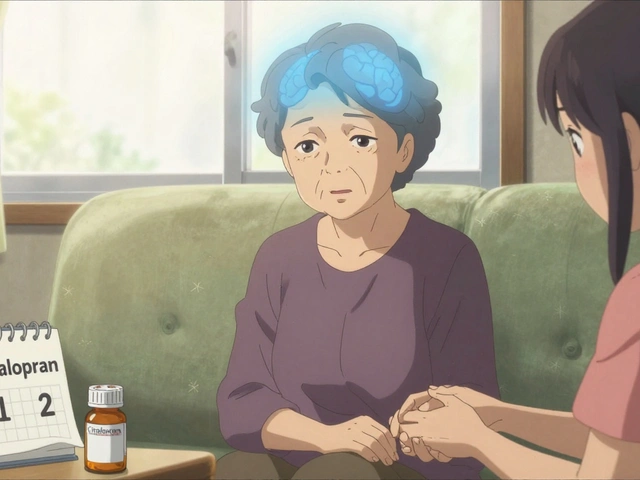
Escitalopram: What It Is, How to Take It, and What to Watch For
If you’ve been told to start escitalopram, you probably wonder what the pill does and whether it’s safe. In plain English, escitalopram is a prescription drug that belongs to the SSRI family – short for selective serotonin reuptake inhibitor. It lifts mood by keeping more serotonin, a natural brain chemical, hanging around longer.
Doctors usually prescribe escitalopram for major depression, generalized anxiety disorder, and sometimes panic attacks. It can also help with social anxiety or obsessive‑compulsive symptoms, but that’s decided case by case. The good news is that many people feel better within a few weeks, though the full effect can take up to 6‑8 weeks.
How Escitalopram Works & When It’s Prescribed
Serotonin helps regulate mood, sleep, and appetite. Escitalopram blocks the re‑absorption (reuptake) of serotonin at nerve cells, so more of it stays active in the brain. This boost can smooth out the emotional roller coaster that comes with depression or anxiety.
Typical starting doses are 10 mg once daily for adults, taken in the morning or evening with or without food. If your doctor thinks you need more, they may raise it to 20 mg after a week or two. Kids and teens get lower doses, and doctors tailor the amount based on weight, other meds, and how you respond.
Don’t stop the pill abruptly. Cutting it off too fast can cause withdrawal‑type symptoms like dizziness, “brain zaps,” or mood swings. If you need to quit, your doctor will likely drop the dose slowly over a few weeks.
Practical Tips for Using Escitalopram Safely
Keep a pill calendar or set a daily alarm – consistency matters. If you miss a dose, take it as soon as you remember unless it’s almost time for the next one; then just skip the missed one.
Watch for side effects in the first two weeks. Common ones include mild nausea, headache, dry mouth, or a bit of sleepy‑ness. Most fade as your body gets used to the drug. If you notice anything severe – like fast heartbeat, severe stomach pain, or any thoughts of self‑harm – call your doctor right away.
Escitalopram can interact with a bunch of other meds, especially other antidepressants, certain pain relievers, and some migraine drugs. Always hand your pharmacist a full list of what you’re taking, including over‑the‑counter supplements.
Alcohol isn’t a good mix. It can increase drowsiness and make side effects feel worse. If you enjoy a drink now and then, talk to your prescriber about what’s safe for you.
When you’re shopping online, look for licensed pharmacies that require a prescription, show clear contact info, and have a pharmacist available for questions. Cheap, no‑prescription sites often sell counterfeit pills that can be dangerous.
Finally, give the medication time. Many people feel a noticeable lift after 2‑3 weeks, but patience is key. Pairing escitalopram with therapy, regular exercise, and good sleep can speed up recovery.
Bottom line: escitalopram is a well‑studied antidepressant that works for many people with depression and anxiety. Take it exactly as your doctor advises, monitor how you feel, and stay in touch with your healthcare team. With the right approach, you’ll give yourself a solid chance at feeling better.

Escitalopram and Blood Sugar: Unraveling the Link with Sugar Cravings
- By : Archer Hamilton
- Date : May 21 2025
Does escitalopram (Lexapro) mess with your blood sugar and spark cravings for sweets and carbs? This article dives into the latest small studies and reviews, exploring how SSRIs might nudge your glucose levels and influence what you reach for in the fridge. Expect real data, clear tips, and some surprise links between your mood meds and what’s on your plate.