Medication QT Risk Checker
How This Tool Works
This tool helps you assess your risk of QT prolongation based on medications you're taking. QT prolongation can increase your risk of dangerous heart rhythms. Enter your medications and, if available, your QT interval measurement to get a risk assessment.
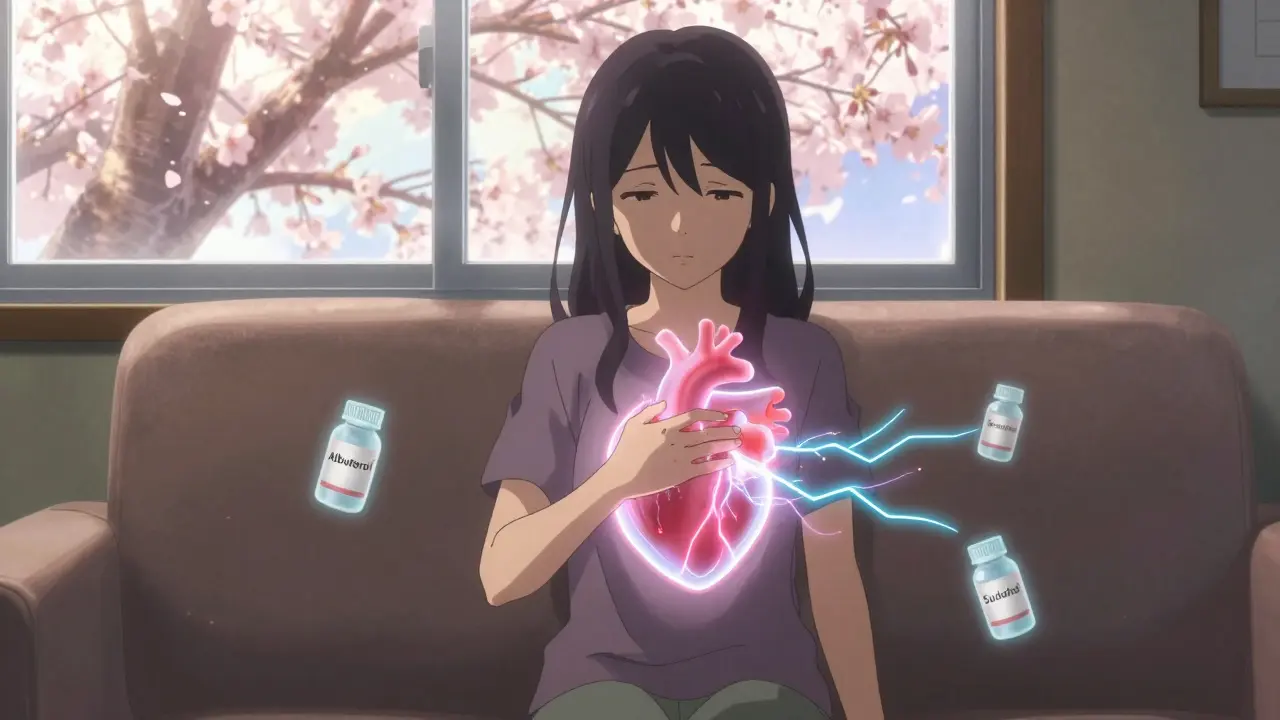
Medication-induced palpitations are more common than most people realize. You take a pill for your asthma, an antibiotic for an infection, or even an over-the-counter cold remedy-and suddenly your heart feels like it’s pounding out of your chest. It’s not just anxiety. It’s not just caffeine. It’s the medicine itself. And while many cases are harmless, some can lead to serious, even life-threatening heart rhythms if ignored.
How Medications Throw Your Heart Off Balance
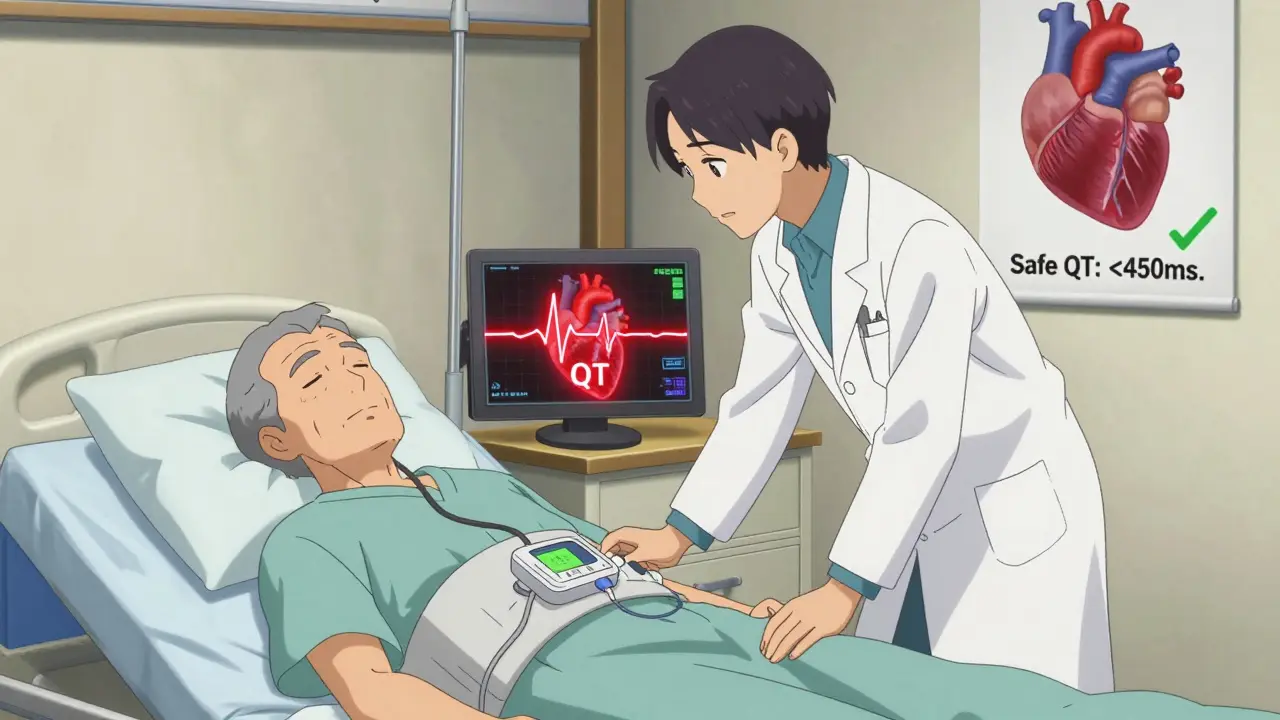
Your heart doesn’t just beat randomly. It follows a precise electrical signal that tells each chamber when to contract. Certain medications interfere with this signal, especially by prolonging the QT interval-the time it takes for the heart to recharge between beats. When this interval gets too long, it can trigger a dangerous rhythm called torsades de pointes. This isn’t rare. According to the American Heart Association, about 1 in 5 arrhythmia cases seen in clinics are linked directly to medications. Some drugs speed up your heart rate. Others make it irregular. And a few do both. The effect isn’t always immediate. You might feel fine for days after starting a new pill, then suddenly notice your heart fluttering while you’re walking to the mailbox. That delay is why so many people miss the connection.Top Medications That Trigger Palpitations
Not all drugs are created equal when it comes to heart risks. Here are the most common culprits, backed by clinical data:- Beta-2 agonists (asthma inhalers) - Albuterol (salbutamol) can raise your heart rate by 15-25 beats per minute within half an hour. If you’re using it multiple times a day, that’s constant stress on your heart. Salmeterol, the long-acting version, keeps it elevated for up to 12 hours.
- Antibiotics - Azithromycin (Zithromax) is one of the worst offenders. A 2021 study of over 1.2 million patients found it increases the risk of rapid heartbeat by more than double. Levofloxacin and ciprofloxacin also prolong the QT interval, though less severely.
- Decongestants - Pseudoephedrine (Sudafed) at 60mg can spike your heart rate by 10-20 bpm. Phenylephrine is slightly safer, but still risky if you’re older or have high blood pressure.
- Thyroid meds - Levothyroxine (Synthroid) is essential for many, but if your dose is too high-especially when TSH drops below 0.1 mIU/L-you’ll likely feel your heartbeat in your throat. About 1 in 10 users report palpitations.
- Antidepressants - Amitriptyline (a tricyclic) can stretch the QT interval by 40-60 milliseconds. Even SSRIs like citalopram carry risk, especially at doses over 40mg/day. Sertraline, by contrast, has a much lower profile.
- Newer weight-loss drugs - Semaglutide (Ozempic, Wegovy) wasn’t originally known for this, but clinical trials show a consistent 3-5 bpm increase in heart rate, even at standard doses.
What Doctors Look For: The Evaluation Process
If you’re reporting palpitations, your doctor shouldn’t just shrug and say, “It’s probably nothing.” A proper evaluation includes four key steps:- Complete medication review - Every pill, supplement, and OTC drug you take. Many patients forget herbal teas, energy powders, or sleep aids. That’s often where the trigger hides.
- ECG (electrocardiogram) - This measures your QT interval. Normal is under 450ms for men, under 460ms for women. If it’s over 500ms, or has jumped more than 60ms from a previous test, you’re in high-risk territory.
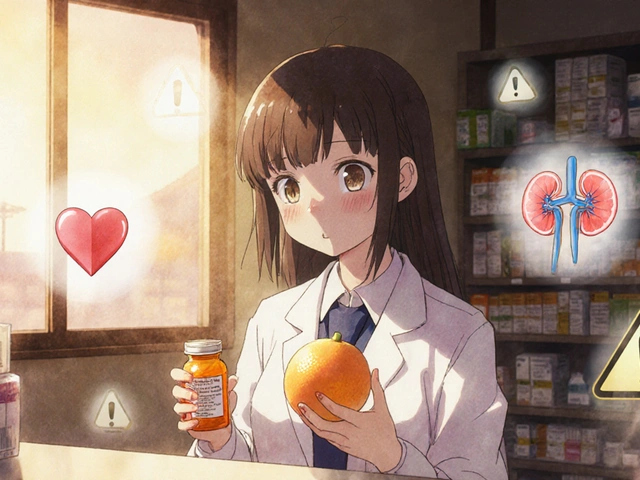
- Blood tests - Low potassium (<3.5 mmol/L) or magnesium (<1.7 mg/dL) makes your heart far more vulnerable. Thyroid levels (TSH) must also be checked.
- Holter monitor - If your ECG looks normal but symptoms persist, a 24-48 hour portable monitor catches intermittent rhythms that a single snapshot misses. It finds problems in 35-45% of cases where the initial test was clean.
How to Manage It: From Mild to Critical
The approach depends on how bad things are:- Mild cases - If your QT interval is under 500ms and you’re not dizzy or fainting, your doctor might keep the medication but monitor you closely. Weekly ECGs, checking electrolytes, and cutting caffeine or alcohol can help.
- Moderate cases - If you’re having symptoms and your QT is between 480-500ms, reducing the dose often works. Mayo Clinic data shows 60-70% of patients feel better within 72 hours of a dose drop.
- High-risk cases - QT over 500ms, torsades de pointes, or fainting? Stop the drug immediately. No exceptions. Hospitals follow strict protocols for this. The risk of sudden cardiac arrest is real.
Switching medications is often the solution. For example, if you need an antibiotic and have heart risks, amoxicillin is a far safer choice than azithromycin. Studies show it causes arrhythmias in only 0.8% of patients versus 2.9% for azithromycin. For thyroid patients, keeping TSH between 0.5 and 2.0 mIU/L cuts palpitations from 12% down to just 4.3%.
Prevention Is the Best Treatment
The most effective strategy isn’t fixing the problem after it starts-it’s stopping it before it begins.- Ask for a baseline ECG before starting any new medication known to affect the heart.
- Keep a simple log: note when you take each drug and when you feel palpitations. Over time, patterns emerge.
- Never combine two QT-prolonging drugs. Doing so increases risk by nearly sixfold.
- Older adults (over 75) are 3.2 times more likely to develop dangerous rhythms from these drugs. Extra caution is non-negotiable.
Electronic health systems are catching on. Hospitals using real-time alerts (like Epic’s QTc Monitor) block over 8,500 risky prescriptions every month. These aren’t just fancy tools-they’re saving lives.
Real Stories Behind the Numbers
Reddit users describe it as “a fluttering under the ribs that won’t quit.” One woman on Patient.info said she woke up every morning with her heart pounding-until her doctor lowered her levothyroxine dose. Another man on Drugs.com, who took Sudafed daily for allergies, stopped after his heart rate hit 130 bpm. His symptoms vanished in two days.A 68-year-old woman in a MyHeartCommunity.org case study switched from citalopram to sertraline. Her palpitations disappeared within 10 days. She didn’t lose her mood stability. She just got her heart back.
What You Should Do Now
If you’re on any of these medications and feel your heart racing, skipping, or pounding:- Don’t panic-but don’t ignore it.
- Write down every medication, supplement, and OTC product you take.
- Check if you’ve had an ECG recently. If not, ask for one.
- Ask your doctor: “Could this medication be causing my palpitations?”
- If you’re over 65, have heart disease, or take multiple meds, request a medication review.
You’re not overreacting. You’re being smart. Medications save lives-but they can also strain your heart. Knowing which ones do both is the first step to staying safe.
Can over-the-counter cold medicines cause palpitations?
Yes. Pseudoephedrine (in Sudafed) and phenylephrine (in many store-brand cold remedies) can increase heart rate by 10-20 beats per minute. The risk goes up with higher doses, older age, or existing heart conditions. Even one tablet can trigger symptoms in sensitive people. Always check labels and talk to your pharmacist before taking decongestants if you have heart issues.
Is a rapid heartbeat from medication always dangerous?
Not always. Many people experience mild, temporary palpitations without any long-term risk. But if it’s new, persistent, or accompanied by dizziness, chest pain, or fainting, it’s not harmless. The real danger comes when the heart rhythm shifts into something like torsades de pointes-a type of ventricular tachycardia that can turn fatal within minutes if not treated. That’s why even small symptoms deserve evaluation.
How long do medication-induced palpitations last?
It depends on the drug. For short-acting meds like albuterol or pseudoephedrine, symptoms often fade within hours after stopping. For drugs that build up in your system-like azithromycin or antidepressants-it can take days to weeks for the heart to return to normal. In some cases, especially with QT prolongation, the electrical changes linger longer. Monitoring with follow-up ECGs is key to knowing when it’s safe.
Can I still take my thyroid medicine if it causes palpitations?
Yes-but only if you adjust the dose. Levothyroxine is essential for many, but too much triggers palpitations. The fix isn’t stopping it-it’s lowering the dose until your TSH level is between 0.5 and 2.0 mIU/L. Studies show this cuts palpitations from 12% of users down to under 5%. Always get your TSH checked every 4-6 weeks after a dose change.
Are there safer alternatives to azithromycin for infections?
Absolutely. Amoxicillin is a top choice-it has less than half the arrhythmia risk of azithromycin. Doxycycline and cephalexin are also low-risk options for many common infections. If you have a history of heart problems, ask your doctor to avoid macrolides (azithromycin, clarithromycin) and fluoroquinolones (levofloxacin, ciprofloxacin) unless absolutely necessary.
Can I prevent medication-induced palpitations before they start?
Yes. Ask for a baseline ECG before starting any new medication known to affect the heart. Get your potassium and magnesium levels checked. Avoid combining multiple QT-prolonging drugs. Keep a symptom journal. And if you’re over 65 or have heart disease, insist on a medication review before starting anything new. Simple steps like these prevent thousands of hospitalizations each year.