When your immune system turns on your own body, things get messy. Instead of fighting off germs, it starts attacking your joints, skin, gut, or even your spine. That’s what happens in autoimmune diseases like rheumatoid arthritis, psoriatic arthritis, Crohn’s disease, and ankylosing spondylitis. For decades, treatment meant managing pain with pills that barely touched the root cause. Then came TNF inhibitors - a new kind of medicine that doesn’t just mask symptoms. It cuts off the signal that’s making your body destroy itself.
What Exactly Is TNF?
TNF stands for tumor necrosis factor - specifically, TNF-alpha. It’s not a villain by design. Your body makes it to help fight infections and heal wounds. But in autoimmune diseases, too much TNF-alpha gets produced, and it never turns off. Think of it like a fire alarm stuck on blast mode, screaming even when there’s no fire. This constant signal pulls in immune cells, triggers inflammation, and slowly tears apart your tissues.
Scientists discovered TNF-alpha sits right at the top of the inflammation chain. Block it, and you knock down most of the other inflammatory signals too - like IL-1, IL-6, and chemokines that draw more troublemakers to the scene. That’s why targeting TNF became such a big deal. It’s not just one piece of the puzzle. It’s the whole box.
The Five TNF Inhibitors You Need to Know
The FDA has approved five TNF inhibitors for autoimmune conditions. They all do the same basic job - block TNF-alpha - but they’re built differently, which changes how they work and how you take them.
- Etanercept (Enbrel): This one’s a fusion protein - basically, it’s a decoy receptor. It mimics the part of your immune cell that TNF normally binds to, so TNF latches onto it instead. It’s injected under the skin, usually once or twice a week.
- Infliximab (Remicade): A monoclonal antibody given through an IV infusion. You sit in a clinic for about two hours every 4 to 8 weeks. It binds to both free and cell-bound TNF, and it can trigger immune cells to kill off inflamed tissue.
- Adalimumab (Humira): Another monoclonal antibody, but it’s injected under the skin every other week. It’s one of the most widely used TNF inhibitors globally.
- Golimumab (Simponi): Also a monoclonal antibody, injected once a month. It’s often chosen for patients who want less frequent dosing.
- Certolizumab pegol (Cimzia): This is unique. It’s a fragment of an antibody, not a full one, and it’s attached to polyethylene glycol (PEG). That means it lasts longer in your body and doesn’t trigger certain immune reactions. It only targets free-floating TNF, not the kind stuck to cells.
These differences matter. For example, the full antibodies (infliximab, adalimumab, golimumab) can cause what’s called antibody-dependent cell-mediated cytotoxicity (ADCC). That means they don’t just block TNF - they help your immune system destroy cells that are producing it. Etanercept doesn’t do that. It just soaks up the excess TNF like a sponge.
How TNF Inhibitors Actually Work (Beyond Just Blocking)
It’s not as simple as turning off a switch. TNF inhibitors do more than just stop TNF from binding to its receptors (TNFR1 and TNFR2). They also change how immune cells behave.
For one, they can trigger apoptosis - programmed cell death - in overactive immune cells. This helps clear out the troublemakers driving inflammation. They also reduce the stickiness of blood vessel walls, meaning fewer immune cells can sneak into joints or the gut lining to cause damage.
There’s even evidence they lower levels of oxidative stress and other inflammatory markers beyond TNF. In people with rheumatoid arthritis, studies show TNF inhibitors can reduce C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) - blood tests that measure inflammation - by 50% or more within weeks.
And here’s the twist: TNF isn’t just bad. It also helps control infections and even keeps some tumors in check. That’s why blocking it comes with risks. But the body has two TNF receptors: TNFR1 and TNFR2. TNFR1 drives inflammation and cell death. TNFR2 helps regulate immune responses and may even protect tissues. Some new research is looking at drugs that block only TNFR1 - hoping to keep the good while stopping the bad.
Who Gets These Drugs - And When?
TNF inhibitors aren’t your first-line treatment. Doctors usually try conventional drugs like methotrexate or sulfasalazine first. These are called DMARDs - disease-modifying antirheumatic drugs. They’re cheaper and have been around for decades. But they often don’t stop joint damage.
If you’ve tried at least one DMARD and still have active disease - swollen joints, persistent fatigue, ongoing gut flare-ups - then TNF inhibitors become an option. They’re not magic. But they work better than DMARDs alone. In rheumatoid arthritis, about 50-60% of patients see major improvement with TNF inhibitors, compared to 20-30% with DMARDs alone.
Before starting, you’ll need a TB test. TNF inhibitors can wake up dormant tuberculosis. You’ll also get screened for hepatitis B and other infections. If you’ve had cancer, especially lymphoma, your doctor will be extra cautious.
Side Effects and Risks - The Real Talk
Yes, these drugs work. But they come with trade-offs.
The biggest risk? Infections. You’re 2 to 5 times more likely to get serious ones - like pneumonia, sepsis, or fungal infections. Reactivation of latent TB happens in 4 to 7 times more people on TNF inhibitors than in the general population. That’s why screening is non-negotiable.
Injection site reactions are common - redness, itching, swelling - affecting 20-30% of people using subcutaneous versions. Most fade after a few doses, but some people never get used to them.
Then there’s the long-term issue: secondary failure. About 30-40% of patients find that after months or years, the drug stops working. Why? Their immune system starts making antibodies against the drug itself. It’s like your body sees the medicine as an invader and kicks it out. That’s more common with infliximab and adalimumab than with etanercept.
And then there’s the paradox. In rare cases, TNF inhibitors cause new inflammatory problems - like multiple sclerosis-like symptoms, lupus-like rashes, or even nerve damage. Scientists think this might happen because TNF inhibitors can’t cross the blood-brain barrier. So while they calm inflammation in your joints, they might cause an imbalance in your brain or spinal cord, triggering immune cells to go rogue.

What Patients Really Experience
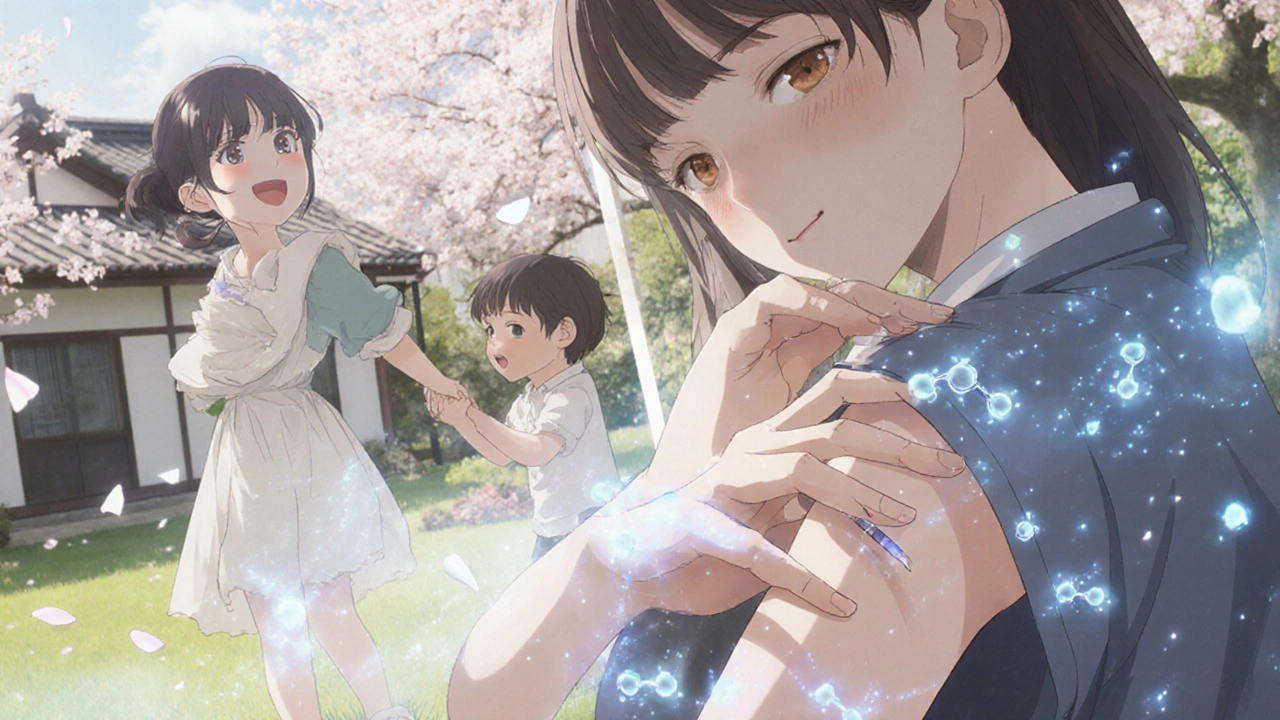
Real people don’t talk about cytokine pathways. They talk about walking again.
One woman with rheumatoid arthritis told her doctor she hadn’t been able to pick up her toddler in over a year. After six months on adalimumab, she was playing tag with him in the backyard. Another man with Crohn’s disease, who’d spent years in and out of hospitals, went from 15 bowel movements a day to two - and finally ate a burger without fear.
But it’s not all wins. Many patients dread the injections. Some feel guilty for being on a drug that costs thousands a month. Others are scared of getting sick. Reddit threads and patient forums are full of stories about insurance battles, missed work for infusions, and the loneliness of chronic illness.
Support programs from drugmakers - like Humira Complete or Inflectra Connect - help with training, co-pays, and 24/7 nurse lines. But not everyone knows they exist.
The Future: Biosimilars and Beyond
When Humira’s patent expired, biosimilars flooded the market. These aren’t generics. They’re highly similar versions made by other companies after the original drug’s patent expires. Amjevita (adalimumab biosimilar), Cyltezo, and others now make up nearly a quarter of the U.S. market for adalimumab.
Biosimilars have cut costs - sometimes by 30-50%. That means more people can access treatment. But they don’t change how the drugs work. The same risks, same side effects, same effectiveness.
Looking ahead, newer biologics targeting IL-17 and IL-23 are gaining ground, especially for psoriasis and psoriatic arthritis. They’re more targeted, and in some cases, more effective. But TNF inhibitors still lead for rheumatoid arthritis and Crohn’s disease.
Research is now focused on smarter versions - drugs that block only TNFR1, or ones that can cross the blood-brain barrier safely. The goal isn’t just to suppress inflammation. It’s to restore balance without breaking the rest of the immune system.
Is It Right for You?
TNF inhibitors aren’t for everyone. But for those who’ve tried everything else and still suffer - they can be life-changing.
If you’re dealing with persistent joint pain, unexplained fatigue, gut flares, or skin plaques that won’t quit - and your doctor says you’re a candidate - ask about TNF inhibitors. Ask about the risks. Ask about biosimilars. Ask what support is available.
They’re not a cure. But they’re one of the few tools we have that actually change the course of autoimmune disease - not just the symptoms. And for many, that’s enough to get back to living.
How long does it take for TNF inhibitors to work?
Most people start noticing improvements in 4 to 8 weeks, but full benefits can take 3 to 6 months. Some feel better sooner - especially in skin or gut symptoms. Joint pain and stiffness often improve more slowly. If there’s no change after 12 weeks, your doctor may switch you to another drug.
Can I stop taking TNF inhibitors if I feel better?
Stopping usually leads to a flare-up. Even if you’re in remission, the disease is still there, just quiet. Most doctors recommend staying on the medication long-term. In rare cases, after years of stable remission, some patients may try to taper off under close supervision - but this isn’t common and carries high risk of relapse.
Do TNF inhibitors cause weight gain?
Not directly. But some people gain weight because they’re finally able to move again - eating more, being more active, or taking steroids alongside the TNF inhibitor. Others lose weight due to improved gut function in Crohn’s patients. Weight changes are usually tied to overall health improvement, not the drug itself.
Are TNF inhibitors safe during pregnancy?
Etanercept and adalimumab are considered low-risk during pregnancy and are often continued to prevent disease flares, which can be more dangerous than the drug. Certolizumab pegol is the only TNF inhibitor that doesn’t cross the placenta significantly, making it the preferred choice for pregnant women. Always consult your rheumatologist or OB-GYN before making changes.
Can I get vaccines while on TNF inhibitors?
Yes - but only non-live vaccines. Flu shots, pneumonia shots, and COVID boosters are safe and recommended. Avoid live vaccines like MMR, varicella, or the nasal flu spray. Get all necessary vaccines before starting TNF inhibitors if possible. Your doctor will help you plan timing.






14 Comments
Wow. This is one of the clearest explanations I’ve ever read.
Thank you.
I’ve been on Humira for five years. The first six months were rough-injections every other week, anxiety about infections, insurance fights-but now I can carry my daughter without wincing. It’s not perfect, but it’s the best thing that’s happened to my body in a decade.
Let’s be real-TNF inhibitors are overhyped. Yes, they work for some, but the data is messy. The infection risk? Underreported. The secondary failure rate? Often ignored. And don’t even get me started on the cost-$20,000 a year for a drug that makes your body a sitting duck for fungi and TB? That’s not medicine-it’s a gamble with your life. And biosimilars? They’re not identical, but regulators pretend they are. The FDA’s approval process is a joke.
Meanwhile, real science is moving toward TNFR1-specific blockers. But no one’s funding that because Big Pharma makes more money selling the same old drug under a new name.
OMG I JUST GOT MY FIRST INJECTION AND MY ARM IS ON FIRE?? IS THIS NORMAL?? I’M SO SCARED
Hey, I know how scary this can feel-especially when you’re new to it. That burning sensation? Totally normal. It fades after a few doses. I used to cry after every injection, too. But now? I can play with my niece without pain. You’re not alone. And if you need someone to talk to about the fear or the cost or the weird side effects-I’ve been there. DM me. Seriously. You got this.
Oh, so now we’re just gonna hand out biologics like candy? Who gave you the right to decide who gets to live? I’ve got a cousin who got sepsis from Humira. Died at 34. And you’re out here acting like this is some miracle cure? Wake up. This isn’t science-it’s corporate greed dressed up as hope. And don’t even get me started on how they market this to desperate people. It’s disgusting.
Meanwhile, real healers-herbs, fasting, gut protocols-are being silenced. But hey, let’s just keep injecting poison and calling it progress.
I’m curious-how do you know if you’re one of the 50-60% who respond well? Is there a biomarker? Or is it just trial and error? I’ve been on methotrexate for two years and still can’t open a jar. I’m scared to start something stronger… but I’m also tired of living like this.
I just want to say how much I appreciate how thorough this is-it’s rare to see a post that doesn’t just skim the surface. I’ve been living with Crohn’s for 18 years, and I’ve tried everything: steroids, immunomodulators, even a colectomy that didn’t stick. When I started Cimzia, I didn’t expect to feel better so fast-but within three weeks, the diarrhea stopped, the fatigue lifted, and I actually started enjoying food again. It’s not perfect-I still get the occasional flare, and I hate the monthly shots-but it’s given me back something I thought I’d lost forever: normalcy. And I know that sounds cheesy, but it’s true. This isn’t just about inflammation-it’s about being able to sit at a dinner table without planning your bathroom route.
While I appreciate the effort put forth in this document, it is gravely deficient in its adherence to evidence-based medicine standards. The assertion that TNF inhibitors "change the course of autoimmune disease" is not substantiated by longitudinal, double-blind, placebo-controlled trials with sufficient power. Furthermore, the omission of any discussion regarding the role of epigenetics, microbiome dysbiosis, and environmental triggers in autoimmune pathogenesis renders this piece dangerously reductive. The FDA’s approval process is not infallible, and the promotion of biologics as first-line alternatives to lifestyle intervention constitutes a systemic failure in medical education. I urge you to consult the Cochrane reviews before disseminating such misleading information.
One thing the post doesn’t clarify: TNF-alpha isn’t just a cytokine-it’s a pleiotropic mediator with context-dependent roles. In early disease, it may be pro-inflammatory; in chronic phases, it can help maintain tissue integrity. That’s why blocking it broadly causes side effects. The real frontier is spatial targeting-delivering inhibitors only to inflamed joints or gut mucosa, not systemically. That’s where the next-gen drugs are headed. And yes, TNFR1-selective blockers are in Phase II. If they work, we might finally get efficacy without immunosuppression.
Bro. I was in a wheelchair for six months. Couldn’t walk. Couldn’t sleep. My wife cried every night. Then I got adalimumab. Six weeks later? I did my first push-up in 10 years. I cried. My dog cried. My neighbor cried. Now I’m hiking every weekend. Yeah, I get infections. Yeah, I’m scared. Yeah, I pay $500 a month even with insurance. But I’d take that pain every day if it meant I could hold my kid again. This ain’t just medicine-it’s a second chance. Don’t let fear steal that from you.
There’s something deeper here than just biology. When your body turns against you, you lose not just function-but identity. You become a patient. A problem. A cost center. TNF inhibitors don’t just block a protein-they restore dignity. The woman who picked up her toddler? She didn’t just regain mobility. She reclaimed motherhood. The man who ate a burger? He got back joy. This isn’t about cytokines. It’s about remembering what it means to be human. And if that’s not worth fighting for-I don’t know what is.
Let’s be honest-this whole TNF thing is just a Band-Aid on a bullet wound. We’re patching inflammation while ignoring the root causes: processed food, chronic stress, glyphosate, endocrine disruptors, the whole damn industrialized world. And instead of fixing that, we pump people full of $20k/year biologics and call it a win? It’s like giving someone a new tire while their car is on fire. The real solution isn’t blocking TNF-it’s fixing the system that made them sick in the first place. But hey, Big Pharma loves a recurring revenue stream.
Also, why is no one talking about how these drugs make you emotionally numb? I felt like a zombie for months. Like I was watching my life through glass. That’s not healing. That’s suppression.
So now we’re giving American taxpayers’ money to fund foreign drug companies to treat people who won’t take responsibility for their own health? I’ve seen this before-Europeans come here, get biologics, then go home and complain about U.S. healthcare costs. We’re subsidizing global medical tourism. And for what? So people can go back to eating sugar and sitting on couches? This isn’t healthcare. It’s a national disgrace.
Write a comment