Opioid Use Disorder Symptom Checker
Physical Dependence Assessment
Physical dependence is a normal biological adaptation to opioids. It's not addiction but causes withdrawal when stopping.
Opioid Use Disorder Assessment
Opioid Use Disorder involves loss of control and negative consequences. The DSM-5 requires 2+ symptoms in 12 months.
Cravings
Loss of Control
Continued Use Despite Harm
Failed Attempts to Cut Down
Spending Significant Time on Opioids
Neglecting Responsibilities
Opioid Use Disorder
Physical Dependence
Important Note: This tool is for educational purposes only. It is not a diagnostic tool. Please consult a healthcare professional for proper assessment and treatment.
Many people think if you take opioids for pain and start feeling sick when you stop, you’re addicted. That’s not true. You might just be physically dependent. And confusing the two can cost people their pain relief, their dignity, or even their lives.
What Physical Dependence Really Means
Physical dependence happens when your body gets used to having a drug in your system. It’s not a choice. It’s biology. If you take opioids daily for more than a week-especially at doses above 30 morphine milligram equivalents (MME) per day-your brain adjusts. It starts making more norepinephrine, changing how your nerves fire, and creating a new normal. When you stop taking the drug, that new normal collapses. Your body goes into overdrive. That’s withdrawal. Symptoms hit fast: nausea in 92% of cases, vomiting in 85%, sweating in 78%, anxiety in 89%. You might yawn nonstop, get diarrhea, or feel like you’re freezing one minute and drenched the next. These aren’t signs of being a bad person. They’re signs your nervous system is recalibrating. The good news? This isn’t permanent. Withdrawal peaks around days 3-5 and fades within 2-4 weeks. It’s uncomfortable, but not life-threatening in most cases. And it doesn’t mean you crave the drug. You just don’t feel right without it.What Addiction Actually Looks Like
Addiction-now called Opioid Use Disorder (OUD)-isn’t about withdrawal. It’s about losing control. It’s when you keep using opioids even when your life falls apart. Someone with OUD might steal money from family to buy pills. They might drive hours to get more, even after losing their job. They’ll keep using despite knowing it’s wrecking their relationships, health, or legal standing. They’ll lie, hide, and isolate. And they’ll still feel a powerful, almost irresistible urge to use-what doctors call craving. Studies show 83% of people with severe OUD report this. Neuroscience shows why. Addiction rewires the brain’s reward system. The dopamine pathway, the part that makes you feel pleasure, gets hijacked. The prefrontal cortex, which helps you make smart choices, weakens. Even after years clean, brain scans show lasting changes. That’s why relapse is so common. The key difference? Someone physically dependent can stop with medical help and go on with their life. Someone with OUD needs more than tapering-they need treatment that addresses the brain’s altered motivation and behavior.Why the Confusion Exists
For decades, doctors used the word “dependence” to mean both physical adaptation and addiction. That changed in 2013 when the DSM-5 dropped “dependence” as a diagnosis. Now, “substance use disorder” is the only clinical term for addiction. But the old language stuck. Patients hear “you’re dependent on opioids” and think, “I’m an addict.” That fear stops people from getting the pain relief they need. A 2020 study found 68% of chronic pain patients on opioids believed withdrawal meant they were addicted. So they quit cold turkey-or worse, they stopped seeing their doctor. And it’s not just patients. Some providers, scared of lawsuits or regulatory scrutiny, cut prescriptions too fast. The CDC’s 2016 opioid guidelines helped reduce overprescribing, but they also led to 44% fewer opioid prescriptions nationwide. That’s good for preventing misuse-but it also pushed many people toward heroin and fentanyl. An estimated 20,000+ overdose deaths from illicit drugs between 2016 and 2020 were linked to this abrupt discontinuation.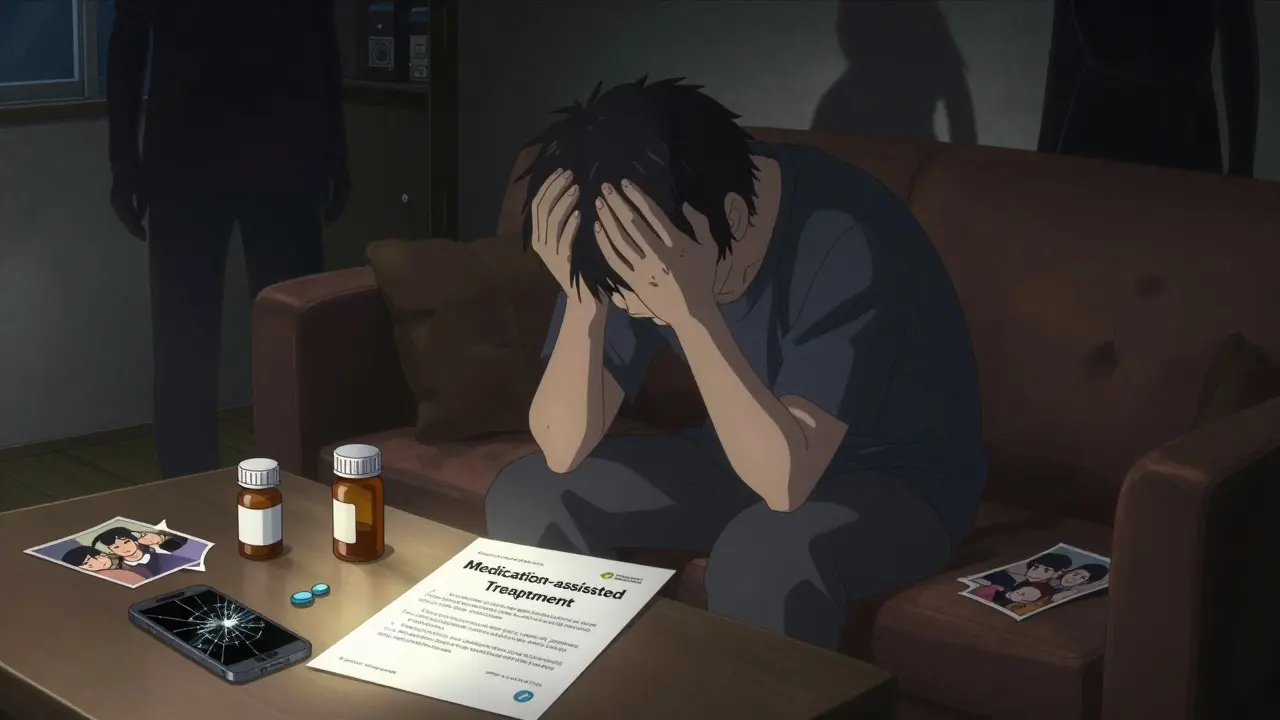
Numbers Don’t Lie
Here’s the hard truth: almost everyone who takes opioids long-term becomes physically dependent. Studies show nearly 100% of patients on daily opioids for 30+ days develop it. But how many become addicted? Only about 8%. That’s from a 2017 study in Pain Medicine. Even among people who misuse prescription opioids, only about 1 in 5 develop OUD. The National Survey on Drug Use and Health in 2017 found 9.9 million Americans misused prescription painkillers. Only 1.7 million met the full criteria for OUD. That means over 8 million people were physically dependent-not addicted. And here’s another stat: if you’re opioid-naïve and take opioids for acute pain-like after surgery-your chance of developing OUD is less than 1%. That’s not zero. But it’s not the epidemic most people think it is.How Doctors Tell the Difference
There’s no blood test. No brain scan you can walk into a clinic for. But there are tools. The Opioid Risk Tool (ORT) helps predict who might be at higher risk for OUD. It looks at family history, past substance use, mental health, and age. About 24% of patients are flagged as high-risk. For diagnosis, doctors use the DSM-5 criteria. You need at least two of eleven symptoms in 12 months:- Craving
- Loss of control over use
- Continuing use despite harm
- Failed attempts to cut down
- Spending a lot of time getting or using the drug
- Neglecting responsibilities
- Giving up hobbies
- Using in dangerous situations
- Tolerance
- Withdrawal
- Needing more to get the same effect
What to Do If You’re Physically Dependent
If you’ve been on opioids for pain and your doctor says it’s time to stop, don’t quit cold turkey. That’s dangerous and unnecessary. The CDC recommends tapering slowly: reduce your dose by 5-10% every 2-4 weeks. If you’re on over 100 MME/day, go slower-5% per month. Use the Clinical Opiate Withdrawal Scale (COWS) to track symptoms. A score above 12 means moderate withdrawal and you might need help. Medications like clonidine or the newer lofexidine (FDA-approved in 2023) can ease withdrawal. They don’t treat addiction. They just make the transition bearable. You’re not failing. You’re managing a normal side effect of treatment.
What to Do If You Have Opioid Use Disorder
If you’re struggling with cravings, lying, stealing, or losing control-this isn’t about willpower. It’s a medical condition. The gold standard is Medication-Assisted Treatment (MAT). Three FDA-approved options:- Buprenorphine: Reduces cravings and withdrawal. Lowers death risk by 70-80%.
- Methadone: Long-acting opioid that stabilizes brain chemistry. Reduces mortality by 50%.
- Naltrexone: Blocks opioids entirely. Best for people already detoxed.





16 Comments
Physical dependence isn't a moral failure-it's a biological fact. Your body adapts. That's it. No judgment. No shame. Just science. And yet, we treat people like criminals for having a nervous system that works too well.
So… you’re telling me I’m not an addict just because I didn’t steal my mom’s jewelry? 😅
Dependence = body says ‘hey’ 🤓 Addiction = soul says ‘I can’t stop’ 🥺💔
I never knew the difference till I saw my cousin go through withdrawal. He wasn’t a bad person-he was just sick. We need more kindness, not more stigma.
Stop conflating dependence with addiction. It’s dangerous. It’s lazy. And it’s killing people who need pain relief. The CDC guidelines were a step forward-but they became a weapon. Fix that.
Typical American medical overreach. We turn every physiological adaptation into a psychiatric disorder. In Canada, we just call it ‘tolerance’ and move on. No drama. No labels. Just medicine.
While I appreciate the intent behind this post, there are several grammatical inconsistencies-particularly around the use of em dashes and serial commas-that undermine its credibility. Also, ‘MME’ should be defined on first use. Still, the core message is valid.
So now we’re giving people a free pass to stay on opioids forever? What’s next? ‘Oh, you’re addicted? That’s just your brain being creative!’ No. Some people are weak. They make bad choices. And they should be held accountable.
One must acknowledge the epistemological framework underpinning the DSM-5’s reclassification of substance-related disorders. The ontological distinction between dependence and addiction reflects a paradigmatic shift in neuropsychiatric taxonomy-a shift that, regrettably, has not yet permeated public consciousness.
I’ve been on opioids for 8 years for fibromyalgia. I don’t crave them. I don’t lie. I don’t steal. But if I skip a dose, I feel like I’ve been hit by a truck. Is that addiction? I don’t think so. But my doctor treats me like I am.
Yessss!! 🙌 Finally someone says it! Dependence ≠ Addiction. And if you’re one of those people who thinks anyone on opioids is a junkie-you need to check your privilege. 🤝❤️
Why are Americans so obsessed with labels? In India we just say ‘medicine helps’ or ‘medicine hurts’. No need for fancy terms like OUD or MME. People just want to feel better.
You say 8% get addicted but what about the other 92% who get hooked on pills because doctors push them? You’re ignoring the real problem-pharma greed. This isn’t biology-it’s capitalism.
my dr just cut me off after 3 yrs and now i’m sweating and shaking and my kid is scared of me… and you want me to just ‘taper’?? like what am i supposed to do?? i cant even get a script anymore and the clinic said ‘you’re not addicted so we dont care’… so now what?? 😭
Some folks think pain is a character flaw. Like if you’re hurting too much, you’re just whiny. But here’s the truth: your body doesn’t lie. And if you’ve been on meds for years and you don’t do drugs for fun-you’re not broken. You’re just human. And you deserve better than being ghosted by your doctor.
And that’s why we need doctors who understand the difference. Not just algorithms. Not just fear. Not just quotas. But real, trained, empathetic humans who see patients-not prescriptions.
Write a comment