood Work
DAS28 is more complex. It uses the same joint counts as CDAI, but adds a blood test-either ESR (erythrocyte sedimentation rate) or CRP (C-reactive protein). These measure inflammation in your body. So while CDAI tells you how you feel and how your joints look, DAS28 tells you what’s happening inside.
There are two versions: DAS28-ESR and DAS28-CRP. CRP is more responsive to changes, so most doctors now use that one. The formula looks scary, but you don’t need to calculate it. Your clinic’s software does it. The score ranges from 0 to 10, with these thresholds:
- Remission: Under 2.6
- Low: 2.6 to 3.2
- Moderate: 3.2 to 5.1
- High: Over 5.1
Here’s the catch: you need blood work. And labs don’t always deliver results on the same day. In 68% of cases, doctors have to make treatment decisions without knowing your CRP. That means they might hold off on changing meds-waiting for results that come hours later. That delay can cost you. A 2022 study found that when labs are late, patients stay in moderate or high disease activity longer than they should.
So why use it? Because it catches hidden inflammation. Some patients feel fine but have high CRP. That’s a red flag. CDAI would say they’re in remission. DAS28 says they’re not. That’s why European clinics still prefer it. But in the U.S., simplicity wins. That’s why CDAI is now the go-to for daily use.

Imaging: Seeing What Your Eyes Can’t
Even the best scores can miss damage. That’s where imaging comes in.
Traditional X-rays have been the gold standard since the 1940s. They show bone erosion and joint space narrowing. But they’re slow. It takes 6 to 12 months before damage shows up. By then, it’s already done. You can’t reverse it. That’s why X-rays are used mostly for long-term tracking-not for checking if your new drug is working.
Ultrasound is faster. It uses sound waves to show swollen synovium (the lining of your joints) and increased blood flow-signs of active inflammation. It’s done right in the clinic. You see it on the screen. Your doctor points to the red spots on the screen and says, “This is what’s hurting you.” Studies show it finds synovitis 20% better than a physical exam. And it changes treatment in 22% of cases where doctors would’ve done nothing otherwise.
MRI is the most sensitive. It shows bone edema-swelling inside the bone-months before X-rays show erosion. That’s huge. Bone edema is the earliest sign that your immune system is attacking your bones. If you catch it early, you can stop it. But MRI costs around $1,200 in the U.S. Most insurance won’t cover it unless you’re in a clinical trial or have rapidly worsening disease. So it’s not for routine checks. It’s for high-risk cases.
Here’s what the numbers say:
- Ultrasound detects synovitis in 85% of cases where physical exams miss it
- MRI predicts future bone erosion with 89% accuracy
- X-rays need 5+ points of progression per year to be considered “active disease”
When to Use What? A Practical Guide
You don’t need all three every visit. Here’s how most clinics do it:
- Every 3 months: CDAI. Quick, no labs, tracks how you’re doing overall.
- Every 6 months: DAS28-CRP. If your CDAI is high or you’re not improving, check for hidden inflammation.
- At diagnosis and annually: X-ray. To track long-term damage.
- If you’re not responding: Ultrasound. To see if there’s hidden joint inflammation.
- If you have severe disease or rapid progression: MRI. To check for bone edema and plan aggressive treatment.
Some clinics now use digital tools like the ACR’s “RA Monitor” EHR module. It auto-calculates CDAI, flags scores over 10, and suggests an ultrasound referral. That’s the future: smarter, faster, more targeted.
The Gaps: What These Tools Miss
None of these tools measure fatigue. Or brain fog. Or how hard it is to button your shirt. And that’s a problem.
One study found that fatigue accounts for 14% of what makes patients feel worse-but CDAI and DAS28 don’t include it. That’s why some patients feel “fine” on paper but still can’t get out of bed. Doctors are starting to add patient-reported outcomes (PROMs) to the mix. Apps like RheumaTrack let you log fatigue, pain, and stiffness before your visit. That data gets fed into your chart.
Another gap: discordance. In one Brazilian study, 33% of patients rated their disease as worse than their doctor did. That doesn’t mean the doctor’s wrong. It means the patient is suffering more than the joints show. That’s when ultrasound helps-seeing real inflammation can validate the patient’s experience.
And then there’s the reverse: patients who feel fine but have high CRP or bone edema. That’s the silent damage. That’s why imaging is non-negotiable for high-risk patients.
What’s Next? AI, Wearables, and Personalized Monitoring
The next five years will change everything.
AI software like DeepJoint can now analyze MRI and ultrasound images with 92% accuracy-matching expert radiologists. That means faster, cheaper readings. Soon, your ultrasound might be interpreted by AI while you wait.
Wearable sensors are being tested in trials like RACoon. These tiny devices track your hand movement, grip strength, and daily activity. If your movement drops by 15% over two weeks, your doctor gets an alert. That’s not science fiction-it’s happening now.
By 2027, experts predict half of RA monitoring will combine clinical scores, imaging, and wearable data. You won’t just go to the clinic every three months. You’ll have a living picture of your disease-updated daily.
But the core won’t change. You still need to measure. You still need to act. The tools just get better.
What You Can Do Today
Don’t wait for your doctor to bring up monitoring. Ask:
- “What’s my CDAI score right now?”
- “Has my DAS28-CRP been checked this year?”
- “Do I need an ultrasound or MRI based on my scores?”
- “Can I use an app to log my symptoms before my visit?”
If your score is above 10 and you’ve been on the same meds for six months, it’s time to talk about changing treatment. Don’t assume you’re doing fine just because you’re not in excruciating pain. The damage is silent until it’s too late.
And if your clinic doesn’t use CDAI or imaging? It’s not standard care. Push for it. You’re not just managing symptoms. You’re protecting your future mobility.
What’s the difference between CDAI and DAS28?
CDAI uses only clinical measures: tender joints, swollen joints, and patient and doctor assessments-all on a 0-10 scale. No blood tests. DAS28 includes those same measures but adds a blood marker (ESR or CRP) to measure inflammation. CDAI is faster and better for routine use. DAS28 catches hidden inflammation but needs lab results.
Which is better: CDAI or DAS28?
For daily clinical use, CDAI is preferred in the U.S. because it’s quick, doesn’t require labs, and strongly predicts joint damage. DAS28 is more sensitive to inflammation and preferred in Europe, but its need for blood work makes it less practical for real-time decisions. Many doctors use both-CDAI for routine visits, DAS28 when they suspect hidden inflammation.
Do I need an MRI for rheumatoid arthritis?
Not usually. MRI is reserved for patients with aggressive disease, rapid progression, or when clinical scores and X-rays don’t match. It’s expensive and not covered by insurance for routine checks. Ultrasound is often the first imaging test because it’s cheaper, faster, and shows active inflammation. MRI is used when doctors need to see bone swelling before erosion appears.
Can ultrasound replace X-rays for monitoring RA?
No. Ultrasound shows active inflammation and early joint changes, but X-rays are still the standard for tracking long-term bone damage. They’re the only tool with decades of historical data used in clinical trials. Ultrasound is better for short-term monitoring; X-rays are essential for long-term assessment. Many clinics use both.
Why do some patients feel worse than their scores suggest?
CDAI and DAS28 don’t measure fatigue, brain fog, or overall quality of life. Some patients have high inflammation or early bone damage that doesn’t yet cause joint swelling. Others have pain that’s neurological or related to other conditions. That’s why patient-reported outcomes and imaging are critical-they help fill the gaps that scores alone can’t see.
How often should I be monitored for RA?
If you’re in remission or low disease activity, check every 6 months. If you’re in moderate or high activity, check every 3 months. X-rays are done at diagnosis and then yearly or every two years. Ultrasound is used when there’s uncertainty or poor response. MRI is only if there’s rapid progression or suspicion of early bone damage.



12 Comments
I had no idea CDAI was that simple. Just count joints and ask how you feel? Makes sense why docs love it.
This is exactly why I started tracking my own symptoms in a notebook before appointments. I was hitting 14 on CDAI but felt like I was just "tired". Turns out my joints were screaming. Now I bring my notes. Game changer.
Also, if your clinic isn't using CDAI regularly, ask why. It's not fancy, but it's the most reliable predictor of damage. Don't let them brush you off.
So DAS28 needs blood work and CDAI doesn’t… but the blood work catches stuff your joints are too polite to tell you about? Classic. Like your body’s whispering secrets and the doc’s like, ‘Wait, did you say CRP or just ‘I’m fine’?’
People think if they’re not in excruciating pain, they’re fine. That’s the lie RA tells you. You’re not fine. You’re just numb from years of being told to ‘push through.’ This post is right-you’re not managing symptoms. You’re delaying destruction.
Just had my first ultrasound last month and honestly? Mind blown. The tech pointed to this red blob on my knuckle and said, 'That’s inflammation you can’t feel yet.' I cried. Not because it hurt-because someone finally saw it. We need more of this. Not just the scores. The visuals.
Also, typo: 'synovium' not 'synovium'... wait, did I just do that? Oops.
If you're on biologics and your CDAI hasn't dropped below 10 in 6 months, you're not doing well-you're just surviving. Time to talk about switching. Don't wait for your joints to crumble. Your future self will thank you.
In Nigeria, we don’t have MRI machines in most clinics. We use what we have: hands, eyes, and the patient’s voice. This post reminded me-no score is a replacement for listening. A woman once told me, 'My fingers don’t hurt, but I can’t hold my baby.' That’s a score no machine can measure. We need tools, yes-but we need hearts more.
I love that we’re moving toward wearables 🙌 My Fitbit already tracks my grip strength. I didn’t even know it could. Now I’m logging fatigue too. If tech can catch what my joints hide, I’m all in. Also, anyone else use RheumaTrack? It’s kinda addictive in a weirdly helpful way 😅
Let’s be real-most doctors still treat RA like it’s 2005. They see a score of 8 and say, 'You’re doing great!' Meanwhile, you can’t open a jar, you’re exhausted, and your knees sound like Rice Krispies. This isn’t management. It’s negligence wrapped in a clipboard. If your doc doesn’t use imaging or push for CDAI every 3 months, find a new one. Your bones aren’t optional.
The paradigm shift from symptom-based to damage-prevention-based care in rheumatology is nothing short of revolutionary. One must recognize that the integration of objective biomarkers, validated clinical indices, and advanced imaging modalities constitutes a triad of evidence-based practice that has demonstrably improved long-term functional outcomes. It is imperative that patients, clinicians, and policymakers alike advocate for the universal adoption of standardized monitoring protocols to mitigate irreversible structural deterioration.
I’ve been in remission for 2 years. CDAI’s been under 2.8. But I still get that foggy, heavy feeling every morning. No one ever asks. I just nod and say 'fine.' Maybe I should start using an app. Or maybe I’m just tired of being told I’m 'doing great' when I’m not.
Wait so you’re saying I need an ultrasound because my CDAI says remission but I still can’t button my shirt? I’m gonna ask my doc next time. Thanks for this. (Typo: ‘synovium’ lol)
Write a comment