Statins & Antifungals Interaction Checker
Check if your statin and antifungal combination is safe. This tool is based on FDA guidelines and medical research on statin-azole interactions.
When you take a statin to lower your cholesterol, you’re not just managing heart health-you’re also putting your muscles at risk if you later need an antifungal. This isn’t a rare edge case. It’s a well-documented, dangerous interaction that sends people to the hospital every year. The problem? Certain antifungal drugs, especially azoles like itraconazole and fluconazole, can turn normally safe statins into muscle-destroying toxins. The result? rhabdomyolysis-a condition where muscle cells break down, leak into the bloodstream, and can shut down your kidneys.
How Statins and Antifungals Collide
Statins work by blocking an enzyme in your liver that makes cholesterol. But your body doesn’t just clear them out on its own. Most statins are broken down by a group of liver enzymes called CYP3A4. That’s where antifungals come in. Azole antifungals-used for everything from athlete’s foot to yeast infections-are powerful inhibitors of CYP3A4. Think of it like jamming a lock. When these drugs block CYP3A4, statins can’t be processed. They build up in your blood. And when they get too high, they start attacking muscle tissue.This isn’t theoretical. In 2012, the FDA updated its warnings after reviewing hundreds of cases. They found that combining simvastatin with itraconazole could spike simvastatin levels by more than 10 times. That’s not a typo. Ten times. And at those levels, muscle damage isn’t just possible-it’s likely.
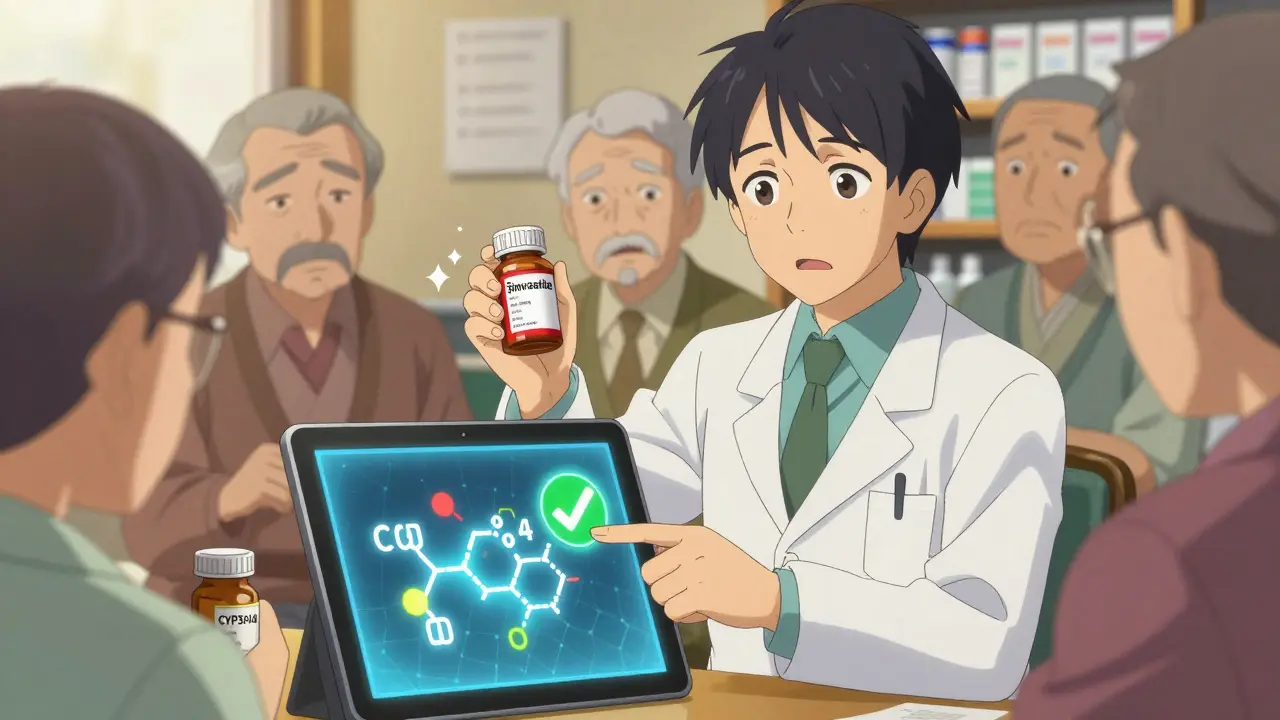
Not All Statins Are Created Equal
Some statins are far more dangerous than others when mixed with antifungals. It comes down to how they’re metabolized.- High-risk statins: Simvastatin, lovastatin, atorvastatin. These rely heavily on CYP3A4. Simvastatin is the worst offender. Even a low dose of 20 mg can become toxic when paired with itraconazole.
- Lower-risk statins: Pravastatin, fluvastatin, rosuvastatin, pitavastatin. These use other enzymes or are cleared mostly unchanged. That makes them much safer choices if you need an antifungal.
A 2023 study in Frontiers in Pharmacology showed that voriconazole increased atorvastatin levels by 3.5 to 5.2 times. But pravastatin? No meaningful change. That’s why doctors now recommend switching statins-not just lowering the dose-when antifungals are needed.
Which Antifungals Are the Worst?
Not all antifungals are the same. Their strength as CYP3A4 inhibitors varies wildly.- Strongest inhibitors: Ketoconazole, itraconazole, voriconazole. These are the ones the FDA explicitly warns against. Ketoconazole is so potent it’s no longer used orally in the U.S. for this reason. Itraconazole? It’s still common for fungal nail infections. Voriconazole? Used in serious hospital infections.
- Moderate inhibitor: Fluconazole. This one trips people up because it’s so common. Used for yeast infections, oral thrush, even prevention in immunocompromised patients. At 200 mg daily or higher, it can still raise simvastatin levels by 350%. That’s enough to trigger rhabdomyolysis.
- Safer option: Isavuconazole. Approved in 2015, it barely touches CYP3A4. If you need long-term antifungal therapy, this is the one to ask about.
Here’s what the numbers look like:
| Statin | Antifungal | AUC Increase | Risk Level |
|---|---|---|---|
| Simvastatin | Itraconazole | 1,160% | Extreme |
| Lovastatin | Itraconazole | 1,550% | Extreme |
| Simvastatin | Fluconazole (400 mg/day) | 350% | High |
| Atorvastatin | Fluconazole (400 mg/day) | 80% | Moderate |
| Pravastatin | Any azole | <10% | Low |
| Rosuvastatin | Any azole | <10% | Low |
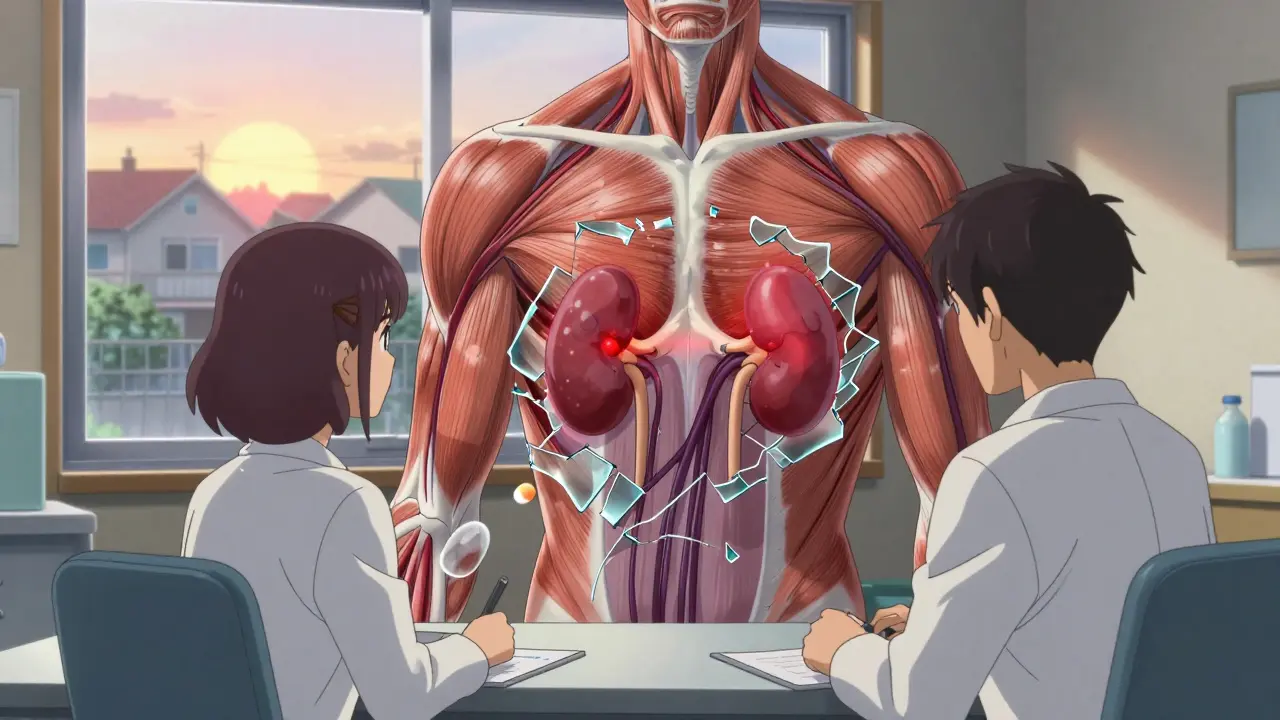
What Happens When Muscle Breaks Down
Rhabdomyolysis doesn’t sneak up. It hits hard and fast. Symptoms usually show up within 7 to 14 days after starting the antifungal. You’ll feel it.- Severe muscle pain: Not soreness from the gym. This is deep, constant, and doesn’t go away. Often in the thighs, shoulders, or lower back.
- Weakness: So much that climbing stairs or lifting your arm feels impossible.
- Dark urine: Think cola-colored. That’s myoglobin leaking from dead muscle cells. It’s a red flag for kidney damage.
One 2018 case report described a 68-year-old man on simvastatin 40 mg who developed rhabdomyolysis after 7 days of fluconazole 200 mg daily. His creatine kinase (CK) level hit 18,400 U/L. Normal is 30-200. He spent three days in the hospital. He wasn’t even elderly or overweight. Just unlucky with a drug combo.
Real-World Data: It’s Happening More Than You Think
The FDA’s adverse event database recorded 1,247 cases of rhabdomyolysis tied to statin-azole combinations between 2010 and 2019. Simvastatin with itraconazole made up nearly 40% of those. Simvastatin with fluconazole? Almost 30%. And here’s the kicker: a 2022 study in JAMA Internal Medicine found that 18.7% of patients still got these dangerous combinations. That’s nearly 1 in 5. Elderly patients? Over 23%.Why? Because many doctors don’t realize fluconazole-even at 100 mg-is risky. Or patients don’t tell their doctor they’re taking an antifungal for a yeast infection. Pharmacists in community pharmacies report seeing 2-3 cases per year. Most are in people over 65, with kidney issues or on multiple meds.
What Should You Do?
If you’re on a statin and need an antifungal, don’t guess. Ask. Here’s what works:- Stop simvastatin or lovastatin completely. Don’t lower the dose. Stop it. Restart only 2-3 days after the antifungal ends.
- Switch to a safer statin. Pravastatin 40 mg, fluvastatin 80 mg, or rosuvastatin 20 mg are safe with all azoles. No dose adjustments needed.
- If you must use atorvastatin, limit it to 20 mg daily with fluconazole. Avoid itraconazole or voriconazole entirely.
- Ask about isavuconazole. If you need long-term antifungal treatment, this is the best alternative.
- Get a CK test before starting. Baseline levels help track changes. Monitor weekly during treatment.
- Know the warning signs. Muscle pain + dark urine = stop the meds and go to urgent care.
The Bigger Picture: Why This Keeps Happening
You might think this is just a “medication error.” But it’s more than that. It’s a system failure. EHRs like Epic now have hard stops-they won’t let you prescribe simvastatin over 20 mg with itraconazole. One study showed this cut dangerous prescriptions by 87%. But outside hospitals, in outpatient clinics, the warnings are still missed.Why? Because antifungals are often prescribed for short-term issues. A vaginal yeast infection. A fungal nail infection. Patients don’t think to mention it. Doctors don’t think to check. And statins? They’ve been taken for decades. It feels routine.
But routine doesn’t mean safe. A 2023 review in the Journal of Antimicrobial Chemotherapy found that even “low-risk” combinations like fluconazole and simvastatin can push CK levels over 10,000 U/L. That’s enough to cause kidney failure.
What’s Next?
Researchers are looking at genetics. Some people have a variant in the CYP3A5 gene that makes them poor metabolizers. If you have this, even low doses of statins with antifungals can be dangerous. Testing for this isn’t routine yet-but it might be soon.The American College of Cardiology and Infectious Diseases Society of America are working on new guidelines for 2024. They’ll include algorithms based on age, kidney function, and other meds. That’s a good sign. But until then, the safest move is simple: know your statin. Know your antifungal. And never assume it’s safe.
If you’re on simvastatin and your doctor prescribes fluconazole, ask: “Can we switch my statin instead?” You might be surprised how often the answer is yes-and how much safer it makes you.
Can I take fluconazole with my statin?
It depends on which statin you’re taking. Fluconazole can be used with pravastatin, fluvastatin, rosuvastatin, or pitavastatin without major risk. But if you’re on simvastatin or lovastatin, even low doses of fluconazole can raise your risk of rhabdomyolysis. If you’re on atorvastatin, keep the dose under 20 mg daily. Always check with your doctor before combining them.
Is it safe to take simvastatin with itraconazole?
No. The FDA explicitly contraindicates this combination. Itraconazole increases simvastatin levels by over 10 times, which can cause severe muscle damage and kidney failure. This combination should never be prescribed. If you’re on simvastatin and need an antifungal, switch statins or delay the antifungal until you’re off the statin.
What are the signs of rhabdomyolysis?
The main signs are severe muscle pain (not typical soreness), weakness, and dark, cola-colored urine. These usually appear 7-14 days after starting the antifungal. If you experience these symptoms, stop the medications and seek medical care immediately. High creatine kinase levels and kidney damage can follow quickly.
Which statin is safest with antifungals?
Pravastatin, fluvastatin, and rosuvastatin are the safest choices. They’re not significantly affected by CYP3A4 inhibitors like azole antifungals. Pravastatin is often the go-to replacement because it’s well-studied, effective, and has minimal drug interactions. Your doctor can switch you without losing cholesterol control.
Can I take a lower dose of simvastatin with fluconazole?
The FDA recommends no more than 10 mg of simvastatin daily with fluconazole. But even that carries risk-especially in older adults or those with kidney issues. Most experts now advise switching to a different statin entirely instead of trying to manage a risky combination. Safety outweighs convenience.